A sequestrated Lung presenting as Lung abscess- a rare case.
Sivaresmi Unnithan
Ranjan K Das1, Bhabatosh Biswas M2 and Sivaresmi Unnithan1*
1Department of Pulmonary Medicine, Calcutta Medical Research Institute, India
2Department of Cardiothoracic Surgery, Calcutta Medical Research Institute, India
- *Corresponding Author:
- Dr. Sivaresmi Unnithan
Department of Pulmonary Medicine
Calcutta Medical Research Institute
India
Tel: 9051301137
E-mail: sivaresmi@gmail.com
Received date: February 18, 2016; Accepted date: April 15, 2016; Published date: April 20, 2016
Citation: Das RK , Bhabatosh Biswas M, Unnithan S. A Sequestrated Lung Presenting as Lung Abscess- A Rare Case. Med Case Rep. 2016, 2:2.
Abstract
INTRODUCTION: Intralobar pulmonary sequestration [ILS] is overall the most common form of Bronchopulmonary sequestration (BPS) usually occurring in the left lower lobe commonly presenting as consolidation in the lower lung lobes. METHODS: A young male [23 years] presented with hemoptysis and a large cavity with air fluid level in the left lower lung lobe for 6-7 years. Computed Tomography of chest and bronchoscopy were inconclusive and therefore he was taken up for lobectomy. RESULTS: The intraoperative finding was a sequestered lower lobe with a separate arterial supply directly from the thoracic aorta CONCLUSION: Cystic and cavitary lesions are rare presentations of ILS and are often diagnosed only during surgery. This is a rare case of pulmonary sequestration that presented to us in the form of a lung abscess.
Keywords
Pulmonary sequestration; Lung abscess; Intralobar; Extralobar
Introduction
Bronchopulmonary sequestration (BPS) is most of the times simply referred to as pulmonary sequestration and is estimated to comprise 0.15 to 6.4 percent of all congenital pulmonary malformations [1,2]. Sequestrations are classified anatomically as interlobular pulmonary sequestration (ILS, also known as intrapulmonary sequestration), in which the lesion is located within a normal lobe without its own visceral pleura and extralobar pulmonary sequestration (ELS, also known as extra pulmonary sequestration), in which the lesion is located outside the normal lung and has its own visceral pleura (also called “accessory lung”). The diagnosis is usually made preoperatively in most of the cases [3,4]. In our case, the presentation of the patient was recurrent chest infections and a lung abscess not responding to anti tubercular drugs.
Methods
A 23 year old normotensive non diabetic male presented to us with a 2 year history of occasional episodes of hemoptysis and complaints of generalized weakness , several episodes of cough with expectoration and low grade fever in the past 6-7 years. A complete work up included routine blood investigations, chest radiography, computerized tomography of chest and bronchoscopy.
Results
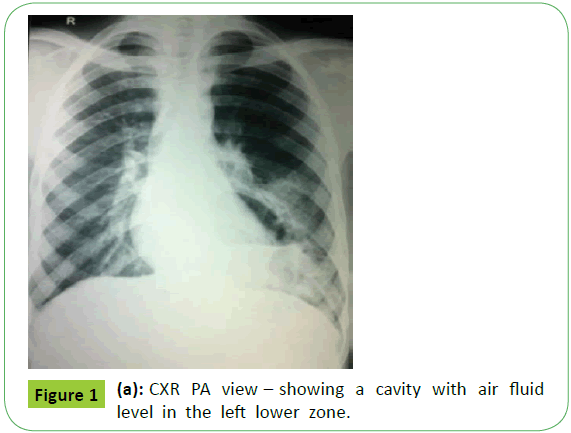
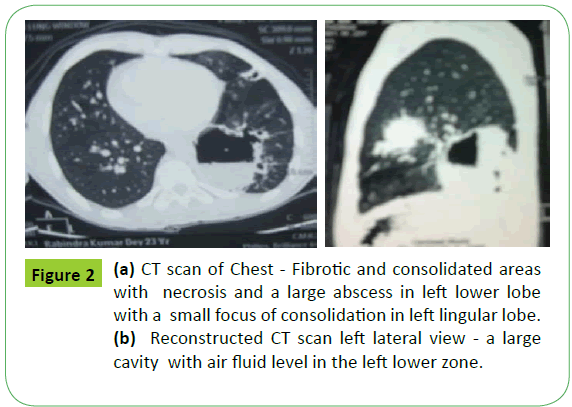
His chest radiograph (Figure 1) showed a large cavity with air fluid level in the left lower zone. A chest radiograph done in 2009 also showed the same findings. He had been treated 3 years ago with broad spectrum antibiotics along with empirical ant tubercular drugs considering it to be a tubercular lung abscess although his sputum for negative for acid fast stain bacilli. But the abscess persisted. Computed Tomography (CT thorax) (Figures 2a and 2b) revealed fibrotic and consolidated areas with necrosis and a large abscess in left lower lobe with a small focus of consolidation in left lingular lobe.
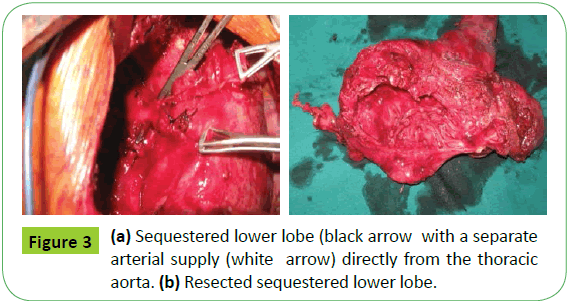
On examination, he was hemodynamically stable and was afebrile. He had second grade clubbing and there were coarse crepitations over the basal part of left hemithorax on auscultation. Sputum for acid fast bacilli (AFB) was negative and culture showed no growth. Bronchoscopy revealed no end bronchial abnormality and his bronchoalveolar lavage (BAL) revealed no AFB, fungus or any other microorganism. In view of recurrent hemoptysis and persistence of thick walled cavity, he was admitted for lobectomy (left lower lobe). The intra operative finding was a sequestered lower lobe with a separate arterial supply directly from the thoracic aorta (Figures 3a and 3b). The sequestered lobe along with lingular lobe were resected and sent for histopathology. Histopathological examination revealed a mixed pattern of respiratory bronchiolitis, interstitial lung disease and desquamative interstitial pneumonia. The singular lung tissues showed chronic inflammation. The postoperative period was uneventful. His repeat chest radiograph after 3 weeks showed blunting of the left costophrenic angle with features of minimal pleural thickening.
Discussion
Bronchopulmonary sequestration is included amongst the rare group of congenital pulmonary anomalies. Bronchopulmonary sequestration can be described as a region of lung parenchyma that is partially or completely separated from the Bronchopulmonary tree of the lung proper. Its blood supply is usually from an aberrant artery arising from the aorta or one of its branches. It consists of abnormal nonfunctioning pulmonary tissue, including airway and alveolar elements and lacks normal communication with the tracheobronchial tree [5]. The term “sequestration” was first used in the medical literature by Pryce in 1946. Its origin is from the Latin word sequestare, which means “to separate.”
ILS [Intralobar pulmonary sequestration] is overall the most common form, accounting for about 75 to 90 percent of sequestrations. It usually occurs in the left lower lobe (67%). Intralobar pulmonary sequestration presents in adolescence or adulthood in the form of recurrent pneumonia, whereas ELS more commonly presents in the fetal and neonatal period along with other congenital anomalies. Overall there is equal gender distribution in pulmonary sequestration but males are 4 times more likely to present in the extra pulmonary form [6-8].
The arterial supply of ILS is from either thoracic or abdominal aorta whereas ELS derives its arterial supply from the abdominal aorta usually. The venous return of the intralobular variety is into pulmonary veins whereas the extralobar variety drains into the systemic veins [9].
A vast majority of patients with intralobar sequestration are asymptomatic and symptoms, when present, are often nonspecific which may include chest pain, pleuritic pain, shortness of breath, and wheezing. Recurrent infection, however, is more common signs which are indicated by fever and productive cough. This risk of infection occurs despite the absence of a direct connection with the tracheobronchial tree because these sequestrations are not completely isolated from the native lung. Bacteria can invade through the alveolar pores of Kohn. Once bacteria have colonized the sequestration, frank infection can ensue because of the lack of normal bronchial drainage [10,11]. Usually the cysts are found to contain glairy mucus or in some cases pus [12].
Our reviews about patients with bronchopulmonary sequestration revealed that a diagnosis of sequestration requires a high index of suspicion. A chest radiograph may reveal a homogeneous lesion in the lung base in uncomplicated intralobular sequestration, whereas complicated sequestration may show as a cystic lesion with air-fluid levels [13,14]. But on the whole, the commonest radiological presentation is an ill-defined consolidation that is usually mistaken as non-resolving pneumonia [15]. Chest CT usually shows a discrete mass in the posterior- or medial-basal segment of the lower lobe, with or without cystic changes [15]. Cystic changes, when present, are usually multiple in nature. Colin R Cooke in 2006 reports a case where a cystic lesion [multiple cysts] in the right lower lobe was found to be a sequestered lobe. [11]
R. Prasad et al. in 2009 report a case of a 35 year old ATT non responder whose CT scan of Chest showed a cavity with fluid level localized to left lower anterobasal and posteromediobasal segments [16]. Bilal Mirza et al. reported a 2-year-old boy presenting with recurrent episodes of chest infections and respiratory distress with an intralobular pulmonary sequestration disguised as congenital lobar emphysema on the right side [17].
In 1961, B. T. Le Roux reported a series of 8 cases of intralobar pulmonary sequestration, in which 4 were polycystic; one was a single large cyst and another an 8-year-old boy admitted in 1951 with the diagnosis of either a lung abscess or a loculated empyema. Pus was obtained on thoracentesis in this 8 year old boy and thoracotomy revealed a pulmonary sequestration in the right lower lobe [12].
In many of the cases, the diagnosis of pulmonary sequestration is made preoperatively [3,4]. In suspected cases, CT scan of the chest with contrast and CT aortography and pulmonary angiography are important modalities for the diagnosis of the sequestration as well as to delineate its blood supply [3].
Again, as we browsed further through relevant articles, we learnt that lesions present in lobes other than the lower lobe should spur investigation of alternative diagnoses, as sequestration outside of the lower lobes accounts for only 5% of cases reported in the literature [18]. This makes our case more unique because of the concomitant involvement of the left lingula.
In our case, the patient had presented to us with a cavitary lesion with air fluid level in the left lower zone right from the beginning. Non response to ATT was noted. The presence of a large lung abscess with repeated episodes of hemoptysis and unremarkable findings of FOB prompted us to proceed for lobectomy
Differential for this case included bronchogenic CA, metastatic disease, lung abscess, pulmonary infarction, TB, PCP, fungal infection, Wegener’s granulomatosis and infected bronchogenic cyst. During the operation, the diagnosis of intralobar pulmonary sequestration was made on the basis of detection of a separate arterial supply from the thoracic aorta. Moreover, histopathology confirmed the presence of primitive lung tissue.
Conclusion
Cystic and cavitary lesions are rare presentations of ILS and are often diagnosed only during surgery. This is a rare case of pulmonary sequestration that presented to us in the form of a lung abscess.
References
- Raemdonck D, Boeck K, Devlieger H, Maurits D, Toni L, et al. (2001) Pulmonary sequestration: a comparison between pediatric and adult patients. Eur J Cardiothorac Surg 19: 388-395.
- Corbett H, Humphrey M (2004) Pulmonary sequestration. Paediatr Respir Rev 5: 59-68.
- Shah M, Bhatt B, Modi M (2003) Case report: Extra lobar pulmonary sequestration. Indian J Radiol Imaging 13: 271-273.
- Felker E, Tankin L (1990) Imaging of pulmonary sequestration. AJR Am J Roentgenol 154: 241- 249.
- Landing H, Dixon G (1979) Congenital malformations and genetic disorders of the respiratory tract (larynx, trachea, bronchi, and lungs). Am Rev Respir Dis 120:151.
- Pryce M (1946) Lower accessory pulmonary artery with intralobar sequestration of lung: report of seven cases. J Pathol Bacteriol 58:457- 467.
- Clements S (1999) Congenital malformations of the lungs and airways. In: Pediatric Respiratory Medicine, Taussig LM, Landau LI (eds), Mosby, St Louis 1999. p.1106.
- Bruce M. Schnapf O (2003) Pulmonary sequestration. E- Medicine Journal 2628.
- Nicolette A, Kosloske M, Bartow A, Murphy S (1993) Intralobar pulmonary sequestration: A clinical and pathological spectrum. J Pediatr Surg 6: 802-805.
- Kumar V, Abbas K, Fausto N (2005) Pathologic basis of disease, (7thedn) Elsevier Saunders, Philadelphia.
- Colin R, Cooke M (2006) Bronchopulmonary Sequestration. Respir Care 51:661-664.
- Le Roux BT (1962) Intralobar pulmonary sequestration. Thorax 17:77-84.
- Bolca N, Topal U, Bayram S (2004) Bronchopulmonary sequestration: radiologic findings. Eur J Radiol 52:185-191.
- Hirai S, Hamanaka Y, Mitsui N, Uegami S, Matsuura Y (2007) Surgical treatment of infected intralobar pulmonary sequestration: A collective review of patients older than 50 years reported in the literature. Ann Thorac Cardiovasc Surg 13: 331- 334.
- Zylak J, Eyler R, Spizarny L, Stone H (2002) Developmental lung anomalies in the adult: radiologic-pathologic correlation. Radiographics 25-43.
- Petersen G, Martin U, Singhal A, Criner J (2003) Intralobar sequestration in the middle-aged and elderly adult: recognition and radiographic evaluation. J Thorac Cardiovasc Surg 126: 2086-2090.
- Prasad R, Garg R, Verma K (2009) Intralobar sequestration of lung. Lung India. 26: 159-161.
- Mirza B, Raza B, Ijaz I, Ijaz L, Naz F, et al. (2011) Intralobar pulmonary sequestration masquerading as congenital lobar emphysema. J Indian Assoc Pediatr Surg 16: 15-17.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences