Severe Hypertrophic Cardiomyopathy: Septal Ablation with Coated Stent - A Case Report and Literature Review
Juan David Rojas*, Mateo Guzmán, Diego Ardila and Arnold Méndez-Toro
1Department of Internal Medicine, Hospital Universitario Nacional, Universidad Nacional de Colombia, Bogotá DC, Colombia
2Department of Hemodynamics, Hospital Universitario Nacional, Bogotá DC, Colombia
3Department of Cardiology, Hospital Universitario Nacional, Bogotá DC, Colombia
- *Corresponding Author:
- Juan David Rojas
Hospital Universitario Nacional de Colombia
Calle 44 #59-75, Bogotá DC, Colombia
Tel: +3017014967
E-mail: jurojasp@unal.edu.co
Received Date: February 16, 2020; Accepted Date: March 03, 2020; Published Date: March 10, 2020
Citation: Rojas JD, Guzmán M, Ardila D, Méndez-Toro A (2020) Severe Hypertrophic Cardiomyopathy: Septal Ablation with Coated Stent - A Case Report and Literature Review. Med Case Rep Vol.6 No.1: 133.
DOI: 10.36648/2471-8041.6.1.133
Abstract
Background: Hypertrophic cardiomyopathy (HMC) is a genetic pathology of cardiovascular origin cataloged as the leading cause of sudden death in young adults. Its genotypic and phenotypic presentation is diverse. 10% clinically identified of which 40% are asymptomatic. The first line therapy is the pharmacological one; in the absence of response, it is usually indicated to perform septal myectomy or alcohol septal ablation.
Case summary: Here, we describe the case of a 59-year-old woman, black, with an unclear history of cardiomyopathy, arterial hypertension of difficult management and atrial fibrillation (AF), who presented angina, high blood pressure, electrocardiographic abnormalities and elevation of cardiac biomarkers suggesting a non-ST elevated myocardial infarction (NSTEMI). This is an unusual case in which septal ablation was performed with a medicated stent as a treatment for severe HMC in a patient with paroxysmal AF without significant obstruction in coronary arteries.
Discussion: Only 10% of patients with HCM are clinically identified, 60% of these being symptomatic. Its presentation includes symptoms associated to congestive heart failure, chest pain and arrhythmias. The first-choice therapy is medical. When it fails, next step is septal reduction therapy either open or percutaneous intervention. Concerning the latter, non-alcoholic ablation with septal embolization (micro coils, polyvinyl alcohol, cyanoacrylate) has recently been proposed as an alternative; septal stent ablation is not recommended given the need for dual antiplatelet and the expected recurrence rate. In selected patients, septal stent ablation arises as an alternative to conventional management.
Keywords
Hypertrophic obstructive; Cardiomyopathy; Ablation technique; Stent; Septal myectomy
Introduction
Hypertrophic cardiomyopathy (HCM) is a genetic pathology defined by the presence of left ventricular hypertrophy (wall thickness of 15 mm or greater) in the absence of both secondary etiologies and dilatation of the cardiac cavity [1-3]. In the last 10 years, the number of alcohol septal ablations (ASA) exceeds the number of septal myectomies performed in 50 years; in HCM specialized centers, myectomy-ASA rate oscillates between 5:1 to 20:14. New technologies for nonalcohol septal occlusion, including septal embolization (micro coils, polyvinyl alcohol and cyanoacrylate) have recently been proposed as an alternative [3-5]. Here, a selected case is described in which the septal ablation with stent implant was used for HCM treatment.
Timeline
Below Table 1 explains the timeline of the study.
Table 1: Timeline of the studies.
| Early 2018 | Coronary angiography with no evidence of significant lesions |
| Early 2018 | Stable progressive angina; paroxysmal atrial fibrillation diagnosed |
| June 2019 | NSTEMI diagnosed |
| June 18th, 2019 | Transthoracic echocardiogram with severe hypertrophic obstructive cardiomyopathy |
| June 19th, 2019 | Cardiac magnetic resonance imaging (MRI) showing apical involvement |
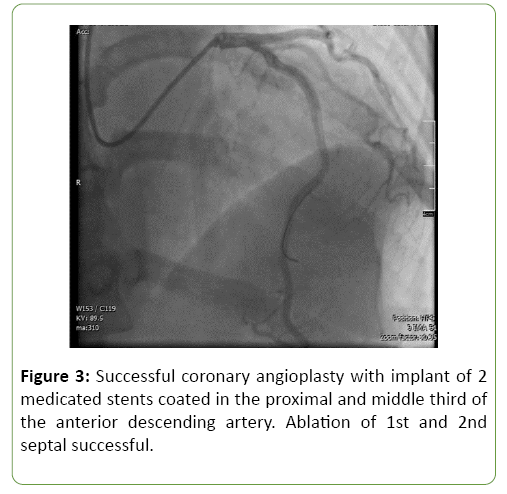
| July 3rd, 2019 | Successful coronary angioplasty with implant of 2 medicated STENTs in proximal and middle thirds of the anterior descending artery |
Case Report
A 59-year-old, Black race, female patient who lives in Bogota DC, with an unclear history of sudden death in a male relative, has been diagnosed with hypertension, non-valvular paroxysmal atrial fibrillation, and apparent dilated cardiomyopathy, currently on direct oral anticoagulants.
During June 2019, she presents a progressive worsening of effort dyspnea and multiple chest pain episodes, poorly indepth description, which auto-resolve. The day before admission she presents an acute chest pain characterized as oppressive, of moderate to severe intensity, irradiated to both upper extremities, associated with palpitations, without mitigating or aggravating, during home rest without previous physical or emotional stress factors, which It does not improve the administration of oral nitrates.
At admission, blood pressure is 204/120 mmHg, with no other abnormal findings on physical examination; an EKG is taken (normal axis, sinus rhythm, HR 62 bpm, findings suggest severe left ventricular hypertrophy with ST segment depression in lateral derivations, related to volume overload) and positive troponin; thus, oriented as a NSTEMI vs. hypertensive emergency with the heart as a target organ vs. acute aortic syndrome (less likely given pain characteristics). Intravenous anti-hypertensive management (labetalol and nitrates) is established, with decrease in symptomatology. She is then referred to our institution.
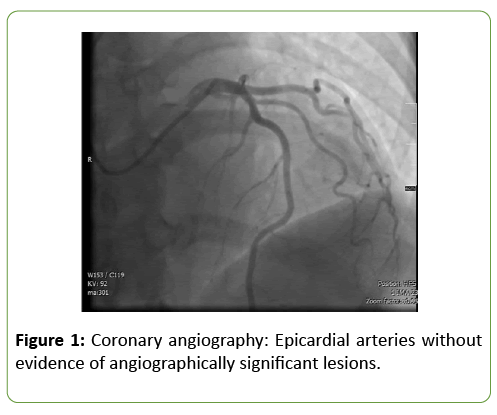
Initial diagnosis is NSTEMI; a transthoracic echocardiogram demonstrates left ventricle estimated ejection fraction of 45%, mild diffuse hypokinesia and severe hypertrophic myocardiopathy conditioning a left ventricular outflow tract obstruction (LVOTO) (gradient of 53 mmHg), with no evidence of systolic anterior motion of the mitral valve. She is sent to hemodynamics department, where a coronary angiography is performed, with no evidence of significant lesions; septal arteries are evidenced with a large diameter (Figure 1). Treatment possibilities include alcohol septal ablation vs. STENT placement in septal arteries due to their diameter. The cardiovascular surgery service does not consider her a candidate for management surgical given absence of mitral valve involvement.
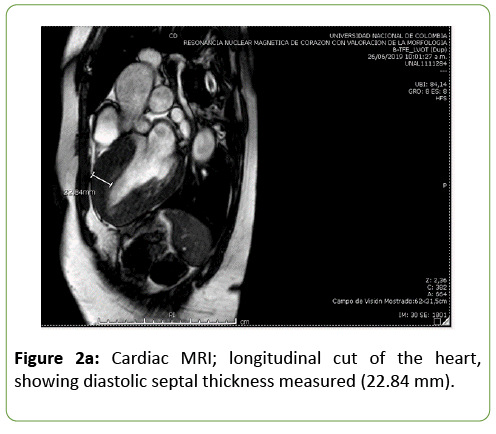
The institutional cardiology group examines the patient given persistence of chest pain with minimal effort, requirement of beta blocker at maximum doses and use of 4 antihypertensive drugs (including aldosterone receptor antagonist) used with no satisfactory blood pressure control. It is decided to perform contrasted cardiac MRI to shed light towards hypertrophy phenotype (and plan an intervention) (Figure 2a).
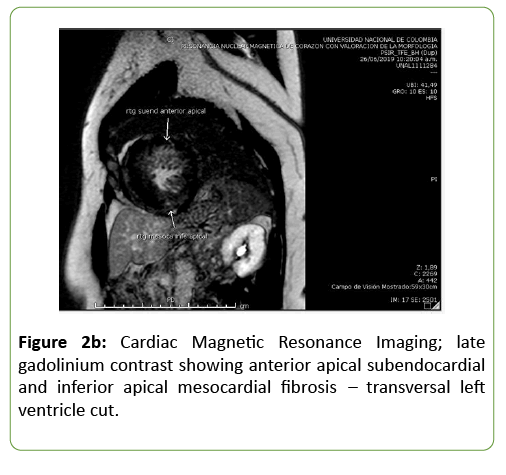
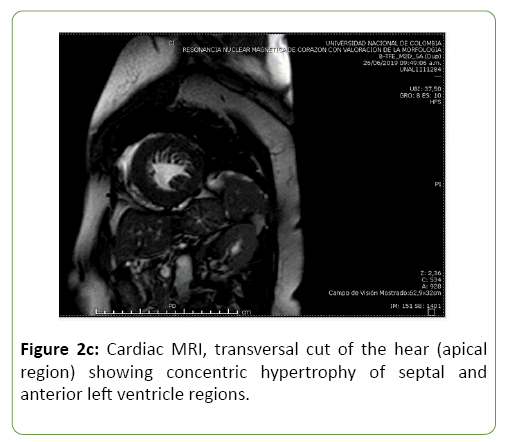
Cardiac MRI is performed on June 19th, 2019, revealing asymmetric concentric hypertrophy cardiomyopathy with predominant septum involvement in basal, middle and apical cavities, with subendocardial and myocardial late enhancement, associated to mild to moderate LVOTO due to septal basal hypertrophy, with no systolic anterior motion of the mitral valve (Figures 2b and 2c). This, in addition to prior findings, leads to the decision of performing a septal stent ablation.
First and second septal arteries ablation is successful, with placement of two STENTs in descending anterior artery (proximal and middle thirds) (Figure 3); the peak gradient decreased from 80 to 50 mmHg. After the procedure, the patient presented a new episode of chest pain, nausea and high blood pressure levels. She is monitored in intermediate care during 48 hours with resolution and no recurrence of symptoms. Finally, she is assessed by the electrophysiology department, who consider the patient is not a candidate for implantable cardioverter-defibrillator for primary prevention, given a risk of sudden death estimated at 5 years at 1.63% (according to HCM Risk SCD36). The patient presents a satisfactory recovery, with no further recurrences, and so, she is discharged with cardiac rehabilitation, anticoagulation (rivaroxaban) and dual antiplatelet therapy (clopidogrel 75 mg and Acetylsalicylic Acid 100 mg daily).
Discussion
Hypertrophic cardiomyopathy is a genetic pathology defined by the presence of left ventricular hypertrophy (wall thickness of 15 mm or greater) in absence of secondary aetiologies and dilatation of the cardiac cavity [1-3]. HCM is the first identifiable cause of sudden death in young adults [4-7]. It is estimated 20 million people worldwide suffer from this condition; 10% clinically identified, of which 40% are asymptomatic [8].
This is pathology with etiology and heterogeneous phenotypic presentation secondary to various morphologies of left ventricular hypertrophy that condition specific anatomical and hemodynamic patterns. The degree of hypertrophy is associated with the risk of sudden death, but not with the development of heart failure [9]. A majority of patients present with an asymmetric septal hypertrophy and diastolic dysfunction with a preserved ejection fraction [7], and therefore, patients with HCM can present LVOTO, diastolic dysfunction, myocardial ischemia, and/or mitral insufficiency [10].
Symptoms can be classified into three large groups: associated with heart failure, chest pain, and arrhythmias that increase in frequency with age. Approximately 10% of patients progress to left ventricular dilation and systolic disfunction [11]. When assessed, our patient ’ s clinical presentation suggested myocardial ischemia associated to the imaging of severe LVOTO and diastolic dysfunction. Only 6% of patients with HCM have EKG findings within normative parameters related to lower obstructive gradient, absence of left ventricular hypertrophy and better cardiovascular prognosis prognosis [12]. In this patient, abnormal findings include ST segment depression in basal EKG, which has been related to an odds ratio of 20 for sudden death or implantable cardioverterdefibrillator requirement [13].
Diagnostic workup includes a transthoracic echocardiography (TTE) evidencing morphology, systolic and diastolic function, presence or absence of mitral insufficiency (and its stage), and LVOTO gradient [3,10]; however, it’s an operator-dependent tool, limited to acoustic window is limited by the low lateral resolution of ultrasound [2]. In specific phenotypes, like apical hypertrophy, TTE can be insufficient [14]. Our case did not present mitral valvular dysfunction, which is why we didn’t consider septal myectomy.
Although Doppler echocardiography is the mainstay for the diagnosis of LVOTO [15], cardiac MRI better characterizes the myocardium and through late gadolinium uptake, it allows the identification of areas of fibrosis defined strongly as an independent predictor of mortality [16]. Cardiac MRI was used identifying areas of hypertrophy at the apical level without mitral valve alteration that allowed evaluating therapeutic approach and prognostic decision.
90% of patients with heart failure in the context of HCM have LVOTO; once they are symptomatic, the treatment of choice is pharmacological [3,17]. The annual mortality associated with heart failure due to HCM is 0.5% (20 times less than heart failure secondary to aetiologies, other than ischemic) [18]. The scientific evidence is mainly from observational and retrospective studies, and better outcomes are associated to beta-blockers of non-dihydropyridine calcium-channel blockers [3,17]. In this patient, despite using beta-blocker therapy at maximum doses, chest pain recurred with no association to physical exertion in a pathology where the use of venodilators and arterial vasodilators can worsen the symptomatology [3].
In patients who have an unsatisfactory symptom control despite pharmacologic therapy (specifically those classified as NYHA III-IV) and LVOTO gradient greater than 50 mmHg at rest and/or with provocation, invasive treatment options can be considered. These include septal myectomy and, in some cases, alcohol septal ablation (ASA) [3]. It is not encouraged to perform invasive procedures in asymptomatic patients [3]. In the history of interventional therapy for HCM, there have been multiple comparisons to determine the best management. Final decision is, however, heavily influenced by individual case approach, prioritizing the presence or absence of mitral valvular pathology.
According to the European Cardiology Society, by extrapolation, a minimum activity requirement for the performance of ASA and septal myectomy includes 10 annual procedures for interventional cardiologists and cardiovascular surgeons respectively [3]. In the last 10 years, the number of ASA exceeds the number of myectomies performed in 50 years, probably facilitated by the emergence of interventional cardiology; in specialized centers in HCM, the myectomy-ASA rate oscillates between 5:1 to 20:14.
In our center, septal myectomy is considered the gold standard of management for persistently symptomatic patients despite maximum medical therapy, given the 90-95% of probability for a complete long-lasting symptom management, with low rate of adverse events associated with the surgical procedure [18]. Mortality associated with the procedure relies heavily on the experience of the surgeon and the surgical centers, which could limit access to effective therapy in low-income settings or experience-lacking institutions [19]. Determinants of surgical success include age below 50, male gender, absence of post-procedure atrial fibrillation and a left atrial diameter lesser than 46 mm [20]. Risks associated with the procedure include iatrogenic ventricular septal defect, need for cardiac pacemaker due to AV block and aortic insufficiency whose frequency depends on the center, estimating that 8% of patients require reintervention and 14% use of pacemakers. The estimated survival is 90% equal to that of the general population [21].
In myectomy non-candidates, either due to comorbidities or age, therapy of choice is ASA, whose purpose is to produce a transmural infarct at the basal septal ventricular level, lowering the intraventricular gradient [22]. The healing process can lead to AV block and/or facilitate arrhythmogenic processes [18]. Benefits include being a less invasive method, and, thus, shorter hospital stay [23]. In high-volume patient centers, the mortality rate is close to 1% and long-term survival may match that of myectomy [24]. Among its disadvantages, ASA is associated with potential transmural infarctions with a probable increase in the rate of arrhythmia and sudden death in susceptible patients, confined and dependent on the inflexible anatomical distribution of the septal perforator artery [4].
Given the absence of mitral valve involvement, the possibility of septal myectomy in our patient was ruled out, opting as therapeutic measure for ASA. Prior to performing the ablation, it is necessary to exclude coronary artery disease and define the septal artery to be intervened however, our patient documented not only the absence of angiographically significant lesions, but the presence of two septal arteries with large dependent myocardial mass (Figure 1).
We still lack studies concerning additional procedures to those mentioned; non-alcohol ablation and septal embolization (microcoils, polyvinyl alcohol and cyanoacrylate) has been recently proposed as an alternative [3,5]. On the other hand, septal stent ablation has been in a few scenarios where the approach for septal alcohol ablation is technically not feasible [25,26]. However, it has been relegated over the years given the high recurrence rate due to the appearance of collateral circulation and the need to use dual antiplatelet therapy to support stent permeability [27]. In other cases, it has been used after the ASA failure and the concurrent presence of significant coronary artery disease with marked and sustained improvement at one year of LVOTO [28], with no recurrence of collateral circulation. Regarding this last case, it was probably related to previous myocardial fibrosis secondary to alcohol ablation.
Due to the described comorbidities of the patient, with paroxysmal AF and without coronary artery lesions significant, the suppression of the surgical option and combined with angiographic assessment prior it was decided to perform septal stent ablation without immediate complication.
Conclusion
HCM is a genetic pathology of cardiovascular origin listed as the leading cause of sudden death in young adults. Its genotypic and phenotypic presentation is diverse. Early identification through genomic and imaging screening leads to a decrease in the sudden death rate. The implementation of cardiac MRI widens the sensitivity for diagnosis with respect to the TTE and allows estimating the risk of adverse outcomes. In those persistently symptomatic patients, despite the maximum medical therapy, an open or percutaneous intervention is performed. In the latter, non-alcoholic ablation with septal embolization (microcoils, polyclinic alcohol, cyanoacrylate) has recently been proposed as an alternative. In selected patients, septal stent ablation arises as an alternative to conventional management.
Informed Consent
The authors confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of Interest
None declared.
References
- Maron BJ (2002) Hypertrophic cardiomyopathy: A systematic review. JAMA 287:1308-1320.
- Veselka J, Anavekar NS, Charron P (2017) Hypertrophic obstructive cardiomyopathy. Lancet, London, England, UK. 389:1253-1267.
- Elliott PM, Anastasakis A, Borger MA, Borggrefe M (2014) Task Force members: 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). European Heart Journal 35(39):2733-2779.
- Maron BJ, Nishimura RA (2014) Surgical septal myectomy versus alcohol septal ablation. Circulation 130:1617-1624.
- Asil S, Kaya B, Canpolat U, Yorgun H, Şahiner L, et al. (2018) Septal reduction therapy using nonalcohol agent in hypertrophic obstructive cardiomyopathy: Single center experience. Catheter Cardiovasc Interv 92:557-565.
- O’Mahony C, Jichi F, Ommen SR, Christiaans I, Arbustini E, et al. (2018) International external validation study of the 2014 European society of cardiology guidelines on sudden cardiac death prevention in hypertrophic cardiomyopathy (EVIDENCE-HCM). Circulation Lippincott Williams and Wilkins 137:1015-1023.
- Semsarian C, Ingles J, Maron MS, Maron BJ (2015) New perspectives on the prevalence of hypertrophic cardiomyopathy. J Am Coll Cardiol 2015;65:1249-1254.
- Maron BJ (2018) Clinical course and management of hypertrophic cardiomyopathy. Longo DL, ed. N Engl J Med Massachusetts Medical Society; 2018;379:655-668.
- Spirito P, Bellone P, Harris KM, Bernabò P, Bruzzi P, et al. (2000) Magnitude of left ventricular hypertrophy and risk of sudden death in hypertrophic cardiomyopathy. N Engl J Med 342:1778-1785.
- Maron BJ, Maron MS (2016) The remarkable 50 Years of Imaging in HCM and How it Has Changed Diagnosis and Management. JACC Cardiovasc Imaging 2016;9:858–872.
- Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, et al. (2007) Classification of the cardiomyopathies: a position statement from the european society of cardiology working group on myocardial and pericardial diseases. Eur Heart J 29:270–276.
- McLeod CJ, Ackerman MJ, Nishimura RA, Tajik AJ, Gersh BJ, et al. (2009) Outcome of Patients With Hypertrophic Cardiomyopathy and a Normal Electrocardiogram. J Am Coll Cardiol 54:229–233.
- Haghjoo M, Mohammadzadeh S, Taherpour M, Faghfurian B, Fazelifar AF, et al. (2009) ST-segment depression as a risk factor in hypertrophic cardiomyopathy. Europace 11:643-649.
- Moon JCC, Fisher NG, McKenna WJ, Pennell DJ (2004) Detection of apical hypertrophic cardiomyopathy by cardiovascular magnetic resonance in patients with non-diagnostic echocardiography. Heart 90:645-649.
- Steel KE, Kwong RY (2008) Application of cardiac magnetic resonance imaging in cardiomyopathy. Curr Heart Fail Rep NIH Public Access 5:128.
- Chan RH, Maron BJ, Olivotto I, Pencina MJ, Assenza GE, et al. (2014) Prognostic value of quantitative contrast-enhanced cardiovascular magnetic resonance for the evaluation of sudden death risk in patients with hypertrophic cardiomyopathy. Circulation 130:484-495.
- Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, et al. (2011) 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy: Executive Summary. Circulation 124:2761-2796.
- Maron BJ, Rowin EJ, Udelson JE, Maron MS (2018) Clinical spectrum and management of heart failure in hypertrophic cardiomyopathy. JACC Hear Fail Elsevier; 6:353-363.
- Maron BJ, Dearani JA, Ommen SR, Maron MS, Schaff HV, et al. (2015) Low operative mortality achieved with surgical septal myectomy. J Am Coll Cardiol 66:1307-1308.
- Desai MY, Bhonsale A, Smedira NG, Naji P, Thamilarasan M, et al. (2013) Predictors of long-term outcomes in symptomatic hypertrophic obstructive cardiomyopathy patients undergoing surgical relief of left ventricular outflow tract obstruction. Circulation 128:209-216.
- Smedira NG, Lytle BW, Lever HM, Rajeswaran J, Krishnaswamy G, et al. (2008) Current effectiveness and risks of isolated septal myectomy for hypertrophic obstructive cardiomyopathy. Ann Thorac Surg 85:127-133.
- Sorajja P, Ommen SR, Holmes DR, Dearani JA, Rihal CS, et al. (2012) Survival after alcohol septal ablation for obstructive hypertrophic cardiomyopathy. Circulation Lippincott Williams & WilkinsHagerstown, MD 126:2374-2380.
- Sorajja P (2017) Alcohol septal ablation for obstructive hypertrophic cardiomyopathy. J Am Coll Cardiol 70:489-494.
- Veselka J, Faber L, Liebregts M, Cooper R, Januska J, et al. (2017) Outcome of alcohol septal ablation in mildly symptomatic patients with hypertrophic obstructive cardiomyopathy: A long-term follow-up study based on the Euro-alcohol septal ablation registry. J Am Heart Assoc 6:e005735.
- Nishimura RA, Seggewiss H, Schaff HV (2017) Hypertrophic obstructive cardiomyopathy: Surgical myectomy and septal ablation. Circ Res 121:771-783.
- Fifer MA, Yoerger DM, Picard MH, Vlahakes GJ, Palacios IF (2003) Covered stent septal ablation for hypertrophic obstructive cardiomyopathy: Initial success but ultimate failure resulting from collateral formation. Circulation 107:3248-3249.
- Anzuini A, Uretsky BF (2004) Covered stent septal ablation for hypertrophic obstruction cardiomyopathy. Circulation 3248-3249.
- Sianos G, Papafaklis MI, Vourvouri EC, Ligthart JT, Baks T, et al. (2006) Hypertrophic obstructive cardiomyopathy: Septal ablation with overlapping sirolimus-eluting and covered stents after failed alcoholization and concomitant coronary artery disease. Circulation 114:e553-e555.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences