Management of a Pregnant Woman with Idiopathic Interstitial Pneumonia Accompanied by Secondary Pulmonary Hypertension: Case Report and Literature Review
Satoshi Ohira, Ryoichi Asaka, Yasuhiro Tanaka, Chiho Fuseya, Hirofumi Ando, Norihiko Kikuchi, Tsutomu Miyamoto, Makoto Kanai and Tanri Shiozawa
DOI10.21767/2471-8041.100081
Satoshi Ohira*, Ryoichi Asaka, Yasuhiro Tanaka, Chiho Fuseya, Hirofumi Ando, Norihiko Kikuchi, Tsutomu Miyamoto, Makoto Kanai and Tanri Shiozawa
Department of Obstetrics and Gynecology, Shinshu University School of Medicine, 3-1-1 Asahi, Matsumoto 390-8621, Japan
- *Corresponding Author:
- Satoshi Ohira
Department of Obstetrics and Gynecology
Shinshu University School of Medicine
3-1-1 Asahi, Matsumoto 390-8621, Japan
Tel: 81-263-37-2719
Fax: 81-263-39-3160
E-mail: osatoshi@shinshu-u.ac.jp
Received Date: October 14, 2017; Accepted Date: October 27, 2017; Published Date: October 29, 2017
Citation: Ohira S, Asaka R, Tanaka Y, Fuseya C, Ando H, et al. (2017) Management of a Pregnant Woman with Idiopathic Interstitial Pneumonia Accompanied by Secondary Pulmonary Hypertension: Case Report and Literature Review. Med Case Rep Vol.3 No.4:44. DOI: 10.21767/2471-8041.100079
Abstract
Idiopathic interstitial pneumonias (IIPs) typically occur in the fifth and sixth decades, and thus are uncommon in the child-bearing age group. We herein report an extremely rare case of a pregnant woman with IIP accompanied by secondary pulmonary hypertension that had a successful cesarean delivery. A 36-year-old primigravida woman was referred to our Obstetrics department at 6 weeks of gestation. Seven years ago, she had a dry cough and moderate dyspnea, and was diagnosed with non-specific interstitial pneumonia (NSIP), a subtype of IIP. At 11 weeks of gestation, spirometry showed a vital capacity of 1.89 L (60% of predicted). An arterial blood gas analysis showed PaO2 of 77.2 mmHg and oxygen saturation of 95% in breathing room air at rest. An echocardiogram revealed mild pulmonary hypertension; systolic pulmonary artery blood pressure (PABP) of 44 mmHg. Fetal growth and amniotic fluid volume were normal. Our management plan was to maintain oxygen saturation at more than 95% of oxygen saturation and systolic PABP at less than 50 mmHg. Oxygen therapy was initiated at 13 weeks of gestation because of dyspnea at rest. At 28 weeks of gestation, an echocardiogram showed severe pulmonary hypertension with systolic PABP of 64 mmHg. Therefore, we performed cesarean section at 30 weeks of gestation. The newborn was a male weighing 1.452 g with Apgar scores of 6 and 7 at 1 min and 5 min, respectively. Although the patient’s post-operative course was uneventful, she was discharged on a regimen of oxygen therapy. The effects of pregnancy on IIPs remain unclear because of its extreme rarity. In the management of pregnant women with IIPs accompanied by secondary pulmonary hypertension, the maintenance of systolic PABP of less than 50 mmHg on an echocardiogram may be effective.
Keywords
Pregnancy; Idiopathic interstitial pneumonia; Secondary pulmonary hypertension
Introduction
Idiopathic interstitial pneumonias (IIPs) are progressive inflammatory interstitial disease of unknown etiology, and have several subtypes including idiopathic pulmonary fibrosis (IPF) and non-specific interstitial pneumonia (NSIP). The mean age of presentation is between the fifth and sixth decades [1]. Therefore, IIPs are uncommon in the child-bearing age group, with only seven cases of pregnant women with IIPs being reported in the English literature [1-6]. We herein report an extremely rare case of a pregnant woman with IIP accompanied by secondary pulmonary hypertension.
Case Presentation
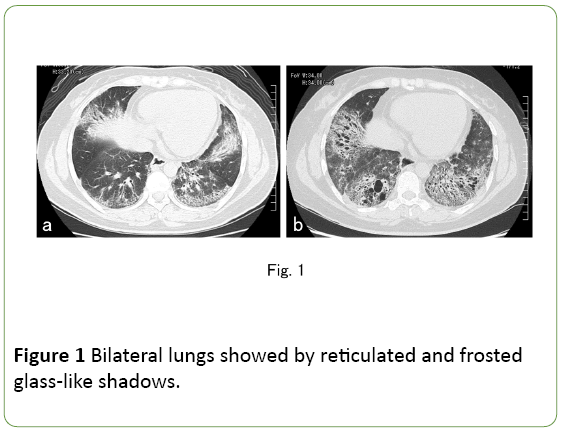
The patient was a 36-year-old primigravida woman. At 29 years of age, she had a dry cough and moderate dyspnea, and a chest CT scan revealed that the lower areas of the bilateral lungs were occupied by reticulated and frosted glass-like shadows (Figure 1a).
Rheumatoid factor and antinuclear factor were negative and C3 complement levels were normal. Based on these findings, she was diagnosed with NSIP. Although 15 mg/day of prednisolone and 140 mg/day of ciclosporin were administered, her chest CT scan at 35 years of age, i.e., three months before pregnancy, showed that reticulated and frosted glass-like shadows in the bilateral lungs had deteriorated (Figure 1b).
Although respiratory medicine physicians recommended contraception, she became pregnant because of her strong desire for a baby. She was referred to our Obstetrics department at 6 weeks of gestation. Bilateral end-inspiratory fine basal crepitations and marked clubbing of the fingers were noted in a physical examination.
At 11 weeks of gestation, spirometry showed a vital capacity (VC) of 1.89 L (60% of predicted) and forced expiratory volume in the first second (FEV1) of 1.42 L (52.4% of predicted). An arterial blood gas analysis showed PaO2 of 77.2 mmHg and oxygen saturation of 95% in breathing room air at rest. An echocardiogram revealed mild pulmonary hypertension with systolic pulmonary artery blood pressure (PABP) of 44 mmHg. Fetal growth and amniotic fluid volume were normal.
Our management plan was to maintain oxygen saturation >95% and systolic PABP <50 mmHg. Continuous supplemental oxygen of 1.5 L by a nasal cannula was started at 13 weeks of gestation because of dyspnea at rest. Breathlessness during conversation gradually worsened with the progression of pregnancy.
At 26 weeks of gestation, 3 L of oxygen therapy was needed to maintain oxygen saturation at more than 95%, and an echocardiogram showed systolic PABP of 48 mmHg. At 28 weeks of gestation, although 4 L of oxygen therapy was given, an echocardiogram showed severe pulmonary hypertension with systolic PABP of 64 mmHg. Therefore, we performed cesarean section at 30 weeks and 4 days of gestation.
Surgery was performed under general anesthesia and Swan- Ganz monitoring and was uneventful. The newborn was a male weighing 1.452 g with Apgar scores of 6 and 7 at 1 min and 5 min, respectively. Seven days after surgery, an echocardiogram showed systolic PABP of 38 mmHg. She was discharged on the 31st postoperative day with continuous supplemental oxygen of 1.5 L by a nasal cannula. The baby was discharged uneventfully when he was 62 days old.
Discussion
Patients with restrictive lung diseases have a decreased total lung capacity because of limited expansion of the lung or chest wall, a decreased functional residual capacity from decreased lung compliance, and hypoxemia that worsens with exertion [6,7].
Restrictive lung diseases may be caused by a number of disease parenchymal disorders, including IIPs, sarcoidosis, hypersensitivity pneumonitis, pneumonicosis, drug-induced lung diseases, and connective tissue diseases [6].
Co-existing interstitial lung diseases during pregnancy with associated hypoxemia may pose significant risks to the mother and fetus. The management of these patients requires careful planning, the monitoring of anticipated maternal and fetal issues and the appropriate use of supplemental oxygen [6].
Since adequate maternal oxygenation is PaO2 >70 mmHg, which is equivalent to oxygen saturation of 95%, to avoid any fetal effects of maternal hypoxia in cases of acute respiratory distress syndrome in pregnancy [8], we also performed oxygen supplementation to maintain oxygen saturation at more than 95% of in our case.
Limited information is available on the impact of IIPs on the course and outcome of a pregnancy because of the extreme rarity of pregnant women with IIPs. In our review of the literature, we only found seven cases (Table 1).
| Authors (ref.) | Age | History of pregnancy |
Subtypes of IIPs | VC, %VC of preconception or 1st-2nd trimester | Pulmonary hypertension | Supplemental oxygen | Course and outcome of pregnancy (weight of newborn) | Postpartum condition of IIP |
|---|---|---|---|---|---|---|---|---|
| Weiss, et al. (2) | 27 | 5G4P | IPF | 1.28 L, 35% | - | 30 weeks ÃÆïÃâýÃâà ¾ Low flow | VD at 36 weeks (1,899 g) | No change VC; 1.15 L, %VC; 32% |
| Prichard, et al. (3) | 25 | NA | IPF | 2.5 L, NA | NA | NA | Decreased respiratory function VD at 38 weeks (NA) | No change |
| Smythe, et al. (4) | 31 | 4G2P | IPF | 1.0 L, 33% | + | 15 weeks ÃÆïÃâýÃâà ¾ | Decreased respiratory function Preterm PROM and VD at 34 weeks 1,400 g) | No change, but sudden death at 3 weeks of postpartum Autopsy was refused |
| Sholapurkar, et al. (5) | 35 | 2G2P | IPF | 1.25 L, 46.5% | NA | NA | No improvement in respiratory condition Therapeutic abortion at 24 weeks | Improvement VC; 2.34 L, %V; 89.4% |
| Boggess, et al. (6) | 35 | 0G0P | IPF | 0.5 L, 17% | - | 20 weeks ÃÆïÃâýÃâà ¾ 2 L/min | Non-reassuring fetal status CS at 33 weeks (1,410 g) | No change 2 L/min of oxygen at home No change |
| Boggess, et al. (6) | 30 | 0G0P | IPF | 2.7 L, 80% | - | - | VD at 37 weeks (3,491 g) | No change |
| Sharma, et al. (1) | 24 | NA | IPF | NA | NA | 36 weeks ÃÆïÃâýÃâà ¾ | VD at 38 weeks (NA) | No change |
| Current case | 36 | 0G0P | NSIP | 1.89 L, 60% | + | 13 weeks ÃÆïÃâýÃâà ¾ 1.5 L/min | Decreased respiratory function Aggravation of pulmonary hypertension CS at 30 weeks (1.452 g) | No change 1.5 L/min of oxygen at home |
Table 1: Case reports of pregnant women with idiopathic interstitial pneumonia.
The ages of the 8 patients, including the present case, ranged between 24 and 36 years. Regarding the subtypes of IIPs, all seven previous cases had IPF, and our case is the first report of NSIP. Weiss et al. suggested that a minimal VC of one 1 L was deeded to sustain the ventilatory requirement of pregnancy [2].
However, in a case with only 0.5 L of VC at 20 weeks of gestation, her pregnancy was sustained until 33 weeks of gestation [6]. The infant was live-born in seven cases; however four out of 7 were preterm births. Sholapurkar et al. [5] reported a case necessitating therapeutic abortion at 24 weeks of gestation because of the lack of an improvement in her condition, even after one month of prednisolone therapy (40 mg daily).
She did not appear to have tolerated the additional workload by pregnancy and parturition; however detained information on her respiratory function was not available.
In pregnant women with IIP, a relationship with secondary pulmonary hypertension is possible. In our review of the literature (Table 1), we only found one case of a pregnant woman with IIP with secondary pulmonary hypertension [4].
The patient underwent cardiac catheterization at 15 weeks of gestation, and had slightly elevated pulmonary arteriolar resistance (218 dynes/sec/cm-5; normal range is within 100 dynes/sec/cm-5). At 34 weeks of gestation, the patient had premature rupture of the membranes and preterm labor; however, it was not reported whether the condition of pulmonary hypertension deteriorated [4].
Our case also had secondary pulmonary hypertension with a mild elevation in systolic PABP detected by an echocardiogram in the first trimester; systolic PABP ≥ 30 mmHg and <50 mmHg on an echocardiogram was classified as mild pulmonary hypertension [9].
Our management strategy was to maintain the systolic PABP at less than 50 mmHg because systolic PABP ≥ 50 mmHg on an echocardiogram was classified as severe pulmonary hypertension [9].
In our case, we terminated the pregnancy at 30 weeks of gestation because systolic PABP reached a severe range. The present report is the first case of a pregnant woman with IIP for which the pregnancy was terminated due to the deterioration of pulmonary hypertension.
Conclusion
In summary, although the influence of IIPs on pregnancy remains unclear, the present case showed that the maintenance of systolic PABP at less than 50 mmHg on an echocardiogram may be effective in the management of pregnant women with IIP and secondary pulmonary hypertension.
Acknowledgments
The authors are grateful to Hiroshi Yamamoto (First Department of Internal Medicine, Shinshu University School of Medicine) and Hirohiko Motoki (Department of Cardiovascular Medicine, Shinshu University School of Medicine) for the management of the patient.
Competing Interests
The authors declare that they have no competing interests.
References
- Sharma CP, Aggarwal AN, Vashisht K, Jindal SK (2002) Successful outcome of pregnancy in idiopathic pulmonary fibrosis. J Assoc Physicians India 50: 1446-1448.
- Weiss ST, Weinberger SE, Weiss JW, Johnson TS (1981) Normal pregnancy and delivery in a woman with severe underlying lung disease. Thorax 36: 878-879.
- Prichard MG, Musk AW (1984) Adverse effect of pregnancy on familial fibrosingalveolitis. Thorax 39: 319-320.
- Smyth AR, Galley GP Jr, Kraynack B (1985) Assessment of severe pulmonary disease in pregnancy with Swan-Ganz monitoring: A report of two cases. J Reprod Med 30:133-138.
- Sholapurkar SL, Vasishta K, Dhall GI, Jindal SK (1991) Idiopathic pulmonary fibrosis (IPF) necessitating therapeutic mid-trimester abortion: A case report. Asia Oceania J ObstetGynaecol 17: 303-306.
- Boggess KA, Easterling TR, Raghu G (1995) Management and outcome of pregnant women with interstitial and restrictive lung disease. Am J ObstetGynecol 173: 1007-1014.
- King TE (1992) Restrictive lung disease in pregnancy. Clin Chest Med 13: 607-622.
- Mehta N, Chen K, Hardy E, Powrie R (2015) Respiratory disease in pregnancy. Best Pract Res ClinObstetGynaecol 29: 598-611.
- Katsuragi S, Yamanaka K, Neki R, Kamiya C, Sasaki Y, et al. (2012) Maternal outcome in pregnancy complicated with pulmonary arterial hypertension. Circ J 76: 2249-2254.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences