Case Report: Suspicion of Amyloidosis Induced Peripheral Neuropathy
Amer I Zabalawi
Canadian Academy of Pain Medicine, Ontario, Canada
Published Date: 2024-01-19DOI10.36648/2471-8041.9.12.332
Amer I Zabalawi1,2* and Qusai N Al-Shahed3
1Canadian Academy of Pain Medicine, Ontario, Canada
2The College of Family Physicians, Ontario, Canada
3Department of Nursing, Haja Andaleeb Al-Amad Nursing and Midwifery College, Nablus, Palestine
- *Corresponding Author:
- Amer I Zabalawi
Canadian Academy of Pain Medicine, Ontario,
Canada,
E-mail: amer.zabalawi@hotmail.com
Received date: December 19, 2023, Manuscript No. IPMCRS-23-18216; Editor assigned date: December 22, 2023, PreQC No. IPMCRS-23-18216 (PQ); Reviewed date: January 05, 2024, QC No. IPMCRS-23-18216; Revised date: January 12, 2024, Manuscript No. IPMCRS-23-18216 (R); Published date: January 19, 2024, DOI: 10.36648/2471-8041.9.12.332
Citation: Zabalawi AI, AI-Shahed QN (2023) Case Report: Suspicion of Amyloidosis Induced Peripheral Neuropathy. Med Case Rep Vol.9 No.12: 332.
Abstract
39 years old known case of chronic polymyositis and multiple comorbidities, developed new onset progressive sharp pain, numbness and reduced sensation on feet. Symptoms increased in severity and started ascending over one month duration affecting whole both lower limbs. Initial investigation started with Nerve Conduction Study (NCS)/ Electromyography (EMG) testing which showed sensory axonal neuropathy, then a full spectrum lab workup and lumbar magnetic resonance scans were done which didn’t show any acute changes related to the concerning symptoms. Due to amyloidosis query, a buccal biopsy was done and result came back positive for Congo red stain raising the possibility of amyloidosis induced peripheral neuropathy. This case presents the diagnostic path of acute onset peripheral neuropathy in a patient with autoimmune condition, multi-comorbidities and suspicion of amyloidosis.
Keywords
Polymyositis; Amyloidosis; Peripheral neuropathy; Electromyography
Introduction
Peripheral neuropathy is one of the common neurologic problems encountered by neurologists and pain practitioners. The onset can be acute, subacute or chronic. Peripheral nerves consist of sensory, motor and autonomic nerve fibers. Nerve damage can be caused by several different conditions or might be idiopathic (unknown) [1,2]. Damage affecting sensory nerves might present as tingling, sharp, burning pain, extreme sensitivity to touch, lack of coordination and falling. If motor nerves are affected, muscle weakness and paralysis might present. Autonomic nerves damage cause heat intolerance, sweating disturbance, bowel motion and bladder contraction disturbance, drop in blood pressure which might cause dizziness or light-headedness [3]. Common causes of peripheral neuropathy are diabetes, exposure to toxic substances including (chemotherapeutics, alcohol, insecticides, solvents and heavy metals), B12 and folate vitamin deficiencies, connective tissue conditions, immune-mediated conditions, cancers such as lymphoma and multiple myeloma, chronic liver and kidney disease, HIV, lyme and thyroid conditions [1]. Neuropathy cases need comprehensive assessment including; detailed clinical history, complete physical examination, nerve conduction studies, full spectrum blood workup, genetic testing and in some cases nerve biopsies are carried out to identify the cause [4,5].
Case Presentation
Patient is a known case of multiple comorbidities (albinism, morbid, obesity, chronic polymyositis, osteoporosis, vitamin D insufficiency, multiple lumbar spine compression fractures treated with kyphoplasty procedure, steroid induced myopathy, multiple healed rib fractures, primary testicular dysfunction, diverticulitis, anal fistulae, chronic venous disease (stage 4) and hyperuricemia).
Patient presented with progressive sharp pain bouts, numbness and reduced sensation on feet. It has increased in severity over one month duration, ascending and covering lower limbs symmetrically to reach the saddle area. Patient denies any history of (recent major trauma, recent spinal interventions, new onset joint changes/pain, fever, rash, bowel motion changes, urinary symptoms, night sweats, weight loss, IV drug use, new medication/vaccination use, exposure to sick contacts, travel, risky sexual exposure) and sphincter control was not affected.
Physical exam
Albinism, obesity and general muscular atrophy. No (jaundice, pallor, cyanosis, enlarged lymph nodes).
Vital signs
Temperature: 36.8°C.
Blood pressure: 145/70 mmHg (when lying down), 140/70 mmHg (after standing up).
Heart rate: 84/min.
Respiratory rate: 15.
Neuro: PERRLA, intact cranial nerves 2-12, no focal signs, no diadochokinesis, physiologic finger-nose-test.
Lumbar Sacral Spine (LSS): Kyphoplasty procedure scar, no spine tenderness on percussion, evident reduced (flexion, extension, lateral flexion and rotation).
Lower limbs: Low gait velocity, short stride length, muscular atrophy, stage 4 varicose veins with skin hemosiderosis over ankles, soles skin dryness and multiple calluses. Proximal myopathy of both hipslexion grade 3/5 on the MRC scale.
Evident hyperalgesia, reduced perception of fine, sharp, vibration and position sense over lower limbs bilaterally more noticed on his soles and ankles. No foot drop.
Deep tendon reflex status: Patellar tendon 2 /2, Achilles tendon 0/2 bilaterally.
CVS: No facial rash, no increased cardiac dullness, no Jugular Vein Distention (JVD) elevation, normal S1/S2, no pathologic murmurs.
Respiratory: Trachea central, good chest expansion, resonant percussion, good air entry bilaterally, no added sounds.
Abdomen: Soft lax, no distention or fullness, no tenderness of the abdomen, no hepato spleen megaly, no pulsatile motion or masses, bowel sounds are regular.
Investigations
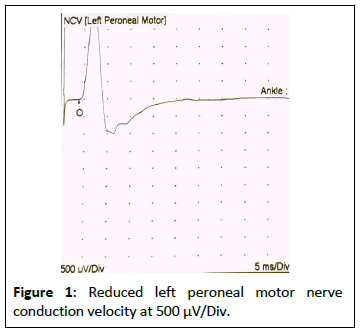
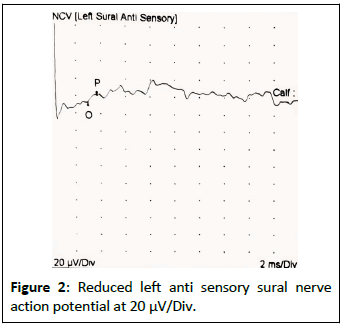
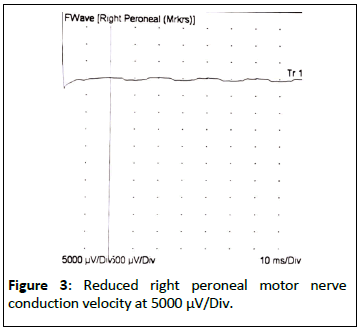
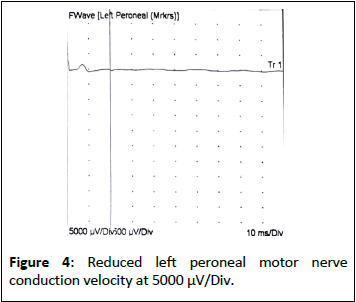
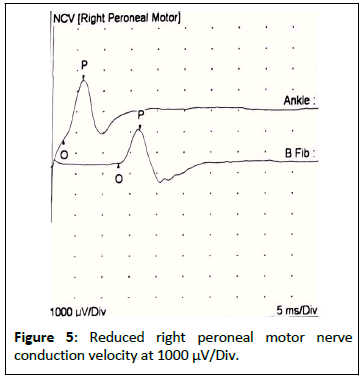
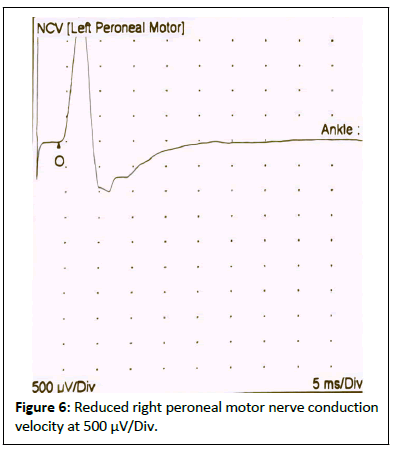
NCS/EMG: Decrease SNAPs of both sural nerves, decrease MAPs of both peroneal nerves (Tables 1 and 2) (Figures 1-6).
| Site | NR | Peak (ms) | Normal peak (ms) | O-P Amp (µV) | Norm O-P Amp | Site 1 | Site 2 | Delta-0 (ms) | Distance (cm) | Velocity (m/s) | Normal velocity (m/s) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Left sural anti sensory (Lat mall) | |||||||||||
| Calf | 3.7 | <4.0 | 6.8 | >14 | Calf | Lat mall | 3 | 13 | 43 | >35 | |
| Right sural anti sensory (Lat mall) | |||||||||||
| Calf | 3.7 | <4.0 | 6.9 | >14 | Calf | Lat mall | 3.1 | 13 | 42 | >35 | |
| Note: Reduced anti sensory nerve action potential for both sural nerves. | |||||||||||
Table 1: Sural le t and right comparison.
| Site | L Lat (ms) | R Lat (ms) | L-R Lat (ms) | L Amp (mV) | R Amp (mV) | L-R Amp (%) | Site 1 | Site 2 | L Velocity (m/s) | R Velocity (m/s) | L-R Velocity (m/s) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Peroneal motor (Ext Dig Brev) | |||||||||||
| Ankle | 3.9 | 2.7 | 1.2 | 2.6 | 2.9 | 10.3 | |||||
| Tibila motor (Abd Hall Brev) | |||||||||||
| Ankle | 5.4 | 5.5 | 0.1 | 4.9 | 5 | 2 | |||||
Table 2: Motor left and right comparison.
LSS MR: Mild to moderate degenerative disk disease changes, no (disk protrusion, canal stenosis, foraminal narrowing) at any level, lumbar vertebral heights well restored, no fracturescement leakage, conus is unremarkable.
Blood workup: HBA1c, random blood sugar, Creatine Phosphokinase (CPK), Aspartate Transaminase (AST), Alanine Aminotransferase (ALT), vitamin B12/B1/E, Complement levels (C3,C4), Erythrocyte Sedimentation Rate (ESR), Anti-Double Stranded DNA (Anti-dsDNA), Myeloperoxidase (MPO), Systemic mastocytosis (Sm), Ribonucleoprotein (RNP), anti-jo-1, Scl-70, cenp-b, Antinuclear Antibodies (ANA), Anti-Neutrophil Cytoplasmic Antibodies (C-ANCA), Perinuclear Anti-Neutrophil Cytoplasmic Antibodies (P-ANCA), ross-a-52, PR3 (proteinase 3), M2 Anti-Mitochondrial Antibodies (AMA-M2), antibodies to Liver Cytosol Antigen Type 1 (LC1), Liver Kidney Microsomal Antibody Type 1 (LKM1), pm-scl100, srp54, sp100, gp100, ku, lass-b, Serum Protein Electrophoresis (SPEP), anti-gliadin Ab., copper test (Table 3).
| Test | Result | Test | Result |
|---|---|---|---|
| HbA1c | Normal | Antibodies to Liver Cytosol Antigen Type 1 (LC1) | Normal |
| Random blood sugar | Liver Kidney Microsomal Antibody Type 1 (LKM1) | ||
| Creatine Phosphokinase (CPK) | pm-scl100 | ||
| Aspartate Transaminase (AST) | srp54 | ||
| Alanine Aminotransferase (ALT) | sp100 | ||
| Vitamin B12 | gp100 | ||
| Vitamin B1 | ku | ||
| Vitamin E | lass-b | ||
| Copper test | Serum Protein Electrophoresis (SPEP) | ||
| Complement Levels (C3,C4) | anti-gliadin Ab. | ||
| Erythrocyte Sedimentation Rate (ESR) | M2 Anti-Mitochondrial Antibodies (AMA-M2) | ||
| Anti-Double Stranded DNA (Anti-ds DNA) | Ribonucleoprotein (smRNP) | ||
| Myeloperoxidase (MPO) | Anti-jo-1 | ||
| Systemic Mastocytosis (SM) | Scl-70 | ||
| Perinuclear Anti-Neutrophil Cytoplasmic Antibodies (P-ANCA) | Cenp-B Antinuclear Antibodies (ANA) | ||
| ross-a-52 | Anti-Neutrophil Cytoplasmic | ||
| pr3 | Antibodies (C-ANCA) |
Table 3: Blood workup investigations.
All the blood workup investigations listed above were normal. Due to this presentation, it was worth to look for fewer common conditions as amyloidosis, so a buccal biopsy was done. Biopsy pathology report showed; thickened eroded oral mucosa, severely inflamed granulation tissue with dense plasma cell infiltrate. Congo red stain for amyloid is positive, with no malignancy.
This positive test has raised the possibility of amyloidosis induced peripheral neuropathy. In order to reevaluate the case and confirm the biopsy results, the patient was referred to amyloidosis specialized center. The positive buccal mucosa biopsy done initially was sent to the center for revaluation.
The re-evaluated buccal biopsy pathology report shows: Mixed, dense inflammatory infiltrates with abundant plasma cells in subepithelial connective tissue and few lymphocytes. No certain evidence of atypical birefringence in the Congo red stain. The inflammation is compatible with periodontitis, no positive reaction with antibodies against amyloid P component, AA-amyloid, apolipoprotein A1, lambda light chain (3 antibodies), kappa light chain (2 antibodies) and transthyretin no light chain restriction in the inflammatory infiltrate (Table 4).
| Biopsy | Result |
|---|---|
| Buccal biopsy pathology report | Congo red stain for amyloid is positive with no malignancy. Thickened eroded oral mucosa severely inflamed granulation tissue with dense plasma cell infiltrate |
| Re-evaluated buccal biopsy pathology report | Mixed, dense inflammatory infiltrates with abundant plasma cells in subepithelial connective tissue and few lymphocytes. No certain evidence of atypical birefringence in the congo red stain. No positive reaction with antibodies against amyloid P component, AA-amyloid, apolipoprotein A1, lambda light chain (3 antibodies), kappa light chain (2 antibodies) and transthyretin no light chain restriction in the inflammatory infiltrate. |
Table 4: Buccal biopsy investigations.
The following investigations were done at the amyloidosis specialized center:
Molecular genetic investigation of the peripheral blood: No disease-causing pathogenic sequence variants in the analyzed regions of the TTR gene. We can exclude hereditary amyloidosis due to a pathogenic sequence variant in the coding regions of the TR gene in the patient.
Echocardiography: Good systolic function (left ventricular ejection function 60%), no regional contraction disturbances, good longitudinal function, no relevant left-ventricular diastolic dysfunction, LA, RA and RV not enlarged, good RV function. No pericardial effusion. The vena cava is not congested, valves sonography and doppler are regular. Echocardiographic criteria for amyloidosis not fulfilled.
Abdominal fat aspiration: No deposits of amyloid found (Table 5).
| Test | Result |
|---|---|
| Molecular genetics of the peripheral blood | No disease-causing pathogenic sequence variants in the analyzed regions of the TTR gene |
| Echocardiography | Good systolic function (left ventricular ejection function 60%), no regional contraction disturbances, good longitudinal function, no relevant left-ventricular diastolic dysfunction, LA, RA, and RV not enlarged, good RV function. No pericardial effusion. The vena cava is not congested, valves sonography and doppler are regular. Echocardiographic criteria for amyloidosis not fulfilled |
| Abdominal fat aspiration | No deposits of amyloid found |
Table 5: Amyloidosis specialized center investigations.
Results and Discussion
Approaching cases of polyneuropathy needs a thorough systemic path; detailed history, complete physical exam and NCS/EMG are important steps in the path to confirm neuropathy diagnosis. Blood workup, tissue aspiration, genetic testing and skin biopsy are investigations carried to reach solid diagnosis. Sural nerve biopsy is rarely done, it is reserved if the picture is not clear and needs further confirmation. It has its own complications of pain, infection, sensory loss and delayed wound healing [1,4,6,7]. In this case, it is noteworthy that the patient suffered from multiple comorbidities and autoimmune polymyositis condition, which raised the suspicion of autoimmune connective tissue disease as the triggering cause, but the investigations meant for connective tissue disease were normal. As part of the workup, metabolic, celiac, copper, B vitamins and folate levels were done and turned also normal. This acute painful and rapid progressive presentation brought up a query of more rare cause as amyloidosis, so a buccal biopsy was done to check for Congo red stain, which turned positive, raising concerns about amyloidosis condition [6,8]. Patient was assessed at amyloidosis specialized center. The buccal biopsy was retested again for Congo red staining and furtherly for amyloid antibodies. The patient was tested correspondingly for molecular genetics of the peripheral blood, echocardiography and abdominal fat aspiration for deposits of amyloid [6,9,10]. All these tests turned negative for amyloid and the buccal biopsy revaluation was compatible with periodontitis, with no evidence of amyloid deposits.
Patient was started on vitamin D 50,000 IU weekly, daily (oral b complex, oral alpha lipoic acid 1000 mg and pregabalin 75 mg) [11-13].
Patient was directed to follow-up with neurology and pain clinics after two weeks for revaluation of a presumed case of connective tissue versus idiopathic peripheral neuropathy condition.
Conclusion
In order to confirm or exclude amyloidosis suspicion, full spectrum amyloidosis testing should be completed at a specialized center through revaluating biopsies for amyloid antibodies, undertaking peripheral blood molecular genetics, echocardiography and abdominal fat aspiration.
Data Availability Statement
The original contributions presented in the study are included in the article.
Supplementary Material
Further inquiries can be directed to the corresponding author.
Ethics Statement
The patient and participants provided their written informed consent to participate in this case report.
Author Contributions
The authors listed have made a substantial, direct and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the report was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- (2014) Peripheral neuropathy. Disorders, National Institute of Neurological Disorders and Stroke Bethesda, MA, USA.
- Castelli G, Desai KM, Cantone RE (2020) Peripheral neuropathy: Evaluation and differential diagnosis. Am Fam Physician 102: 732-739.
[Google Scholar], [Indexed]
- Hammi C, Yeung B (2022) Neuropathy. StatPearls Publishing, Florida, USA.
- Chambers AR, Song K (2023) Sural nerve biopsy. StatPearls Publishing, Florida, USA.
- Lehmann HC, Wunderlich G, Fink GR, Sommer C (2020) Diagnosis of peripheral neuropathy. Neurol Res Pract 2: 1-7.
[Crossref], [Google Scholar], [Indexed]
- Benson MD, Berk JL, Dispenzieri A, Damy T, Gillmore JD, et al. (2022) Tissue biopsy for the diagnosis of amyloidosis: Experience from some centres. Amyloid 29: 8-13.
[Crossref], [Google Scholar], [Indexed]
- Azhary H, Farooq MU, Bhanushali M, Majid A, Kassab MY (2010) Peripheral neuropathy: Differential diagnosis and management. Am Fam Physician 81: 887-892.
[Google Scholar], [Indexed]
- Bucci T, Bucci E, Rullan AM, Bucci P, Nuzzolo P (2014) Localized amyloidosis of the upper gingiva: A case report. J Med Case Rep 8: 1-4.
[Crossref], [Google Scholar], [Indexed]
- Qian M, Qin L, Shen K, Guan H, Ren H, et al. Light-chain amyloidosis with peripheral neuropathy as an initial presentation. Front Neurol 12: 1658.
[Crossref], [Google Scholar], [Indexed]
- Hachulla E, Grateau G (2002) Diagnostic tools for amyloidosis. Joint Bone Spine 69: 538-545.
[Crossref], [Google Scholar], [Indexed]
- Mijnhout GS, Alkhalaf A, Kleefstra N, Bilo HJG (2010) Alpha lipoic acid: A new treatment for neuropathic pain in patients with diabetes. Neth J Med 68: 158-62.
[Google Scholar], [Indexed]
- Derry S, Bell RF, Straube S, Wiffen PJ, Aldington D, et al. Pregabalin for neuropathic pain in adults. Cochrane Database Syst Rev 1: CD007076.
[Crossref], [Google Scholar], [Indexed]
- Julian T, Syeed R, Glascow N, Angelopoulou E, Zis P (2020) B12 as a treatment for peripheral neuropathic pain: A systematic review. Nutrients 12: 2221.
[Crossref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences