Abstract
Severe Hypertrophic Cardiomyopathy: Septal Ablation with Coated Stent - A Case Report and Literature Review
Background: Hypertrophic cardiomyopathy (HMC) is a genetic pathology of cardiovascular origin cataloged as the leading cause of sudden death in young adults. Its genotypic and phenotypic presentation is diverse. 10% clinically identified of which 40% are asymptomatic. The first line therapy is the pharmacological one; in the absence of response, it is usually indicated to perform septal myectomy or alcohol septal ablation.
Case summary: Here, we describe the case of a 59-year-old woman, black, with an unclear history of cardiomyopathy, arterial hypertension of difficult management and atrial fibrillation (AF), who presented angina, high blood pressure, electrocardiographic abnormalities and elevation of cardiac biomarkers suggesting a non-ST elevated myocardial infarction (NSTEMI). This is an unusual case in which septal ablation was performed with a medicated stent as a treatment for severe HMC in a patient with paroxysmal AF without significant obstruction in coronary arteries.
Discussion: Only 10% of patients with HCM are clinically identified, 60% of these being symptomatic. Its presentation includes symptoms associated to congestive heart failure, chest pain and arrhythmias. The first-choice therapy is medical. When it fails, next step is septal reduction therapy either open or percutaneous intervention. Concerning the latter, non-alcoholic ablation with septal embolization (micro coils, polyvinyl alcohol, cyanoacrylate) has recently been proposed as an alternative; septal stent ablation is not recommended given the need for dual antiplatelet and the expected recurrence rate. In selected patients, septal stent ablation arises as an alternative to conventional management.
Author(s):
Juan David Rojas*, Mateo Guzmán, Diego Ardila and Arnold Méndez-Toro
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 241
Medical Case Reports received 241 citations as per google scholar report
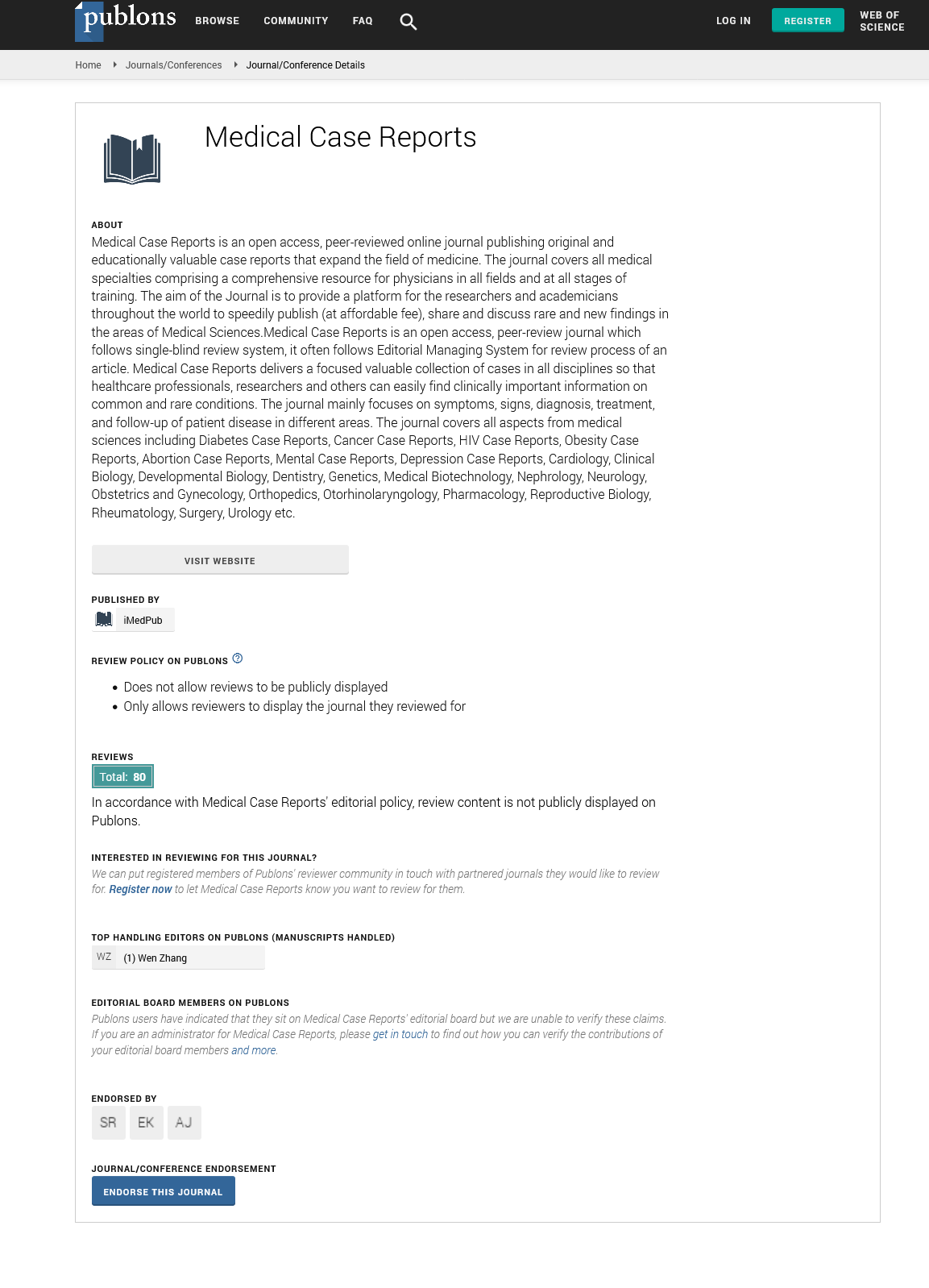
Medical Case Reports peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Cosmos IF
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Secret Search Engine Labs
- Euro Pub
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences