Fertility Preservation in Early Endometrial Cancer in Infertile Patients-Case Series
Nihar Ranjan Bhoi
Department of Reproductive Medicine, Indira IVF Hospital Private Limited, Udaipur, India
Published Date: 2024-12-15DOI10.36648/2471-8041.9.12.351
Amol Lunkad1, Aarthi Rajendran1 , Nihar Ranjan Bhoi2*and Vipin Chandra2
1Department of Reproductive Medicine, Indira IVF Hospital Private Limited, Pune, India
2Department of Reproductive Medicine, Indira IVF Hospital Private Limited, Udaipur, India
- *Corresponding Author:
- Nihar Ranjan Bhoi
Department of Reproductive Medicine,
Indira IVF Hospital Private Limited, Udaipur,
India,
E-mail: drniharbhoi@gmail.com
Received date: December 14, 2023, Manuscript No. IPMCRS-23-18206; Editor assigned date: December 18, 2023, PreQC No. IPMCRS-23-18206 (PQ); Reviewed date: January 01, 2024, QC No. IPMCRS-23-18206; Revised date: January 08, 2024, Manuscript No. IPMCRS-23-18206 (R); Published date: January 15, 2024, DOI: 10.36648/2471-8041.9.12.351
Citation: Lunkad A, Rajendran A, Bhoi NR,Chandra V (2023) Fertility Preservation in Early Endometrial Cancer in Infertile Patients–Case Series. Med Case Rep Vol.9 No.12: 351.
Abstract
Background: Endometrial cancer, though often associated with postmenopausal women, affects a notable percentage of premenopausal individuals, with specific risk factors and suitability for conservative management.
Objective: To document incidentally diagnosed early endometrial cancer in infertile women, evaluate their fertility-sparing treatment outcomes, and analyze patient characteristics.
Methods: A retrospective review of cases diagnosed with early endometrial cancer in infertile women was conducted, assessing treatments and outcomes from January 2020 to August 2023.
Results: Among the subjects, the clinical pregnancy rate for endometrial cancer was 0.06%. Most patients (4) were aged 30-40 years, with common comorbidities including diabetes, hypertension, and obesity. The majority (4) were treated at stage FIGO 1A, while a minority necessitated more radical interventions. Three out of five patients positively responded to conservative management with LNG IUD and Tablet medroxyprogesterone acetate for four months, while one required radical hysterectomy due to an advanced cancer stage. One patient remains under surveillance.
Conclusion: Endometrial cancer in infertile women underlines the need for tailored fertility-sparing treatments. Understanding patient demographics, staging and responses to conservative therapies is crucial for effective management and fertility preservation. This study provides insights into the outcomes of such treatments in this specific cohort, emphasizing the importance of personalized care in this context.
Keywords
Endometrial cancer; Premenopausal; Conservative management; Infertile women; Clinical pregnancy rate
Introduction
Endometrial Cancer (EC) ranks as the fifth most prevalent gynecological cancer in developed nations, with a global yearly incidence estimated at 382,069 new cases [1]. In India, it stands as the third most common genital malignancy, following cervix and ovary cancers [2]. Historically, endometrial cancer has been categorized into two clinicopathological types: Type 1 EC, the estrogen-dependent endometrioid type associated with obesity, accounting for up to 85% of cases, and Type 2 EC, encompassing non-endometrioid subtypes like serous cell, clear cell, undifferentiated carcinoma, and malignant mixed Mullerian tumor, also linked with obesity.
The standard treatment for EC involves total hysterectomy and bilateral salpingo-oophorectomy, with or without lymphadenectomy, proving to be effective [3]. However, for patients wishing to preserve their ability to bear children, fertility-sparing approaches have emerged. These methods include endocrine treatments with oral progestins, medroxyprogesterone acetate, gonadotropin-releasing hormone, and more recently, the use of LNG-IUD. Yet, these treatments carry inherent risks of potential ineffectiveness, the chance of relapse, and the possibility of missing diagnoses related to ovarian or lymph node management, or synchronous ovarian cancer [4].
Study setting and duration
The study was conducted at the INDIRA Reproductive Medicine Centre in Pune, spanning from January 2020 to August 2023.
Inclusion criteria for fertility-sparing therapy
• Confirmation of well-differentiated (grade 1) endometrioid adenocarcinoma through Dilation and Curettage (D and C), validated by an expert pathology review.
• Disease confined solely to the endometrium, confirmed by Magnetic Resonance Imaging (MRI) or transvaginal ultrasound.
• Absence of suspicious or metastatic disease observed on imaging modalities.
• Patients without contraindications to medical therapy or pregnancy.
• Mandatory counselling for patients regarding the nonstandard nature of fertility-sparing therapy for endometrial cancer at our reproductive centre.
Data collection and review
• Identification of eligible cases meeting the inclusion criteria from medical records and databases.
• Collection of demographic information, pathology reports, imaging results (MRI, transvaginal ultrasound), and treatment details.
• Review and validation of the collected data by expert clinicians and pathologists to ensure accuracy and consistency.
Treatment approach
• Application of fertility-sparing therapy involving LNG IUD (Levo -norgestrel Intrauterine Device) and Tablet Medroxyprogesterone Acetate (MPA) for a specified duration.
• Regular monitoring of patients’ response to therapy through clinical assessments and imaging studies.
• Surgical intervention for patients not responding adequately to conservative management or demonstrating disease progression.
Statistical analysis
Descriptive statistical analysis of demographic characteristics, treatment outcomes, and patient responses to fertility-sparing therapy. Interpretation and presentation of findings to assess the efficacy and outcomes of the treatment approach.
Case Presentations
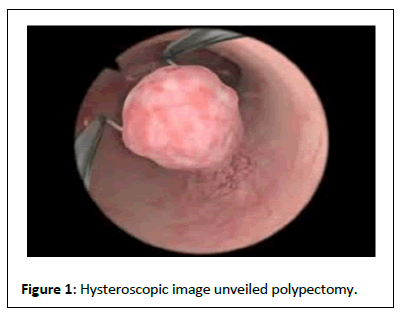
Case 1 was a 35-year-old woman who had been dealing with primary infertility for 14 years and had experienced two previous IVF failures. Her AMH level was 1.32 when she sought further management at our center. Ultrasound revealed an endopolyp of 1.2 × 1 × 0.8 cm in the posterior wall (Figure 1). Opting for a donor cycle, we performed a diagnostic hysteroscopy with polypectomy. The excised tissue was sent for histopathological examination, which unveiled well-differentiated adenocarcinoma with complex hyperplasia and atypia. MRI findings indicated no myometrial invasion or lymph node involvement. Treatment included a combination of Levonorgestrel IUCD and Tablet Medroxyprogesterone acetate 20 mg thrice daily. After four months, a repeated histopathological assessment showed normal results, and we proceeded with our transfer plan. She underwent a fresh transfer of two donor embryos (4AA and 3AA), resulting in the birth of a baby girl at 36 weeks of gestation.
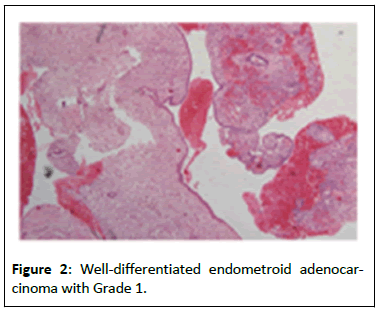
Case 2 was a 38-year-old woman who had experienced primary infertility for 12 years, undergoing four previous IUI failures. She presented with an AMH of 3.32 and an AFC 15. Ultrasound revealed a submucosal fibroid type 2 measuring 1.8 cm × 1.7 cm from the anterior wall, along with anterior wall adenomyosis and a left hemorrhagic cyst. Initially, we decided to cryopreserve embryos using the antagonist cycle, retrieving 8 M2 oocytes, resulting in the formation of 2 good-quality embryos that were cryopreserved. A subsequent hysteroscopic myomectomy revealed well-differentiated endometrioid adenocarcinoma with grade 1 (Figure 2), consistent with MRI findings of no myometrial invasion or lymph node involvement. Treatment comprised levonorgestrel IUCD and Tablet medroxyprogesterone acetate 20 mg thrice daily. After four months, the histopathological assessment showed normal results, and she underwent down regulation with Inj triptorelin 3.6 mg for two months, followed by a successful transfer resulting in a twin pregnancy. However, she was later diagnosed with placenta accreta during the antenatal period, necessitating an obstetric hysterectomy during the caesarean section.
In Case 3, a 33-year-old woman with secondary infertility and a history of a previous abortion came in with an AMH of 3.5 and AFC 13. Ultrasound indicated an endopolyp of 2 × 1.2 × 1 cm in the posterior wall. Embryos were cryopreserved using the antagonist cycle with minimal stimulation protocol, yielding 15 M2 oocytes and forming 6 good-quality embryos. A subsequent hysteroscopic myomectomy revealed well-differentiated endometrioid adenocarcinoma with complex atypia, consistent with MRI findings of no myometrial invasion or lymph node involvement. Treatment involved levonorgestrel IUCD and tablet medroxyprogesterone acetate 20 mg thrice daily. After four months, histopathological reassessment showed normal results, and we proceeded with the transfer of two good-quality embryos. Although her beta Hcg levels were elevated, she experienced a spontaneous abortion.
In Case 4, a 45-year-old woman dealing with primary infertility for 17 years and a known case of hypertension presented with a BMI OF 33.5 and AMH 0.01, AFC 1. Her USG findings suggested endometrial hyperplasia with heterogeneous intrauterine collection indicative of pyometra and possible Ca endometrium with multiple intramural fibroids, along with diminished ovarian reserve. A pipeline biopsy and MRI revealed Squamous cell carcinoma in situ with foci of invasion and poorly differentiated endometrioid cancer. MRI indicated extensive invasion and metastatic involvement, placing her at FIGO 111C. She was recommended for debulking surgery followed by chemoradiotherapy.
Case 5 was a 38-year-old woman with primary infertility for 12 years and diminished ovarian reserve (AMH 0.71). Initial ultrasound indicated features of Adenomyosis and thickened endometrium. We opted for ovarian regeneration followed by an antagonist protocol, retrieving 7 M2 oocytes and forming 3 blastocysts, which were cryopreserved. A diagnostic hysteroscopy and biopsy revealed focal hyperplasia without atypia. MRI indicated an ill-defined lesion along the posterior and right anterolateral wall of the uterus, showing signs of potential neoplasia or focal adenomyosis. She's currently undergoing treatment with LNG IUD along with tablet medroxyprogesterone acetate 20 mg thrice daily.
Results and Discussion
After conducting 6863 ET cycles at our reproductive center, pregnancies were successfully conceived via the IVF ET procedure. The overall conception rate reported was 72.5%. However, in this particular case study focusing on endometrial cancer cases from January 2020 to July 2023, the clinical pregnancy rate was notably lower at 0.06%.
In this case study 4 patients are between the age 30-40 years old and 1 is found to be above 40 years age. With the help of improved diagnostic modalities and increased awareness among patients, we were able to find Ca endometrium at an early stage and an earlier age. As gynecologic malignancy often affects women who are still in reproductive years and women who are postponing childbearing, the incidence of cancer in those who still want to get pregnant has somewhat increased.
In this case study we found 4 patients diagnosed with Ca endometrium had primary infertility due to continuous estrogen exposure maybe a cause. One of the patients had secondary infertility.
In this case, we found 1 patient was found to be diabetic, 2 of patients were found to be hypertensive and 2 of the patients were found to be obese.
All 4 patients had undergone treatment under stage Figo IA except 1 of the patients IIIC who had to undergo debulking surgery followed by chemoradiotherapy. We found 3 of the patients responded well to conservative management with combined treatment of LNG IUD AND tablet medroxyprogesterone acetate 20 mg three times daily for months and 1 patient had to undergo radical hysterectomy because of the advanced stage of cancer. LNG-IUS is superior to oral progestin in endometrial hyperplasia [5]. The pooled regression rates 1)-Simple hyperplasia 89% oral progestins vs. 96% LNG-IUS. 2) Complex hyperplasia LNG-IUS vs. oral progestins (92% vs. 66%). Atypical endometrial hyperplasia (90 vs. 69%, respectively). 96% of patients with endometrial hyperplasia had complete regression within the first year of LNGIUS use. Best treatment option for post-menopausal women with atypical hyperplasia, for any women who do not respond to progestin treatment, is a total hysterectomy.
There are many documented trials [6] registered in ClinicalTrials.gov using higher doses of MPA(500 mg daily), monotherapy, or along with LNG-IUS.
According to a recent meta-analysis [6], treatment with progestins alone or in combination with LNG-IUD for patients with EC/atypical hyperplasia can yield a good complete response rate. However, the outcomes regarding pregnancy might be less favourable when treated with LNG IUD alone.
In another meta-analysis focusing on the utilization of LNG IUD along with Gnrh agonists, 75.5% of patients achieved a complete response. Among these patients, 34 were prepared for pregnancy, and 20 successfully conceived (13 through ART and 7 naturally) [7].
Additionally, a study combining Megestrol Acetate (MA), Tamoxifen, and Gnrh agonists found that 89% of patients achieved complete remission after therapy with this hormone combination. Furthermore, 45% of these patients conceived after treatment.
Another study concentrated on the efficacy of surgically resecting the diseased endometrium followed by commencing oral progestins five days after the procedure, continuing for a total of 6 months. After this treatment, 65% of the patients were able to conceive [3].
Several studies examined [1-3] hysteroscopic resection followed by LNG IUD. They found a recurrence rate of 7%, with 78% achieving a complete response. Moreover, 45% of participants were able to conceive after 12 months of this treatment.
Conclusion
Young women with endometrial cancer who aim to preserve fertility need tailored counselling and conservative treatments. The combined application of progestins and LNG IUD shows promising outcomes, especially for early-stage cases, aiding both in treatment and fertility preservation. Opting for operative hysteroscopy as the primary sampling method is recommended due to its correlation with higher remission rates. While guidelines for managing younger patients conservatively are essential, they should always complement rather than replace individualized care. Each patient possesses unique characteristics, needs, and expectations that warrant a personalized approach to care and management.
Ethical Considerations
Compliance with ethical guidelines and obtaining necessary approvals for conducting retrospective studies and using patient data. Ensuring patient confidentiality and anonymity by using de-identified information in the analysis and reporting.
References
- Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, et al. (2019) Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 144: 1941-1953.
[Crossref], [Google Scholar], [Indexed]
- Setiawan VW, Yang HP, Pike MC, McCann SE, Yu H, et al. (2013) Type I and II endometrial cancers: Have they different risk factors? J Clin Oncol 31: 2607–18.
[Crossref], [Google Scholar], [Indexed]
- Shobeiri MJ, Gharabaghi PM, Esmaeili H, Ouladsahebmadarek E, Mehrzad-Sadagiani M (2013) Fertility sparing treatment in young patients with early endometrial adenocarcinoma. Pak J Med Sci 29: 651-655.
[Crossref], [Google Scholar], [Indexed]
- Falcone F, Laurelli G, Losito S, Di Napoli M, Granata V, et al. (2017) Fertility preserving treatment with hysteroscopic resection followed by progestin therapy in young women with early endometrial cancer. J Gynecol Oncol 28: e2.
[Crossref], [Google Scholar], [Indexed]
- Terzic M, Norton M, Terzic S, Bapayeva G, Aimagambetova G (2020) Fertility preservation in endometrial cancer patients: Options, challenges and perspectives. Ecancermedicalscience 14: 1030.
[Crossref], [Google Scholar], [Indexed]
- Wei J, Zhang W, Feng L, Gao W (2017) Comparison of fertility-sparing treatments in patients with early endometrial cancer and atypical complex hyperplasia: A meta-analysis and systematic review. Medicine 96: e8034.
[Crossref], [Google Scholar], [Indexed]
- Maggiore ULR, Khamisy-Farah R, Bragazzi NL, Bogani G, Martinelli F, et al. (2021) Fertility-sparing treatment of patients with endometrial cancer: A review of the literature. J Clin Med 10: 4784.
[Crossref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences