The Bobath Concept Case Series Report
Klaus Gusowski*, Flavious Vorovenci and Peter Flachenecker
Department of Physiotherapy, Neurological Rehabilitation Center Quellenhof, Bad Wildbad, Germany
- *Corresponding Author:
- Klaus Gusowski
Department of Physiotherapy,
Neurological Rehabilitation Center Quellenhof, Bad Wildbad,
Germany,
E-mail: Klaus.gusowski@sana.de
Received date: November 23, 2022, Manuscript No.IPMCRS-22-15231; Editor assigned date: November 25, 2022, PreQC No.IPMCRS-22-15231 (PQ); Reviewed date: December 06, 2022, QC No.IPMCRS-22-15231; Revised date: December 16, 2022; Manuscript No. IPMCRS-22-15231(R); Published date: December 23, 2022, DOI: 10.36648/2471-8041.8.12.252
Citation: Gusowski K, Vorovenci F, Flachenecker P (2022) The Bobath Concept Case Series Report. Med Case Rep Vol.8 No.12:252.
Abstract
The Bobath Concept is worldwide known to be one of the best concepts to assess and treat people with neurological disorders. It has an inclusive approach and may be used for various diagnoses and disorders of the central nervous system [1]. Despite the lack of scientific evidence, longstanding experiences gathered with this concept and its positive effects on patients make it a useful tool for neurological patients.
This paper tries to close the gap between clinical experience and evidence. According to the “Model of Bobath Clinical Practice”, six patients with different diagnoses and symptoms underwent the clinical reasoning process in an inpatient rehabilitation center. Four patients suffered from Multiple Sclerosis (MS) Relapsing Remitting MS (RRMS), Primary Progressive MS (PPMS) and Secondary Progressive MS (SPMS) and two from ischemic stroke basal ganglia and brainstem infarction. Their age varied between 29 and 78 years. The Barthel-Index ranged from 25 to 90 points, and the Expanded Disability Status Scale (EDSS) of MS patients was between 5.5 and 7.5. Standardized assessments encompassed the 10 Meter Walking Test (10 MWT), Performance Orientated Mobility Measure (POMA/Tinetti), Action Research Arm Test (ARAT), 5 Times Sit to Stand (5 STS), Timed Monopedal Stance (TMS) and Goal Attainment Scaling (GAS). Depending on the diagnosis and treatment goal, two of these assessments plus GAS were chosen and conducted before the treatment, i.e. on day 2 (T1) and at day 8 (T2) of the bobath course. The included patients received care as usual during the rehabilitation process. All therapists formulated a goal orientated treatment hypothesis. Every patient received six treatment units over eight days, all under the supervision of a Bobath instructor. There were no dropouts.
Keywords
Bobath concept; Physiotherapy; Treatment; Assessment; Model of Bobath clinical practice
Introduction
Dr. Berta and Dr. Karel Bobath developed the concept that now bears their name in order to treat patients with neurological disorders. It is worldwide spread and is inclusive, that means there is no patient exclusion due to diagnosis, severity of symptoms or disability status.
In many neurological rehabilitation settings, either physiotherapist or occupational therapists, have the option to work with different concepts. Among these are Vojta, Akrodynamic or Proprioceptive Neuromuscular Facilitation (PNF), as well as treatment with devices such as treadmill, with or without body weight support and/or balance trainer, sport therapy, computer assisted devices for activities of arm and hand, virtual reality devices and many more. All these different treatments modalities positively influence the outcome of the rehabilitation process [2]. In such a multidisciplinary setting with different treatment options, it is difficult to disentangle the effect of one single treatment approach. Due to the lack of scientific evidence, the Bobath concept is often overlooked or only poorly recommended in the guidelines for stroke [3] and multiple sclerosis [4], or even totally excluded from reviews. As a consequence, there is an uncertainty among therapists and rehabilitation physicians about the value of this therapeutically approach and whether it may still represent a reliable treatment method. The positive and measurable effects that were obtained by the therapists when working with the patients are to some extent in strong contrast with the recommendations of the guidelines [5].
This case series report aimed at delineating the effects of a six days treatment in the framework of the second part of the basic Bobath course. The effects are measurable at the level of activity and participation and very relevant regarding activities of daily living. We seized this opportunity in a course setting to isolate the treatment according to the bobath concept and investigate the results of this approach.
Patients and Method
The Bobath basic course, conceived and recommended by the “International Bobath Instructor Training Association” (IBITA), comprises a minimum of 150 hrs of theory and practice. It leads to enlargement of basic knowledge of the bobath concept and extend the understanding of the underlying neurophysiology and neuroanatomy. The course curriculum includes the full range of important components of modern neurological rehabilitation [6]. In these courses, patients are treated only according to the Bobath concept. Over the last 16 years, measurement tools for gathering the results of treatments are part of the course content. The course was split into two parts over eight days. Six patients (Table 1) who served as probands to the participants of the second part of a Bobath basic course at the Neurological Rehabilitation Center Quellenhof were studied.
| Patient | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Sex | m | f | f | f | m | m |
| Age | 46 | 43 | 29 | 78 | 65 | 54 |
| Diagnosis | PPMS | PPMS | RRMS | stroke, basal ganglia | pontine infarction | PPMS |
| Disease duration | 7 years | 11 years | 8 years | 1 years | 1 month | 8 years |
| EDSS | 5.5 | 7 | 7.5 | - | - | 6 |
| Barthel Index | 85 | 75 | 60 | 60 | 25 | 90 |
| male/female (m/f) Primary Progressive Multiple Sclerosis (PPMS) Relapsing Remitting Multiple Sclerosis (RRMS) Expanded Disability Status Scale (EDSS) |
||||||
Table 1: Demographic data.
These were a heterogenic group of patients with different diagnoses, different age and different degrees of disabilities severity. Moreover, Persons with Multiple Sclerosis (PwMS) showed various degrees of fatigue.
All patients were asked about their treatment goals. These goals have been determined according to the “International Classification of Functioning, Disability and Health” (ICF) on the level of activity and/or participation as practical and verifiable as far as possible. The goals were filled in the “Goal Attainment Scale (GAS)” [7,8]. The current state of the patients was scored with “-1”, the expected outcome with “0”. The worsened state was scored as “-2”. The other scale levels were completed, setting the outcome somewhat more than expected at “+1” and much more than expected at “+2”.
Additionally to the GAS, the course participants conducted two other assessments representing the change to the individual goals. Because of the diversity of the diagnoses and goals, different international assessments were taken into consideration such as:
• 10 Meter Walking Test (10 MWT)[9,10]
• 10 Meter Walking Test-steps (10 MWT st)
• 10 Meter Walking Test–seconds(10 MWT sec)
• Performance Orientated Mobility Assessment (POMA/Tinetti) [11,12]
• Timed Get Up and Go, seconds (TGUG)[9,13]
• Single Leg Stance right/left, seconds (SLS r/l)
• 5 Times Sit To Stance, seconds (5 STS)[9,14]
• Action Research Arm Test, points (ARAT) [15]
• Goal Attainment Scale (GAS)[9,10]
The “Barthel Index” (BI) was gathered for all patients, whereas the “Expanded Disability Status Scale” (EDSS) [16] was only obtained in PwMS (Persons with Multiple Sclerosis).
On the first day of treatment, the course participants investigated the impairments of their patients regarding the activities of daily living and rated the movement performance and compensatory patterns and capacity according to the “Model of Bobath Clinical Practice” (MBCP). Together with their patients, the physiotherapists who participated in the course formulated SMART (Specific, Measurable, Achievable, Relevant, Time-bound) treatment goals [17] and filled them into the GAS. With the help of the clinical reasoning process, the movement diagnosis was determined and the treatment hypothesis and treatment plan were formulated. The physiotherapeutic units were 60 min of bobath therapy per session. The first assessment (T1) took place before the first session of treatment, and the second assessment before the last treatment. All the therapeutic sessions were strictly supervised by an experienced Bobath instructor.
Results
Patient 1
A 46 years old male diagnosed with primary progressive multiple sclerosis for about 7 years. EDSS 5.5 points, BI 85 points.
Primary goal: Gait improvement to prevent falls.
Movement analysis/Movement diagnosis: Hypotonia of hip and knee flexors and the ventral trunk muscles. Balance was negatively affected by poor control of the foot movements with a dominance of plantar flexors and supinators, combined with weakness of foot and toe dorsal flexors and pronators in the right lower extremity.
Assessments: 10 MWT, TGUG.
Therapeut c approach: Strengthening of the weak muscles in different positions to increase body function level, followed by transfer into waking activity.
Results: The muscle tone was objectively increased and therefore, walking ability improved. The assessments (10 MWT, TGUG) improved, whereas BI remained unchanged (Table 2).
| 10 MWT st T0 | 10 MWT st T1 |
|---|---|
| 20 | 18 |
| 10 MWT sec T0 | 10 MWT sec T1 |
| 13 | 10.5 |
| TUG T0 | TUG T1 |
| 12.1 | 11.2 |
Table 2: Results patient 1: Comparison T0 vs T1, 10 MWT st (10 Meter Walking Test–steps); 10 MWT sec (10 Meter Walking Test–seconds); TGUG; TUG (Timed Get Up and Go, seconds).
Patient 2
A 43 years old female diagnosed with progressive MS for about 11 years, EDSS 7.0 points, BI 75 points. At admission, she was unable to walk. At the first assessment after 11 days, she could walk a small distance with a wheeled walker, but was still very unsecure, with a high risk of falling.
Primary goal: She wanted to achieve her independence and to do the housekeeping free from walking aids (e.g. to make the beds).
Movement analysis/Movement diagnosis: Accentuated hypertensions of the left trunk and of the left leg were documented.
The patient showed great difficulties maintaining balance in stance due to a spasticity of the distal lower limb.
Assessments: 10 MWT, POMA.
Therapeutic approach: To build up core stability, increase the tone of the left hip flexors and integrate both components in standing and walking.
Results: The results were more than expected (GAS +2). The patient was able to stand very secure and improved her walking capacity and endurance, with a strikingly reduced risk of falling. BI increased by 5 points (Table 3).
| POMA T0 | POMA T1 |
|---|---|
| 10 | 13 |
| 10 MWT St T0 | 10 MWT St T1 |
| 30 | 26 |
| 10 MWT sec T0 | 10 MWT sec T1 |
| 37 | 27 |
Table 3: Results patient 2: Comparison T0 vs T1, Performance Orientated Mobility Assessment, (POMA/Tinetti); 10 MWT st (10 Meter Walking Test–steps); 10 MWT sec (10 Meter Walking Test–seconds).
Patient 3
A 29 years old female with relapsing remitting multiple sclerosis, EDSS 7.5, BI 60 points. The last relapse was 8 weeks ago.
Primary goal: Due to the short treatment period, the primary goal formulated by the patients seemed not to be realistic: Walking long distances with her dog (about 2-3 km) as it was possible before the relapse.
Movement analysis/Movement diagnosis: Severe ataxia of the extremities (left arm and both legs), asymmetric tone of the trunk with a shift of the thorax to the left, extremely supinated left foot in stance. She was able to walk only 5 m with a walker and the help of a caregiver.
Assessments: 10 MWT, POMA.
Therapeutic approach: Intensive training of core stability. To increase the muscle tone of abdominal wall and reclaim symmetry, to increase the tone of lower limb muscles to reduce the ataxia and thereby to increase the control of foot pronation in stance phase.
Results: The walking ability increased significantly. As a consequence, the risk of falls was reduced. BI increased by 5 points (Table 4). The effects on the GAS do not represent the real gain due to the unrealistic goal formulation.
| 10 MWT St T0 | 10 MWT St T1 |
|---|---|
| 20 | 18 |
| 10 MWT sec T0 | 10 MWT sec T1 |
| 23.5 | 13.1 |
| POMA T0 | POMA T1 |
| 19 | 24 |
Table 4: Results patient 3: Comparison T0 vs T1, POMA/Tinetti (Performance Orientated Mobility Assessment), 10 MWT st (10 Meter Walking Test–steps); 10 MWT sec (10 Meter Walking Test-seconds).
Patient 4
A female patient, 78 years old, suffering from multiple diagnoses, second stroke at the level of basal ganglia, older stroke in internal capsule and in the cerebellum, progressive multifocal leukoencephalopathy, surgery of lumbar spinal stenosis L3/4 one year before. The residual hemiplegia resulted in a high risk of falling with repeated falls in the last few months, BI 90 points.
Primary goals: To reduce the risk of falls, to increase the walking distance and to regained walking without aid.
Movement analysis/Movement diagnosis: The patient was able to walk with a walker. She showed reduced core stability and weakness of the right knee and hip extensors with shortening of the hamstrings. The selective foot movement was reduced to dorsiflexion and pronation. By walking, in mid swing, no foot clearance was found, which the cause of multiple falls was. The knee extension in terminal swing was absent.
Assessments: 5 STS, POMA.
Therapeutic approach: The focus was on increasing the muscle tone of the hip flexors and promoting the knee flexion during initial swing. That was achieved among other activities by climbing the stairs.
Results: The risk of falls was decreased. Foot clearance remained a problem but less frequently. The aim to walk without walking aid was not fulfilled, BI increased by 5 points (Table 5).
| POMA T0 | POMA T1 |
|---|---|
| 19 | 24 |
| 5 STS T0 | 5 STS T1 |
| 28.5 | 28 |
Table 5: Results Patient 4: Comparison T0 vs T1, POMA (Performance Orientated Mobility Assessment), 5 STS (Five Times Sit to Stance, seconds).
Patient 5
A 65 years old male, suffering from left paramedian pons infarction four weeks prior to intervention. A hemiplegic left arm with reduced muscle tone of the right leg but with preserved sensitivity was documented. Standing and walking were not possible.
Movement analysis/Movement diagnosis: Poor balance, due to proximal hypotonia especially in the hip flexors, abductors and extensors was observed. Right trunk weakness with a tendency to fall to the right during standing and walking was seen. Due to an unstable scapula, arm and hand function were severely reduced.
Primary goal: Improvement of standing and gait, reduction of the risk of falls, and to regain arm and hand function for obtaining activities of daily living.
Assessments: SLS, ARAT.
Therapeutic approach: It was very challenging to combine the impaired balance with the functional training of arm and hand. Therefore, it was necessary to split the focus between the balance disturbances and the hand function in every treatment. We changed the environment as often as possible, and used different positions and combined them with specific tasks of daily living. First, we choose to train the postural orientation, followed by training of balance and fine motor skills, and eventually tried to restore gross motor activity.
Results: The two therapists helped the patient by improving the locomotion and fine motor skills. The problem-orientated approach of the bobath concept became visible. Activities of daily living improved, BI increased by 10 points (Table 6).
| ARAT T0 | ARAT T1 |
|---|---|
| 19 | 27 |
| SLS r sec T0 | SLS r sec T1 |
| 0 | 1 |
| SLS l sec T0 | SLS l sec T1 |
| 5 | 9 |
Table 6: Results patient 5: Comparison T0 vs T1, ARAT (Action Research Arm Test, points); SLS r/l (Single Leg Stance right/left seconds).
Patient 6
A 48 years old male suffering from primary progressive multiple sclerosis that was diagnosed 8 years before. The symptoms were spastic hemiplegia with limitation of walking distance, and reduction of left arm and hand function. Over the years, walking distance and endurance decreased and the risk of falls increased. Arm and hand activity worsened gradually and led to impaired function. A wheeled walker was needed, BI 75 points.
Movement analysis/Movement diagnosis: Hypotonia of the trunk muscles and of the proximally lower limb, especially in the hip flexors, were seen. Severe hypertonia was present in the plantar flexors and supinators. This abnormal muscle tone influenced the anticipatory postural adjustments for balance and reduced the maximal walking distance to 150 m. Because of the decreased muscle tone, the scapula could not be stabilized on the thorax, resulting in a reduction of arm function. The intrinsic hand muscles were also weak.
Primary goals: To improve balance and therefore reduce the risk of falls. To restore arm function and to improve fine motor skills.
Assessments: POMA, ARAT.
Therapeutic approach: It was important to improve fine motor skills with and for daily activities and to build up the stability of the scapula for a better arm function. Therefore, the therapists worked on the level of body function to improve the stability of the scapula, e.g. in prone. They also used daily activities in combination with postural activities to improve the balance. The lower limb was involved in selective training to improve proximal function and as a result, a reduced spasticity of the foot.
Results: The complex symptomatology improved in terms of postural adjustment and selective motor skills. Ability to walk and fine motors skills of the hand improved as well. BI remained unchanged (Table 7).
| POMA T0 | POMA T1 |
|---|---|
| 21 | 26 |
| ARAT T0 | ARAT T1 |
| 22 | 32 |
Table 7: Results patient 6, POMA/Tinetti (Performance Orientated Mobility Assessment, points); ARAT (Action Research Arm Test, points).
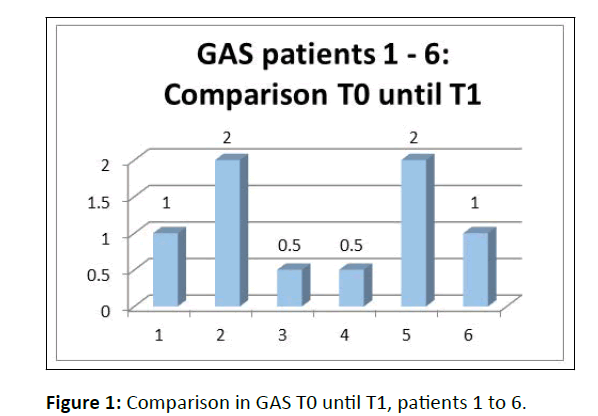
In summary, four out of our six patients achieved the expected goals, or the outcomes were more than expected according to the GAS. The remaining two showed also an improvement and approached their goals (Figure 1).
The changes in GAS corresponded to the changes in Barthel Index. In line with the treatment goals, standardized assessments were conducted in order to corroborate the results of the GAS. In this regard, the patient performances were clinically significant, and mean values improved as follows: 10 MWT sec: -30%, 10 MWT steps -11%, POMA +25%, ARAT +30%.
Discussion
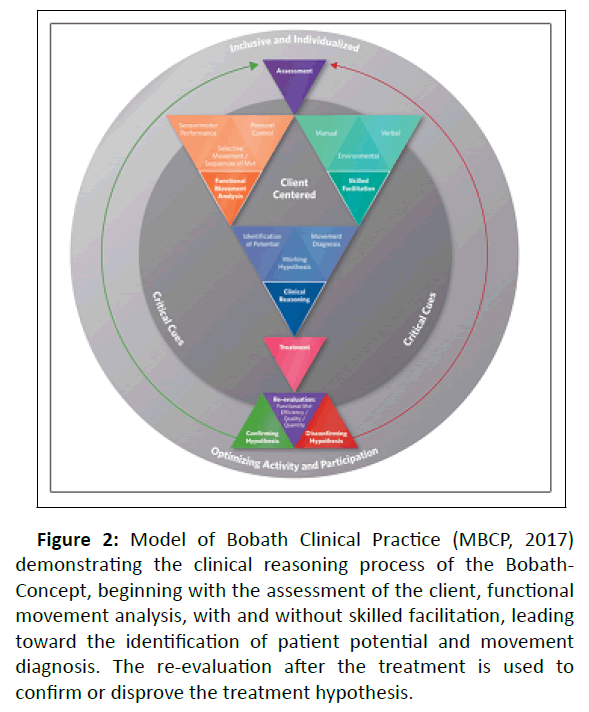
The Bobath concept defines itself as “inclusive” and used to treat different diagnoses and problems in the field of neurology. A clinical reasoning process is required, as explained in the “Model of Bobath Clinical Practice” (Figure 2) which was developed by the research committee of the “International Bobath Instructor Training Association (IBITA)..
Figure 2: Model of Bobath Clinical Practice (MBCP, 2017) demonstrating the clinical reasoning process of the Bobath- Concept, beginning with the assessment of the client, functional movement analysis, with and without skilled facilitation, leading toward the identification of patient potential and movement diagnosis. The re-evaluation after the treatment is used to confirm or disprove the treatment hypothesis.
This model is now part of the Bobath basic courses and used for assessment and treatment of neurological disorders in adults [1]. Within the process of goal definition, patients and therapists share the same responsibility for the therapy and try to specify it accordingly on the level of activity and/or participation (ICF). The capacity, defined as the highest probable level of functioning, of the given activity is to be observed under several conditions. Due to the wide range of symptoms commonly observed in disorders of the Central Nervous System (CNS) it is reasonable firstly to define various goals and to follow them accordingly to their importance for daily living or even simultaneously if possible. The performance of every activity can be influenced with verbal input, manual facilitation or changes of the environment. The Bobath therapists are able to observe the selective movements and the postural background for balance necessary to conduct any specific task. The capacity has to be analyzed, and identified “critical cues” lead to the recognition of the potential and resources of the patient but may also help to formulate a movement diagnosis.
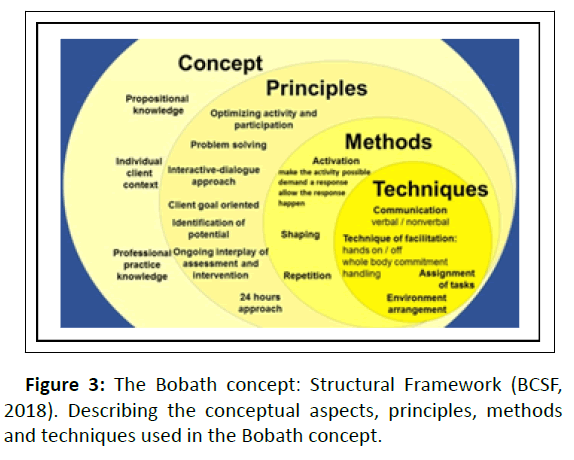
As a consequence, a resource orientated treatment a hypothesis is formulated, which will be permanently proofed during and after the treatment in an attempt to confirm or disconfirm the initial hypotheses. It forces the therapists to reevaluate their process of clinical reasoning. This procedure ensures that treatment and tasks will be permanently adapted to the actual performance and capacity of the patient [18]. In addition, the Bobath Concept Structural Framework (BCSF) as developed by Eckardt et al., [19] and shown in Figure 3 could be used to derive techniques for treatment.
In this case series report, the MBCP and BCSF was illustrated in six patients with various diagnoses, age, and sex, duration of disease, neurological symptoms and resilience. These patients underwent an individual clinical reasoning process as explained above with regard to the patient’s expectations on their basic life skills (level of activity and participation according to the ICF). The goals were determined in advance according to the SMART rule (Specific, Measurable, Achievable, Relevant, Time-bound), with the Goal Attainment Scale, with predefined outcomes “expected”, “more than expected” and “much more than expected”. Treatments were conducted exclusively according to the Bobath concept with techniques taught in the Bobath basic course under supervision of the Bobath instructor.
The contemporary Bobath Concept provides an up to date theoretical and practical knowledge and enables the physiotherapists and occupational therapists to work effectively and goal-oriented. All patients showed a clinically relevant improvement with regard to the assessments, measured on day 2 and day 8, particularly on 10 MWT (mean difference seconds: -30%, steps: -11%), POMA (mean difference: +25%) and ARAT (mean difference: +30%).
This treatment approach is further supported by Jones TA 2017 [20]. Her study demonstrates that training of compensation may inhibit the recovery of neuronal circuits and thus disable patients to exploit their full potential. Therefore, the quality of movement is an important focus in the treatment of neurological patients. The treatment results in the Bobath course verify this approach. In goal determination and in treatments, the best possible “normal” posture and selective movement patterns are tried to achieve individually. Compensatory mechanisms for posture and movement are not supported in an attempt not to interfere with the relearning process of normal neuronal circuits in the CNS.
Conclusion
Due to the different goals and patterns of impairment, the GAS was chosen as a measure to compare the different outcomes of treatment. When administering it to our patients, it was found to be a challenging task to precisely formulate the individual goals. In this regard, the concept of the ICF was helpful for the exact classification of daily activities and participation. Nevertheless, the goal of patient 3 was so broadly defined that it was unreachable within the five treatment sessions however, its analysis was a helpful experience for the course participants.
One of the arguments against the Bobath concept is that it may be in some way “old fashioned”. To counteract this argument, IBITA implemented the two models “Model of Bobath Clinical Practice” and “Bobath Concept Structural Framework” in order to further develop this concept and adapt it to the needs of the patients. Therefore, the Bobath concept nowadays does not simply reflect what Berta and Karel Bobath discovered more than 70 years ago, but is extended, continuously improved and useful to teach students modern neurorehabilitation science.
References
- Michielsen M, Vaughan-Graham J, Holland A, Magri A, Suzuki M (2019) The Bobath Concept-A model to illustrate clinical practice. Disabil Rehabil 41: 2080-2092.
[Crossref], [Google Scholar], [Indexed]
- Gusowski K (2014) Physiotherapie bei multipler sklerose-konventionelle und moderne Verfahren. Neurol Rehabil 20: 239-245.
- Dohle C, Tholen R, Wittenberg H, Saal S, Quintern J, et al. (2015) S2e-leitlinie: Rehabilitation der Mobilitat nach Schlaganfall (ReMoS). Neurol Rehabil 21: 179-184.
[Crossref]
- Hemmer B, Berthele A (2021) S2k-leitlinie diagnose und therapie der multiplen sklerose, neuromyelitis optica spektrum und mog-igg-assoziierte erkrankungen. DG Neurologie 4: 251–275.
[Crossref], [Google Scholar]
- Brock K, Haase G, Rothacher G, Cotton S (2011) Does physiotherapy based on the Bobath Concept, in conjunction with a task practice, achieve greater improvement in walking ability in people with stroke compared to physiotherapy focused on structured task practice alone?: A pilot randomized controlled trial. Clin Rehabil 25: 903-12.
[Crossref], [Google Scholar], [Indexed]
- Hengelmolen-Greb A (2016) Bobath concept review of the teaching content of Bobath basic courses: Does the curriculum contain evidence-based measures?. Physio Sci 12: 17-25.
[Crossref], [Google Scholar], [Indexed]
- Kiresuk TJ, Sherman RE (1968) Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Ment Health J 4: 443-53.
[Crossref], [Google Scholar], [Indexed]
- Turner-Stokes L (2010) Goal Attainment Scaling (GAS) in rehabilitation: A practical guide. Clin Rehabil 23: 362-70.
[Crossref], [Google Scholar], [Indexed]
- Baert I, Smedal T, Kalron A, Rasova K, Heric-Mansrud A, et al.(2018) Responsiveness and meaningful improvement of mobility measures following MS rehabilitation. Neurology 91: e1880-e1892.
[Crossref], [Google Scholar], [Indexed]
- Gijbels D, Dalgas U, Romberg A, Groot V, Bethoux F, et al. (2012) Which walking capacity tests to use in multiple sclerosis? A multicentre study providing the basis for a core set. Mult Scler 18: 364-371.
[Crossref], [Google Scholar], [Indexed]
- Canbek J, Fulk G, Nof Ls, Echternach J (2013) Test-retest reliability and construct validity of the tinetti performance-oriented mobility assessment in people with stroke. J Neurol Phys Ther 37: 14-19.
[Crossref], [Google Scholar], [Indexed]
- Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34: 119-26.
[Crossref], [Google Scholar], [Indexed]
- Podsiadlo D, Richardson S (1991) The timed "Up and Go": A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39: 142-8.
[Crossref], [Google Scholar], [Indexed]
- Buatois S, Miljkovic D, Manckoundia P, Gueguen R, Miget P, et al. (2008) Five times sit to stand test is a predictor of recurrent falls in healthy communityâ?ÂÂÃÂliving subjects aged 65 and older. J Am Geriatr Soc 56: 1575â?ÂÂÃÂ1577.
[Crossref], [Google Scholar], [Indexed]
- Lyle RC (1981) A performance test for assessment of upper limb function in physical rehabilitation treatment and research. Int J Rehabil Res 4: 483-92.
[Crossref], [Google Scholar], [Indexed]
- Meyer-Moock S, Feng YS, Maeurer M, Dippel FW, Kohlmann T (2014) Systematic literature review and validity evaluation of the Expanded Disability Status Scale (EDSS) and the Multiple Sclerosis Functional Composite (MSFC) in patients with multiple sclerosis. BMC Neurol 14: 58.
[Crossref], [Google Scholar], [Indexed]
- The Bobath Concept-A model to illustrate clinical practice
- Woldag H, Stupka K, Hummelsheim H (2010) Repetitive training of complex hand and arm movements with shaping is beneficial for motor improvement in patients after stroke. J Rehabil Med 42: 582-7.
[Crossref], [Google Scholar], [Indexed]
- Eckhardt G, Brock K, Hasse G, Puschnerus C, Hengelmolen-Greb A, et al. (2018) Bobath Concept Structural Framework (BCSF): Positioning partial aspects within a holistic therapeutic concept. Am J Health Res 6: 79-85.
[Crossref], [Google Scholar]
- Jones TA (2017) Motor compensation and its effects on neural reorganization after stroke. Nat Rev Neurosci 18: 267-280.
[Crossref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences