Abstract
The Bobath Concept Case Series Report
The Bobath Concept is worldwide known to be one of the best concepts to assess and treat people with neurological disorders. It has an inclusive approach and may be used for various diagnoses and disorders of the central nervous system [1]. Despite the lack of scientific evidence, longstanding experiences gathered with this concept and its positive effects on patients make it a useful tool for neurological patients.
This paper tries to close the gap between clinical experience and evidence. According to the “Model of Bobath Clinical Practice”, six patients with different diagnoses and symptoms underwent the clinical reasoning process in an inpatient rehabilitation center. Four patients suffered from Multiple Sclerosis (MS) Relapsing Remitting MS (RRMS), Primary Progressive MS (PPMS) and Secondary Progressive MS (SPMS) and two from ischemic stroke basal ganglia and brainstem infarction. Their age varied between 29 and 78 years. The Barthel-Index ranged from 25 to 90 points, and the Expanded Disability Status Scale (EDSS) of MS patients was between 5.5 and 7.5. Standardized assessments encompassed the 10 Meter Walking Test (10 MWT), Performance Orientated Mobility Measure (POMA/Tinetti), Action Research Arm Test (ARAT), 5 Times Sit to Stand (5 STS), Timed Monopedal Stance (TMS) and Goal Attainment Scaling (GAS). Depending on the diagnosis and treatment goal, two of these assessments plus GAS were chosen and conducted before the treatment, i.e. on day 2 (T1) and at day 8 (T2) of the bobath course. The included patients received care as usual during the rehabilitation process. All therapists formulated a goal orientated treatment hypothesis. Every patient received six treatment units over eight days, all under the supervision of a Bobath instructor. There were no dropouts.
Author(s): Klaus Gusowski*, Flavious Vorovenci and Peter Flachenecker
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 241
Medical Case Reports received 241 citations as per google scholar report
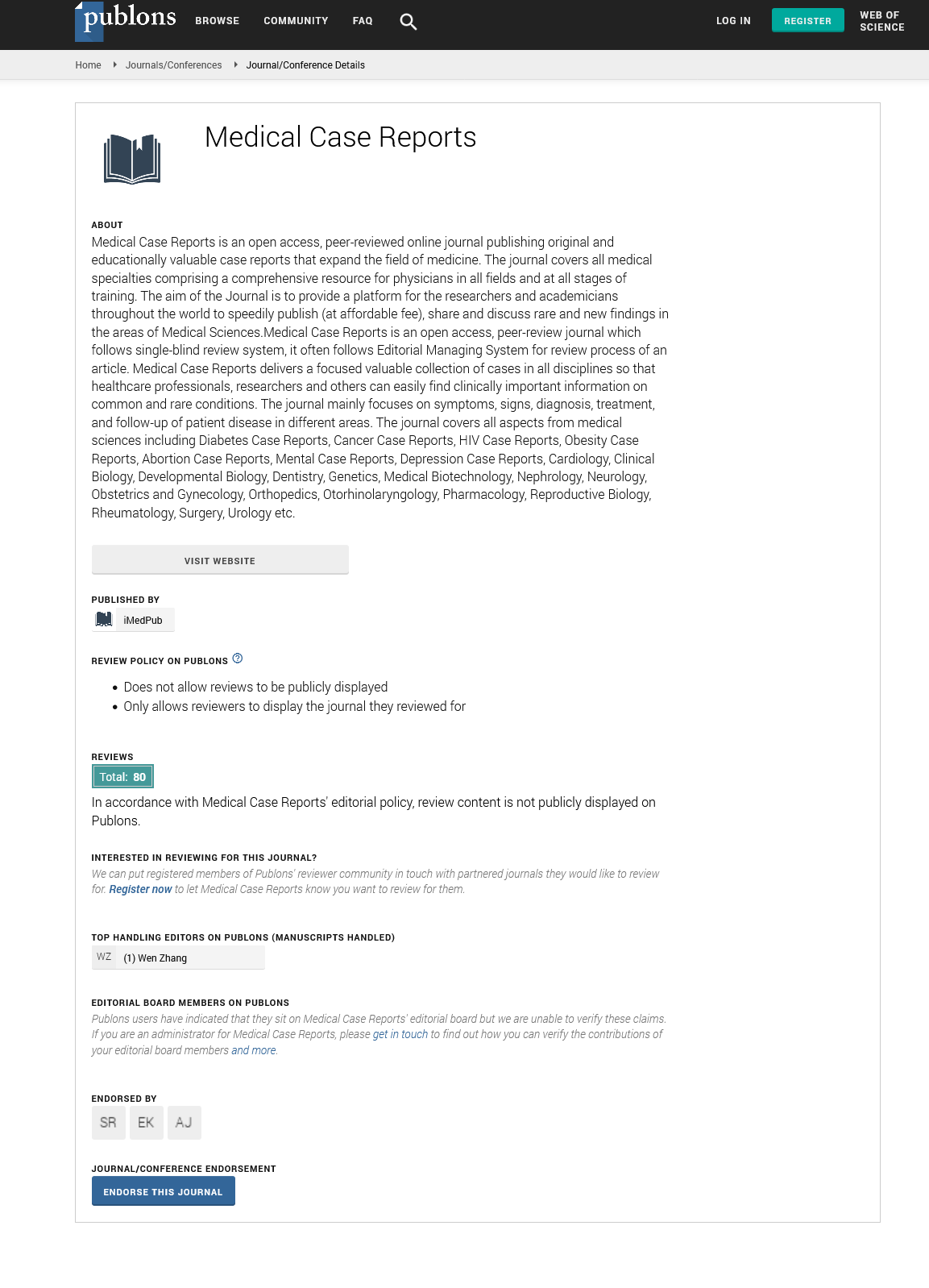
Medical Case Reports peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Cosmos IF
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Secret Search Engine Labs
- Euro Pub
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences