The Use of Demineralized Dentin Matrix as a Graft Material After Extraction Clinical Case
Sherif Nesma*, Quevedo Miguel and Suarez Jose Maria
Department of Medicine and Dentistry, Clinical tutor of Oral Surgery, Santiago de Compostela University, Spain
- *Corresponding Author:
- Sherif Nesma
Department of Faculty of Medicine and Dentistry,
Clinical tutor of Oral Surgery, Santiago de Compostela University,
Spain,
Tel: 34651762767;
E-mail: sherif.kz@gmail.com
Received: February 18, 2022, Manuscript No. IPMCRS-22-11901; Editor assigned: February 21, 2022, PreQC No. IPMCRS-22-11901 (PQ); Reviewed: March 07, 2022, QC No. IPMCRS-22-11901; Revised: March 11, 2022, Manuscript No. IPMCRS-22-11901 (R); Published: March 18, 2022, 10.36648/2471-8041.8.3.215
Citation: Nesma S, Miguel Q, Maria SJ (2022) The Use of Demineralized Dentin Matrix as a Graft Material after Extraction Clinical Case. Med Case Rep Vol.8 No.3
Abstract
The main purpose of this case report is to evaluate the procedure and effectiveness of using the patient’s own Demineralized Dentin Matrix (DDM) as a graft material for socket preservation. After atraumatic extraction of unrestorable remaining teeth and roots, only sound teeth are used in this protocol. The procedure consists of cleaning and drying the caries free tooth that is composed of mostly dentin, and then grinds it immediately using a specially designed machine, in our case we used the Tooth Transformer device. The dentin particles of 300-1200 um are sieved through a special sorting system. Autogenously demineralized dentin particles grafted immediately after extractions can be considered as the gold standard for socket preservation, bone augmentation and bone defects correction. Along with minimally invasive techniques and taking advantage of the regenerative power that encloses the patient´s own tooth, we will try to change the paradigm and give a reasonable alternative to more risky techniques and with greater morbidity for the patient.
Keywords
Demineralized dentin; Bone regeneration; Socket shield; Tooth transformer
Introduction
The extraction of a tooth is sometimes inevitable, which produces, short and medium term set of morphological and physiological changes at the alveolar level, that must be taken into consideration in the planning of future rehabilitation. Currently we can minimize these unwanted changes by using different surgical techniques for bone promotion [1,2].
The main objective of alveolar preservation techniques is to limit the vertical and horizontal structural changes of the socket that occur after the extraction of the tooth, aiming to have a greater bone volume once the healing process is achieved, to facilitate a prosthetic rehabilitation as aesthetic and functional as possible after the insertion of the osseointegrated implants [3]. Despite all this, and even with the current alveolar preservation techniques, it is impossible to prevent a certain degree of reabsorption, which will occur regardless the procedure used [3,4].
Most of the proteins from their origin are common to bone, dentin, and cementum. Dentin, as we know, represents more than 80% of the tooth structure, contains bone morphogenetic, and non-collagen-derived proteins such as osteocalcin, osteonectin and phosphoproteins, that are all involved in the formation of bone architecture [4].
In humans, dentin has a mineral content much higher than any other bone derivative, in addition to being comparable with autogenous bone in two of its properties: it is osteocompatible and osteoconductive, which means that it is in a biological position to provide a scaffold for new bone formation by its inorganic component, and to provide various growth factors present in its organic part, reasons why we can consider dentin as an optimal biological and bioactive material for hard tissues regeneration. From the point of view of its composition, dentin has a 70% inorganic content and an organic content close to 30%, from which 90% is composed of collagen while in alveolar bone the inorganic content is 60% and organic is close to 25% [5,6].
Today we know that both teeth and alveolar bone derive from the neural crest cells and are composed of the same type of collagen, which is Collagen Type-I [7]. Therefore, we can consider our teeth as protein carrying elements that can behave like a conventional graft, since their composition and biological structure is very similar to alveolar bone. Osteogenesis, osteoinduction and osteoconduction are the main biological processes that make up the osseointegration. Osteogenesis is the process by which newly formed bone develops from osteogenic cells. Osteoinduction is the stimulation and activation of osteogenic cells in the tissue surrounding the injury, while osteconduction is the process by which the blood vessels that carry repair elements are developed [8].
We all accept that due to the histocompatibility and predictability of the conventional autologous grafts they are the best surgical choice for obtaining bone; however, they are not exempt from complications and limitations such as: the limited amount of graft material that we usually obtain, the morbidity of the donor area, the duration of the surgical intervention and the set of postoperative discomfort and complications.
This new clinical protocol that we apply today provides osteogenesis, by stimulating the process of bone tissue formation, it also induces osteoconduction by providing the osteoconductive capacity of the material it creates for osteogenic cells and osteoinduction by transforming perivascular undifferentiated mesenchymal cells into boneforming cells, in the presence of certain substances such as BMP-2 was the first researcher who published the realization of a human dentin autograft and found that the bone thus formed is stable and is suitable to be considered as an autologous graft [8,9].
Later, the same group proposed the use of dentin as a new biomaterial and a carrier of Bone Morphogenic Protein-2 (BMP-2) which, as we know, is involved in the bone formation process. These authors demonstrated that highly calcified tissues such as dentin do not generate early osteoinduction or the formation of spongy tissue [9]. They also found that, after demineralization of dentin, certain Bone Morphogenic Proteins (BMPs) remain bioactive, specifically BMP-2, BMP-4, and BMP-7, which bind in collagen rich matrices, as occurs physiologically in the bone [10].
In this respect, later studied the dentin structure according to its demineralization degree and found that bone regeneration using dentin graft highly depends on the mineralization of dentin used [11]. He observed that Completely Demineralized Dentin (CDDM) and Unmineralized Dentin (UDM) induced little bone formation, moreover CDDM was largely resorbed. Meanwhile Partially Demineralized Dentin (PDDM) or Demineralized Dentin Matrix (DDM) induced much more new bone formation. It is important to mention that both DDM and PDDM are interchangeable terms, because DDM is always partially demineralized [11].
A very interesting study made by analyzed and compared the composition of different bone graft materials, Tooth Derived Bone Substitute (TDBS) and human ramus bone. The teeth used in the study were extracted for orthodontic treatment, and the mandibular ramus parts were from healthy patients undergoing orthognathic surgery. The result of his investigation was that TDBS possesses the same chemical elements present in bone graft materials, such as Carbon (C), Calcium (Ca), Oxygen (O), Phosphate (P), Sodium (Na) and Magnesium (Mg) in addition to similar Ca/P ratio to that of the mandibular ramus, as well as the osteoinductive and osteoconductive properties [12]. Many researchers have been able to verify that, after the application of this protocol, an adequate healing process is produced, observed by radiological, histological, and clinical evaluation, and by the adequate integrity of the bone crest after more than 30 months of clinical follow-up [13,14].
Two recent studies, held in 2020, investigated the effect of using autogenous dentin in socket preservation prior to lower third molar extraction, in one study the authors divided the patients into control and test group, while in the other study into control and test sides, since the lower third molar extraction was performed into the two sides of the same patient. They measured the probing depth distal to the lower second molar months after the surgery, and the findings made both of them agree that the autologous grinded dentin helped in the socket preservation and lowered bone loss at the site of extraction [15].
The technical modifications made by the Binderman, et al. group have also represented a clear innovation by simplifying the protocol and conceiving it as we propose it today; in other words, to be able to be applied at the same moment of the extraction of the tooth. This author also considers that the main indication for this surgical technique are teeth to be extracted due to periodontal involvement and those teeth that are, as in our case, partially or totally included in the maxilla [16].
As it is a protocolized technique, whenever possible we must discard teeth with previous endodontic treatments or periapical surgery, as well as all those that present complex fillings, or with little remaining dental material, which could distort the final result of the treatment [16].
In 2007, the FDA approved the use of recombinant human Bone Morphogenic Protein-2 (rhBMP-2) to restore the bone defects related to extractions and in sinus and alveolar ridge augmentation. At first it was delivered in Absorbable Collagen Sponges (ACSs), which problem was the instability and the rapid release of rhBMP-2, this was overcomed when other studies proposed and demonstrated the hight capacity of the DDM to carry and control the release of the rhBMP-2 by sustaining its concentration at the bone formation site for a prolonged time.
A study made in the 2018 showed that the DDM can be much more effective if combined with exogenous rhBMP-2. The researchers in this study got the conclusion that the alveolar ridge preservation with DDM/rhBMP-2 has a synergistic effect on the bone formation [13, 17-19]
The demineralized dentin can also be used in the form of a shell to restore lateral bone defects. Used this technique and fixed the dentin shell with micro screws. It allowed larger augmentation volumes and promising results that provide us with new techniques to restore bone defects with autogenous and feasible material [20].
Case Report
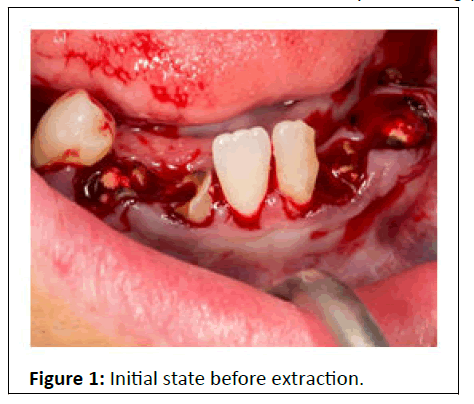
45-year-old male patient reported to the Teaching Unit of Oral Surgery of the University of Santiago de Compostela, Spain (USC), with the chief complaint of fracture and loss of multiple lower teeth, bad aesthetics, and difficulty in chewing (Figure 1).
The patient was asked about his medical history, and we found that there is no relevant medical condition. Clinical examination and cone beam computed tomography were performed.
We found multiple lower remaining roots with previous endodontic treatment, one premolar and two central incisors caries free, in addition to the compromised periodontal condition.
The remaining bone permits the placement of many dental implants, with the need of bone regeneration, in order to fabricate future implant supported overdentures, when the osteointegration is achieved.
We talked to the patient and agreed with him to perform the surgery the next week.
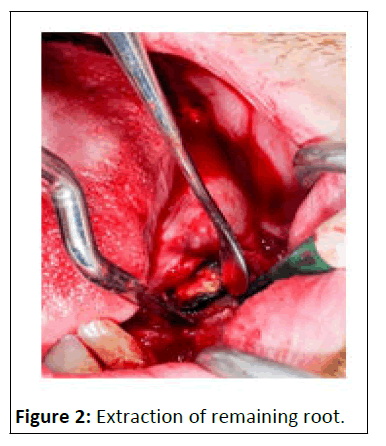
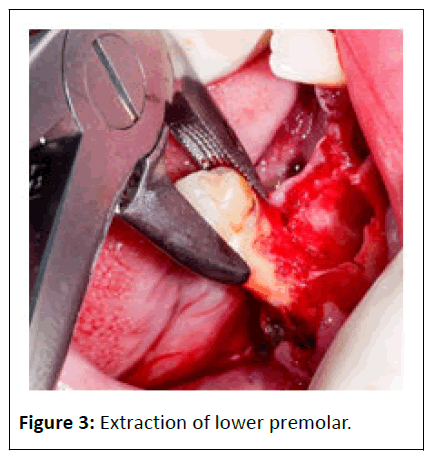
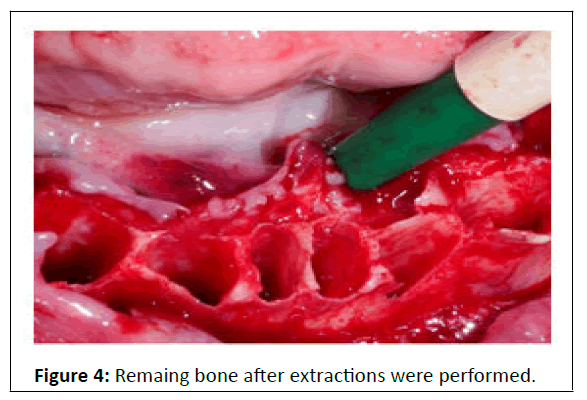
During the surgery, a ter conventional local anaesthesia for the inferior alveolar, buccal, and lingual nerves using 4% Articaine with 1:100,000 adrenaline, complete clearance of remaining roots and teeth was performed, with minimally traumatic extraction techniques (Figures 2- 4).
Sound teeth were then taken for the further procedures (Figure 5).
Meanwhile processing the extracted tooth surface, the alveolar socket is being irrigated continuously with saline to keep it moist and well hydrated.
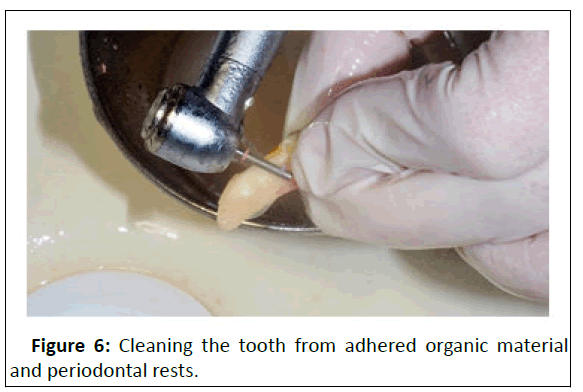
As the protocol used in several studies, the tooth is being cleaned with saline and polished to wash out all the organic material present on its surface from the remaining periodontal ligament, then the pulp tissue is removed gently using a diamond bur. We dried the surface with sterile gauze and air to prevent any oil contamination (Figure 6).
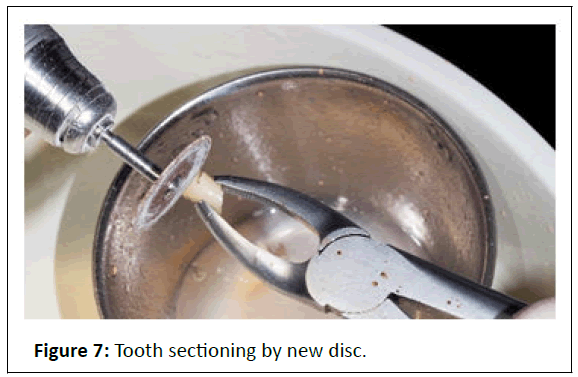
After that with a new disc we started to carefully section the tooth into small portions in order to avoid the blockage of the device with large tooth particles, especially during cutting the enamel in order to prevent deterioration and cracks. During the tooth handling we keep abundant irrigation with saline (Figure 7).
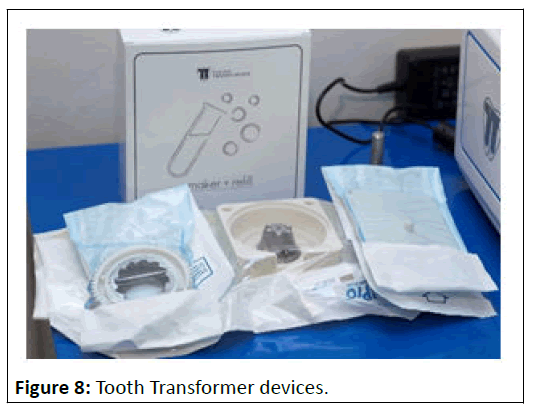
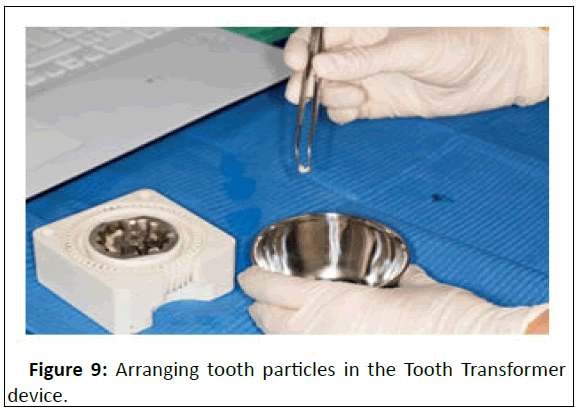
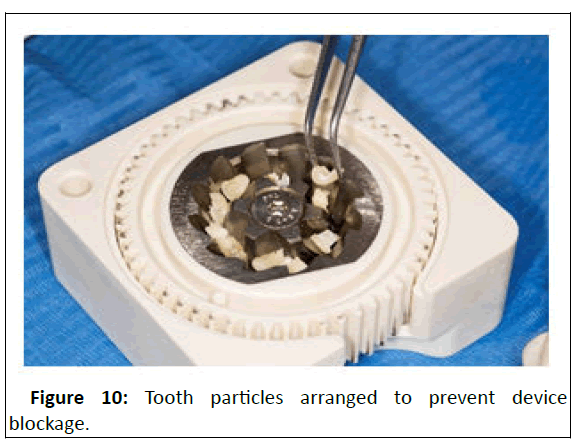
In our case we used the automated device Tooth Transformer that splits the tooth into portions between 0.4 to 0.8 millimeter, small tooth pieces were then inserted in the mill area of the device (Figure 8- 10).
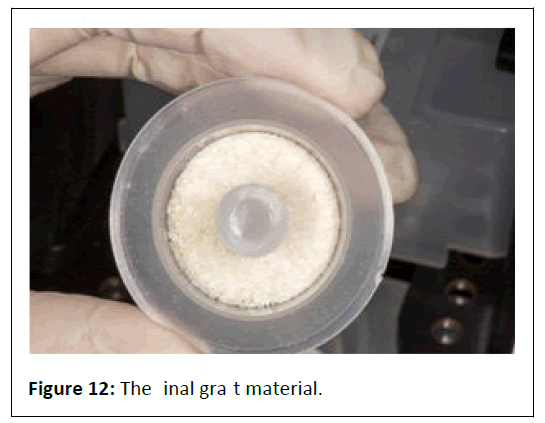
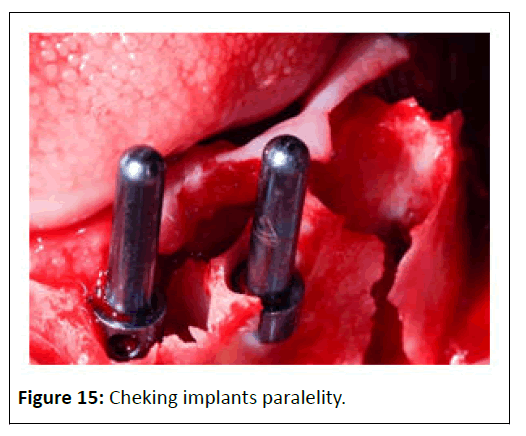
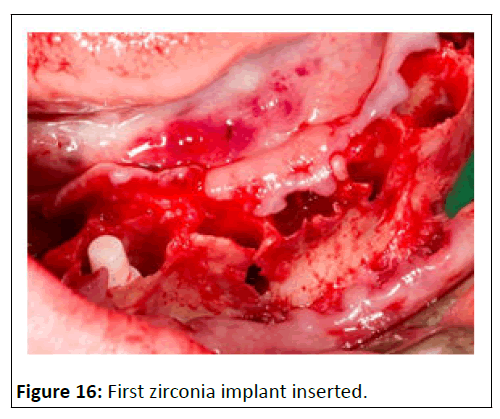
The whole process lasts 40 minutes approximately and after the grafting material is ready, we check that the particles diameter is between 300 and 1200 microns (0.3 to 1.2 millimeter) (Figures 11-16).
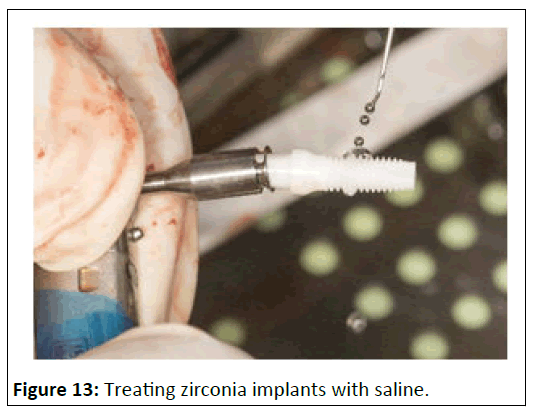
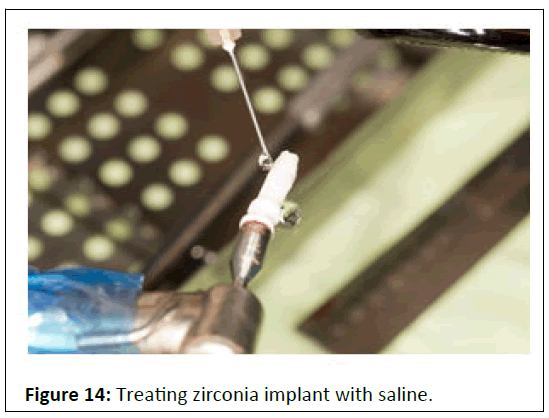
We had previously decided to use Zirconia implants due to its high biocompatibility, aesthetics properties and soft tissue integration [15-19].
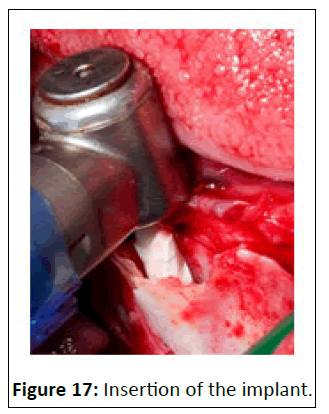
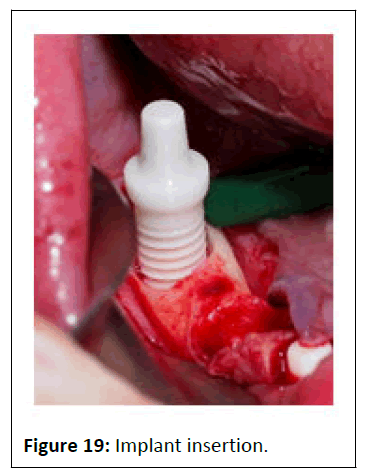
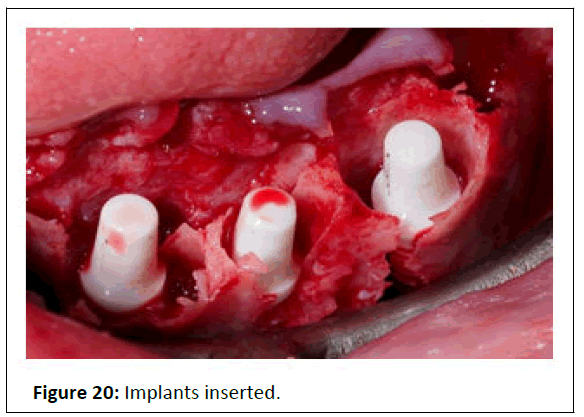
Saline solution is used to treat the surface of zirconia implant with the aim of reducing the quasi-static fracture strength (Figure 17-20).
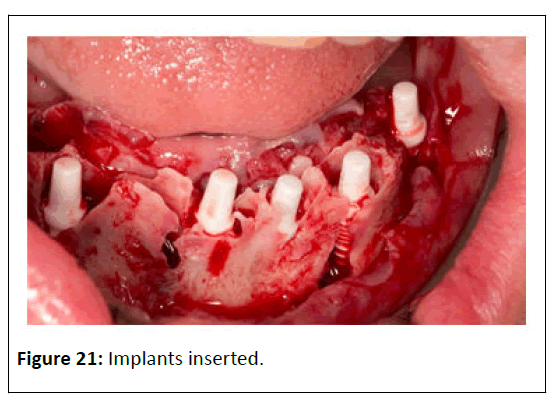
A ter that we started to place the implants. When implants were inserted into their places, and we insured that all have the adequate primary stability [13,14,21].
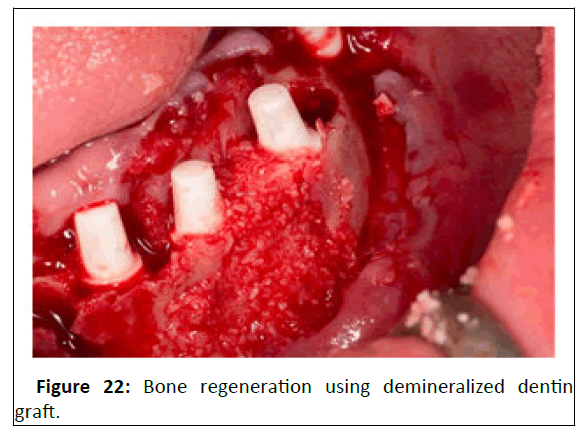
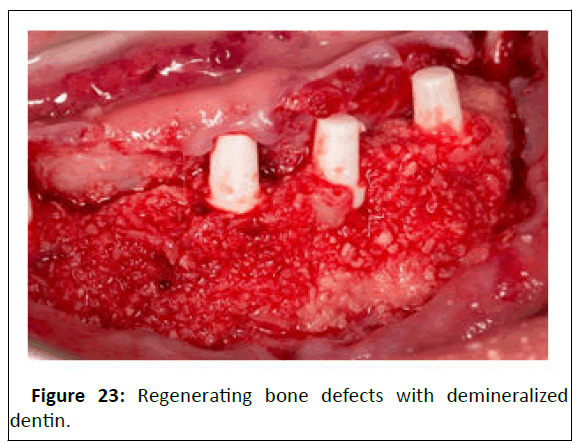
We began to fill all the bone defects with the prepared autologous tooth graft (Figure 21-23).
It is important to mention that the volume of the graft material obtained from the Tooth Transformer device is 2.5 times the volume of the grinded tooth, which provides us all the necessary amount of graft for the needed bone regeneration with feasible cost. We prefer to over contour the emergence profile by two or three millimeter, since months following the surgery certain degree of bone resorption will always occur [20-23].
We reposition the mucoperiosteal flap into its place and suture the site with monofilaments. By that our intervention is finished, now we will wait eight months until the implants are completely osseointegrated to continue with the prosthetic part of the treatment.
Discussion
Numerous authors in recent years have reported that the non-organic and organic composition of dentin is very close to that of bone tissue. Its organic matrix is also dominated by Collage fibres Type I and non-collagenous proteins, such as phosphoproteins, osteocalcin, proteoglycans, and glycoproteins. The most recent studies demonstrated that the dentin used in the form of particles or blocks exhibited osteoconductive and osteoinductive properties, which could therefore be considered a fundamental part of the bone remodeling process [7,22,23]. From the point of view of graft granulometry, there is also a disparity in criteria and thus, while a group of researchers use the particles protocol others use the block graft [24 -26].
Binderman, et al. research group used a clinical protocol similar to ours. In their histological studies, they were able to verify how the structure of the alveolar crest and the soft tissues remained unchanged in the short to medium term, with values similar to those obtained using autologous cortical bone or other biomaterials [4,16]. Calvo Guirado, et al. has also obtained higher values than conventional techniques in his studies, although it is necessary to consider that this study has been carried out in experimental animals, with the logical similarities but also the clear differences with the oral human environment [24].
Both Schwarz and Becker in their studies have used processed dentin root blocks, obtaining a more homogeneous replacement of bone compared to conventional autologous bone grafts, and this circumstance is because the dentin is remodelled very slowly compared to the most biomaterials [7,22,25,26].
It is undeniable that these studies highlight the structural and biological potential of dentin graft, as an alternative method to classical grafts. Now we can also say that new dentin graft material won’t only be used in oral rehabilitation, but it has also the potential of helping in extraoral bone regeneration.
In a recent study in 2021, authors used also the dentin blocks form, in the shape of Perforated Root-Demineralized Dentin Matrix (PR-DDM) to restore extraoral bone defects, specifically in a sheep iliac. The PR-DDM helped in the bone regeneration in the target site, it acted as a unique scaffold that was later absorbed by multinucleated giant cells [27].
As we mentioned before, DDM was used to carry rhBMP-2 to improve its regeneration capacity. When DDM serves as a porter, it combines the properties of the grafting material with those of the transported substances, therefore researchers started to use it as carrying element of other materials, like Metformin, the widely used antidiabetic drug. Gao X, et al. delivered the Metformin and Mesenchymal Stromal Cells (MSCs) in the DDM, and they were seeded in a high glucose medium. The result was satisfying and osteogenenic differentiation took place. Which means that in the future we will be able to offer more treatment options to diabetic patients [28].
The future is so bright, and we can overcome more problems facing the implant treatment by delivering the adequate substance in the new autologous carrier.
Although one of the aims of using DDM was to decrease the need of getting autologous grafts by the conventional methods, still sometimes we can do it to restore large volume defects. Like Umebayashi M, et al. who used Particulate Cancellous Bone and Marrow (PCBM) from the iliac bone and mixed it with equivalent amount of PDDM to rehabilitate maxillary alveolar bone [29].
It is obvious that this new graft material and regeneration techniques are great, however we still face some problems regarding this novel material.
One from the obstacles professionals can face is the relatively limited access to the autologous dentin, Jing X, et al. studied with his team the possibility of modifying the small, achieved amount of dentin by other materials to enhance bone formation, so he could adhere Bone Forming Peptide-1 (BFP-1) to the DDM surface using Carboxymethyl Chitosan (CMC), in order to synthesise new bone graft material. That latest graft material improved bone formation by increasing osteogenic differentiation of stem cells in vitro as well as in vivo [30].
Another difficulty of this regeneration method as proposed by is to determine the amount of BMP and Collagen Type I available after tooth processing, to establish the exact protocol before starting the treatment, and to decide which part or parts of the tooth we are going to use to obtain the best result and finally the human factor as it is not possible to standardize the procedures, nor the fluids used to correctly decrystallize BMP and Collagen Type I [31].
In our clinical case, using the Tooth Transformer protocol, we have obtained a granule size between 0.4 and 0.8 millimeter, this material volume does not vary over time under pressure, thus providing ideal qualities to achieve a homogeneous, vascularized and well mineralized regeneration.
It seems that the promising material in dental practice is the demineralized dentin, since the researchers always discover new uses of it. Ku JK, et al. and his team fabricated a membrane to substitute the collagen membrane from autogenous demineralized dentin matrix in the form of block, in order to overcome the instability of the commonly used collagen membrane. In addition to the advantages of collagen membrane, this new membrane type provided osteoinductive property and higher mechanical and clot stability. Still many studies are needed to widely use this new membrane [32].
The future is so promising, maybe it is time not only to talk about the advantages and uses of DDM, but also of the possible application of allogenic DDM. Um, et al. and his colleagues represented the first comprehensive study concentrating on the osteoinductivity and antigenicity of the allogenic DDM [33]. They concluded that except for the initial inflammation reaction, Allo DDM has no or low antigenicity. Although in the study of Bakhshalian, et al. two days postoperatively WBCs count was higher in the Allo DDM group, this level reached equivalence later, which means that it is not related to immunological reaction [34]. In his most recent study on this topic used Allo DDM in the management of maxillofacial bone defects, and the result was encouraging in terms of osteoinductivity, although occasional antigenicity may occur [35]. The current limitation of the use of Allo DDM in vivo is the risk of viral disease transmission, further studies are needed to approve its wide use [33-35].
Conclusion
Demineralized dentin graft is a new therapeutic option for clinical cases in which we need a significant amount of graft. Despite the lack of clinical and experimental studies in the medium and long term, we believe that a suitable graft material can be obtained, due to its composition almost identical to that of human bone in calcium and phosphorus ions organized in the form of hydroxyapatite and TCP.
We know that its organic part contains large amount of type I collagen and growth factors, in addition to its characteristic organization in microtubules that will promote bone growth and make easier the osteoconduction, at the same time it demonstrated higher behaviour than that of xeno derivatives and other graft types.
With the studies we have at the moment, that as we mentioned before are limited, we can affirm that autologous dentin graft does not provoke any immune reaction, that is why its biological and funcional incorporation fast, effective and predictable examination.
References
- Ten Heggeler JM, Slot DE, Weijden GA (2011) Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: a systematic review. Clin Oral Implants Res 22:779-788
- Zhang S, Li X, Qi Y, Ma X, Qiao S, et al. (2021) Comparison of Autogenous Tooth Materials and Other Bone Grafts. Tissue Eng Regen Med 18:327-341
- Pagni G, Pellegrini G, Giannobile WV, Rasperini G (2012) Postextraction alveolar ridge preservation: biological basis and treatments. Int J Dent 2012:151030
- Diaz C, Del A (2016) Use of autologous dental material as a graft in the post-extraction socket. TFM
- Goldberg M, Kulkarni AB, Young M, Boskey A (2011) Dentin: structure, composition and mineralization. Front Biosci (Elite Ed) 3:711-35
- Clarke B (2008) Normal bone anatomy and physiology. Clin J Am Soc Nephrol. 3:131-139
- Kim YK, Kim SG, Byeon JH (2010) Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:496
- Guirado JC, Fernandez M (2019) Use of dentin as a biomaterial for bone filling. El dentista moderno 38-43
- Murata M, Um I, Kim K, Mitsugi M, Akazawa T, et al. (2011) Human dentin as novel biomaterial for bone regeneration. InTech 12-48
- Al-Namnam NM, Shanmuhasuntharam P, Ha KO, Siar CH (2010) Processed Allogenic Dentine as A Scaffold for Bone Healing: An in vivo study. Aust J of Basic and Appl Sci 4:5932-5940
- Gao X, Qin W, Wang P, Wang L, Weir MD (2019). Nano-Structured Demineralized Human Dentin Matrix to Enhance Bone and Dental Repair and Regeneration. Appl Sci 9:1013-1013
- Khanijou M, Zhang R, Boonsiriseth K, Srisatjaluk RL, Suphangul S, et al. (2021) Physicochemical and osteogenic properties of chairside processed tooth derived bone substitute and bone graft materials. Dent Mater J 40:173-183
- Kim BJ, Kim SK, Lee JH (2021) Bone regeneration of demineralized dentin matrix with platelet-rich fibrin and recombinant human bone morphogenetic protein-2 on the bone defects in rabbit calvaria. Maxillofac Plast Reconstr Surg 43:34
- Dlucik R, Wylegala OB, Dlucik D, Puzzolo D, Micali A (2021) Socket preservation or guided bone regeneration - a case report. Pol Merkur Lekarski 49:153-157
- Labrador SL, Ares M, Aranegui OR, Quiles LJ, González JM (2020) Autogenous Dentin Graft in Bone Defects after Lower Third Molar Extraction: A Split-Mouth Clinical Trial. Materials (Basel) 13:3090
- Binderman I, Hallel G, Nardy C, Yaffe A, Sapoznikov L (2014) a Novel Procedure to Process Extracted Teeth for Immediate Grafting of Autogenous. D J Interdiscipl Med Dent Sci 2:154
- Um I-W, Kim Y-K, Park J-C, Lee J-H (2018) Clinical application of autogenous demineralized dentin matrix loaded with recombinant human bone morphogenetic-2 for socket preservation: A case series. Clin Implant Dent Relat Res 1–7
- Um IW, Ku JK, Lee BK, Yun PY, Lee JK, et al. (2019) Postulated release profile of recombinant human bone morphogenetic protein-2 (rhBMP-2) from demineralized dentin matrix. J Korean Assoc Oral Maxillofac Surg 45:123-128
- Um IW, Ku JK, Kim YK, Lee BK, Leem DH, et al. (2020) Histological Review of Demineralized Dentin Matrix as a Carrier of rhBMP-2. Tissue Eng Part B Rev 26:284-293
- Korsch M (2021) Tooth shell technique: A proof of concept with the use of autogenous dentin block grafts. Aust Dent J 66:159-168
- Yona SK, Ozcan M, Godinger A, Basso N, Rittel D (2019) Random spectrum fatigue of zirconia oral implants in air and saline solution. Eng Fail Anlys 106:104160
- Lindhe J (2000) Clinical periodontology and dental implantology. Ed Panamericana:Madrid 604-654
- Andersson L (2010) Dentin xenografts to experimental bone defects in rabbit tibia are ankylosed and undergo osseous replacement. Dent ramtlgy 26:398-402
- Guirado CJL (2017) New procedure to process the extracted teeth as a graft in post-extraction sockets. Gaceta Dental 290:96-113
- Schwarz F, Golubovic V, Mihatovic I, Becker J (2016) Periodontally diseased tooth roots used for lateral alveolar ridge augmentation. A proof-ofconcept study. J Clin Periodontol 43:797-803
- Becker K, Drescher D, Honscheid R, Golubovic V, Mihatovic I, et al. (2017) Biomechanical, micro-computed tomographic and immunohistochemical analysis of early osseous integration at titanium implants placed following lateral ridge augmentation using extracted tooth roots. Clin Oral Implants Res 28:334-340
- Kabir MA, Murata M, Shakya M, Yamada K, Akazawa T (2021) Bio-Absorption of Human Dentin-Derived Biomaterial in Sheep Critical-Size Iliac Defects. Materials (Basel) 14:223-223
- Gao X, Qin W, Chen L, Fan W, Ma T, et al. (2020) Effects of Targeted Delivery of Metformin and Dental Pulp Stem Cells on Osteogenesis via Demineralized Dentin Matrix under High Glucose Conditions. ACS Biomater Sci Eng 6:2346-2356
- Umebayashi M, Ohba S, Kurogi T, Noda S, Asahina I (2020) Full Regeneration of Maxillary Alveolar Bone Using Autogenous Partially Demineralized Dentin Matrix and Particulate Cancellous Bone and Marrow for Implant-Supported Full Arch Rehabilitation. J Oral Implantol. 46:122-127
- Jing X, Xie B, Li X, Dai Y, Nie L, et al. (2021) Peptide decorated demineralized dentin matrix with enhanced bioactivity, osteogenic differentiation via carboxymethyl chitosan. Dent Mater 37:19-29
- Beca Campoy T (2019) Vertical fracture: Socket Shield and autologous dentin graft. RCOE 24:22-30
- Ku JK, Um IW, Jun MK, Kim IH (2021) Dentin-Derived-Barrier Membrane in Guided Bone Regeneration: A Case Report. Materials (Basel) 14:2166
- Um IW, Lee JK, Kim JY, Kim YM, Bakhshalian N, et al. (2021) Allogeneic Dentin Graft: A Review on Its Osteoinductivity and Antigenicity. Materials (Basel) 14:1713
- Bakhshalian N, Jalayer T, Shahoon H, Arjmandi BH, Azimi HR (2013) Osteopromotive property of allogenic demineralized dentin matrix: a pilot study. J West Soc Periodontol Periodontal Abstr 61:35-38
- Ku JK, Jeong YK, Um IW (2021) Review of Allogeneic Dentin Graft for Maxillofacial Bone Defects. Tissue Eng Part C Methods 27:472-480

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences