Tissue Defect Repair over the Achilles Tendon: Which Flap and which Graft?
Halbony H, Ceviz M, Dincgözoğlu A and Bekerecioglu M*
Department of Plastic Reconstructive Aesthetic Surgery and Wound Care, Kahramanmaras Sutcu Imam University, Onikişubat, Turkey
- *Corresponding Author:
- Bekerecioglu MDepartment of Plastic Reconstructive Aesthetic Surgery and Wound Care, Kahramanmaras Sutcu Imam University, Onikişubat, Turkey, E-mail: halacoolglow@yahoo.com
Received date: May 2, 2022, Manuscript No. IPMCRS-22-13585; Editor Assigned date: May 3, 2022, PreQC No. IPMCRS-22-13585 (PQ); Reviewed date: May 18, 2022, QC No. IPMCRS-22-13585; Revised date: May 24, 2022, Manuscript No. IPMCRS-22-13585 (R); Published date: June 1, 2022, DOI: 10.36648/2471-8041.8.6.231
Citation: Halbony H, Ceviz M, Dincgözoğlu A, Bekerecioglu M (2022) Tissue Defect Repair over the Achilles Tendon: Which Flap and which Graft? Med Case Rep Vol.8 No.6: 231.
Abstract
One of the most challenging areas of urgency to reconstruct lower extremity injuries are soft tissue injuries over the Achillis tendon, where successful defect reconstruction must provide coverage that allows gliding and a cushioning that allows forces of ambulation. However thin enough to permit wearing of normal footwear. A local or regional Flaps combination of tendon substitutes with free muscular or fasciocutaneous flaps and free cutaneous flaps with tendon been described for the reconstruction have of complex defects. However even microsurgical repairs are associated with up to 20% range of complications requiring additional operative interventions.
Five cases of moderate -major defects of the soft tissue overlying the Achillis tendon are presented all of which were ambulant patients with expectations of a normal life who were referred to Kahramanmaras Sutcu Imam University Hospital for surgical intervention.
Keywords
Achilles tendon; Soft tissue Defect; Flap; Graft
Introduction
One of the most challenging areas of urgency to reconstruct lower extremity injuries are soft tissue injuries over the Achillis tendon. Where successful defect reconstruction must provide coverage that allows gliding and a cushioning that allows forces of ambulation. However thin enough to permit wearing of normal footwear [1].
Five cases of moderate-major defects of the soft tissue overlying the Achillis tendon are presented all of which were ambulant patients with expectations of a normal life who were referred to Kahramanmaras Sutcu Imam University Hospital for surgical intervention.
Case 1
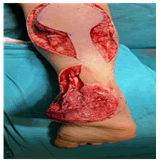
An 18-year-old female patient’s ankle was casted by orthopedics for partial rupture of the Achilles tendon as a result of a motorcycle accident. Soft tissue necrosis occurred due to the compression of the cast (Figure 1). Tissue biopsy culture was negative for any colonization. After the debridement of necrotic tissues of the patient who was referred to our clinic, she was followed up with instillation NPWT. When adequate and healthy granulation tissue has covered on the Achilles tendon, the defect was closed with a full-thickness skin graft taken from the inguinal region (Figure 2).
Case 2
A 10-year-old girl patient suffered a full Achilles tendon rupture after falling from a bicycle was casted by orthopedics. The patient who developed tissue necrosis after the splint/cast was referred to our clinic (Figure 3). Tissue biopsy culture revealed Pseudomonas putida colonization and accordingly antibiotic treatment has been initiated. After adequate debridement of the necrotic tissue and appropriate wound care, the Achilles tendon area was primarily repaired by orthopedics and the tissue defect was closed with a reverse flow sural flap (Figures 4 and 5). 6 months postoperatively debulking operation was performed to allow the patient to be able to wear suitable footwear with respect to her age.
Case 3
A 12-year-old girl with partial Achilles tendon rupture, calcaneal bone fracture and overlying soft tissue injury after a gunshot wound. Tissue biopsy culture revealed acinetobacter baumanni, accordingly antibiotic treatment has been initiated. After the orthopedic intervention (Figure 6), after sufficient necrotic tissue debridement the tissue defect was repaired with a surgically delayed reverse flow sural flap applied after referral of the patient to our clinic for soft tissue defect closure (Figure 7).
Case 4
A 40-year-old male patient with an isolated tissue defect on the Achilles tendon after a gunshot injury (Figure 8). Tissue biopsy culture was negative for any colonization. The wound was followed up with NPWT and serial approximation sutures to decrease wound tension. After appropriate wound preparation required for skin grafting (14 days later), closure was achieved with a full-thickness skin graft (Figure 9).
Case 5
A 35-year-old male patient with tissue defect overlying the Achilles tendon, posterior tibia and fibula fractures and accompanying soft tissue necrosis after a gunshot injury. Tissue biopsy culture revealed Citrobacter farmeri and Enterobacter clocae colonization, accordingly antibiotic treatment has been initiated. Soft tissue necroses were debrided (Figure 10). The resulting defect was followed with NPWT and serial approximation sutures to decrease wound tension. After adequate wound preparation, tissue defect repair was performed with a surgically delayed reverse flow sural flap.
All patients were referred to physical therapy following tissue defect repair.
Results and Discussion
Achilles tendon is both the largest and the strongest tendon in the body, capable of transmitting forces of up to 12.5 times body weight while running [2]. Achilles tendon injury is one of the three most common tendon injuries with the highest incidence in males in their third or fourth decades [3].
Pasterior heel soft tissue defects may occur as a result trauma, post-operative, or as a result of microanjiopathy secondary to peripheral vasculer disease, drug induced, Diabetes mellitus, or other medical conditions [3,4].
The reconstructive aims include providing a length maintaining durable tendon reconstruction which can withstand mechanical end Shear forces allowing for powerful plantar flexion and dosiflexion of the ankle joint [2,5]. Moreover, providing vascularized soft tissue that will address a contour defect, protect the underlying tendon reconstruction [1]. Nevertheless, providing durable skin coverage which is thin enough to permit normal footwear.
For Achilles tendon and the overlying tissue defect reconstruction many techniques have been advocated. Minor or partial ruptures may be skin grafted following adequate debridement hemostasis and a course of hyperbaric oxygen therapy or NPWT which stabilizes the wound environment, decreases wound oedema/bacterial load, improves tissue perfusion and stimulate granulation tissue and angiogenesis [6]. The gold standard treatment for moderate to large defects is the anteriolateral thigh flap with vascularized fascia lata [7]. A Local or regional flaps combination of tendon substitutes with free muscular or fasciocutaneous flaps and free cutaneous flaps with tendon been described for the reconstruction have of complex defects. However even microsurgical repairs are associated with up to 20% range of complications requiring additional operative interventions [8-10].
Conclusion
Coexisting Achilles tendon and overlying soft tissue defect is of great surgical challenge. To evaluate the optimal algorithm for reconstruction of composite soft tissue and Achilles tendon defects further research is needed while taking into consideration donor site scaring, and the need for secondary flap contouring and fat debulking procedures, resulting in the prolongation of the rehabilitation process and hence ambulation.
References
- Dobke M, Suliman A, Mackert GA, Herrera FA, Singer R, et al. (2016) Single-stage reconstruction of Achilles tendon and overlying tissue with the extended temporoparietal fasciagaleal flap--23-year follow-up and the review of the literature. Ann Plast Surg 76: 165-70.
[Cross Ref], [Google Scholar], [Indexed]
- Chalmers R, Tare M, Niranjan N (2010) Vascularised Achilles tendon graft reconstruction--by the tendon for the tendon. J Plast Reconstr Aesthet Surg 63: 273-6.
[Cross Ref], [Google Scholar], [Indexed]
- Iorio ML, Han KD, Evans KK, Attinger CE (2015) Combined Achilles tendon and soft tissue defects: functional outcomes of free tissue transfers and tendon vascularization. Ann Plast Surg 74: 121-5.
[Cross Ref], [Google Scholar], [Indexed]
- Prasetyono TOH, Sisca F (2019) Achilles tendon reconstruction with a half-width Achilles graft and wrap-around fascial flap. Arch Plast Surg 46: 267-271.
[Cross Ref], [Google Scholar], [Indexed]
- Denis E, Paul IH, Andreas S, Franz L, Milomir N, et al. (2019) The anterolateral thigh flap for Achilles tendon reconstruction: Functional outcomes. Plast Reconstr Surg 143: 1772-1783.
[Cross Ref], [Google Scholar], [Indexed]
- Agarwal P, Kukrele R, Sharma D (2019) Vacuum assisted closure (VAC)/negative pressure wound therapy (NPWT) for difficult wounds: A review. J Clin Orthop Trauma 10: 845-848.
[Cross Ref], [Google Scholar], [Indexed]
- Andreu-Sola V, Aguilera-Sáez J, Rivas-Nicolls D, Bosacoma Roura P, Barret JP (2017) Functional reconstruction of acutely burnt achilles tendon with composite anterolateral thigh flap with fascia lata: A case report. Ann Burns Fire Disasters 30: 309-312.
[Cross Ref], [Google Scholar], [Indexed]
- Grishkevich VM (2014) Proximally based sural adipose-cutaneous/scar flap in elimination of ulcerous scar soft-tissue defect over the achilles tendon and posterior heel region: a new approach. J Burn Care Res 35: e143-50.
[Cross Ref], [Google Scholar], [Indexed]
- Altinkaya A, Yazar S, Bengur FB (2021) Reconstruction of soft tissue defects around the Achilles region with distally based extended peroneal artery perforator flap. Injury 52: 1985-1992.
[Cross Ref], [Google Scholar], [Indexed]
- Innocenti M, Innocenti A, Ghezzi S, Delcroix L (2017) Achilles region soft-tissue defects: A reconstructive algorithm based on a series of 46 cases. J Reconstr Microsurg 33: S40-S47.
[Cross Ref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences