Spinal Epidural Abscess Causing Cauda Equina Syndrome: A Case Report
Konstantinos Barkas, Emmanouel Chatzidakis, Panagiotis Zogopoulos and Moschos Fratzoglou
| Konstantinos Barkas, Emmanouel Chatzidakis, Panagiotis Zogopoulos* and Moschos Fratzoglou Department of Neurosurgery, General Hospital of Nikaia-Piraeus “Agios Panteleimon”, Athens, Greece |
| Corresponding Author: Panagiotis Zogopoulos, Vosporou Str, Athens, PO Box: 10444, Greece. Tel: 0030697-6053555, 0030210-5128632; E-mail: p.zogopoulos@yahoo.com |
| Received: January 25, 2016 Accepted: March 03, 2016 Published: March 05, 2016 |
Abstract
We present the case of a patient with low back pain who rapidly progressed to cauda equina syndrome due to an extended epidural abscess of the thoracic, lumbar and sacral spine. The patient was successfully treated with surgical decompression through laminectomies at L1, L3 and L5 levels and surgical drainage of the epidural pus. Six-week course of intravenous antibiotic therapy followed. At 6-month follow-up examination, complete return of extremity motor function was demonstrated and the patient reported resolution of pain. Although, medical treatment with or without aspiration of the epidural space is increasingly used in patients without neurological deficits, in those with neurological deficits the importance of early decompression and debridement of infected tissues should be emphasized. A minimal surgical technique can be adequate for pus drainage as well as for preventing spinal instability in the setting of an extended spinal epidural abscess.
Keywords |
||||
| Cauda equina syndrome; Psoas abscess; Spinal epidural abscess | ||||
Introduction |
||||
| Spinal epidural abscess (SEA) was first described in the medical literature in 1761 and nowadays it comprises 0.2 to 2 cases per 10,000 hospital admissions [1]. The most common risk factors are diabetes mellitus, trauma, intravenous drug abuse and alcoholism. Other common risk factors include the presence of nonspinal infection (including skin abscesses and furuncles as well as endocarditis), conditions involving chronic immunosuppression and epidural anesthesia or analgesia [1-3]. SEA is a rare but potentially devastating entity harboring a significant morbidity, as well as, mortality. The essential problem is the necessity of early diagnosis since it is usually ignored in the preliminary differential diagnosis of low back pain and as a result, appropriate treatment may be delayed. Although, surgical decompression and antibiotics are the cornerstones of therapy, it cannot be overemphasized that only timely treatment is able to avoid or reduce permanent neurological deficits. Therefore, we emphasize the necessity of a high alertness regarding the clinical deterioration of patients with spinal epidural abscess, allowing for a timely surgical decompression. | ||||
Materials and Methods |
||||
| A 50-year-old woman presented to the outpatient clinic of our department suffering from a left sciatica and “foot drop”. She reported a fall 45 days prior with a subsequent fracture of the coccyx followed by a one-month history of progressive left sciatica, as well as, a left thigh weakness and gait disturbance starting 20 days ago. She also complained of slight malaise and dysuria during the last few days. In her medical history she reported an abnormal glucose tolerance test. | ||||
| On examination she was an overweight lady unable to perform left foot extension and she complained of pain in the thigh when the left leg was elevated. She presented positive Lasegue sign in 300 at her left limb and the left quadriceps muscle strength was 3/5. The left knee jerk reflex was diminished and the ipsilateral Achilles tendon reflex was absent. There was no saddle anesthesia, the anal tone was normal and there was decreased sensation in the distribution of L5 and S1 dermatomes. Muscle strength and tendon reflexes of the right limb were normal and the sensation was intact. The examination of the cranial nerves and upper extremities was normal. | ||||
| The general examination revealed a temperature of 37.8°C while there were no signs of lymphadenopathy, tonsillitis, sinusitis, otitis or upper respiratory infection, there were no heart murmurs and there were no skin abscesses, furuncles or signs of perianal infection. There was a slight sensitivity in the left inferior quadrant of the abdomen and a positive Giordano’s sign ipsilaterally. Her leukocyte count (WBC) was 22,000/mm3 (86% Poly), C-reactive protein (CRP) was 370 mg/ml, Erythrocyte Sedimentation Rate (ESR) was 70 mm/h and serum glucose was 221 mg/dl. The urine sample showed pyuria along with the presence of glucose, protein, hemoglobin and ketone bodies. | ||||
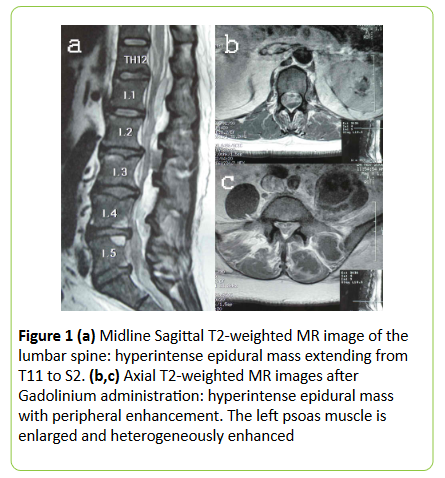
| Owing to the manifestations of fever, pyuria and low back pain, we immediately commenced empirical antibiotics administration (after urine specimen was sent for culture), suspecting an acute pyelonephritis. A few hours later, the patient deteriorated with signs of cauda equina syndrome. A lumbar MRI scan was performed in an emergency basis and it revealed a multilevel spinal epidural mass extending from T11 to S2 which was isointense in T1-weighted images, hyperintense in T2-weighted images and enhanced peripherally after Gadolinium administration. The left psoas muscle was enlarged and heterogeneously enhanced, the ipsilateral paraspinal muscles were also enlarged and there were no signs of spondylodiscitis (Figure 1). | ||||
| The diagnosis of a spinal epidural abscess, as well as, a left psoas muscle abscess was made. A whole-spine MRI that was performed, in order to exclude the possibility of involvement of other sites of the spinal canal was without any significant findings. | ||||
| The patient underwent an emergent operation for decompression of the spinal cord and surgical drainage of the abscesses (both the epidural and that of the psoas muscle). Specifically, laminectomies at L1, L3 and L5 were performed and the pus was drained with the use of a silicon catheter which was inserted caudally and cranially into the epidural space, through each laminectomy site, in order to avoid spinal instability and to achieve pus drainage over the entire extent of the abscess (T11 to S2). | ||||
| The organism cultured from the pus was Staphylococcus aureus, multisensitive to antibiotics which appeared to be the same species that was cultured in the patient’s urine sample. The patient was put under intravenous administration of clindamycin for 2 weeks followed by oral administration for another 6 weeks. | ||||
Results |
||||
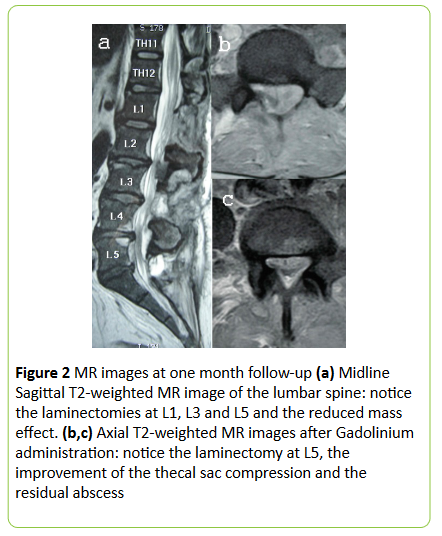
| The postoperative course was uneventful and the patient had a remarkable improvement of her general, as well as, her neurological condition. She suffered a mild fever for almost a month, the WBC returned gradually to normal within 2 weeks, while the CRP and ESR returned to normal after 30 and 50 days respectively. Radiological improvement was noticed in the MRI that was performed at one month (Figure 2) and the patient was discharged without low-back pain or sciatica and only minimal weakness of plantar flexion. | ||||
| At 6-month follow-up examination, the patient was in an excellent general condition, reported resolution of pain and complete return of extremity motor function was demonstrated. The MRI of the lumbar spine and abdomen demonstrated radiological diminution of the spinal lesion, and the psoas abscess remnants were gradually diminished. At 1- year follow-up the psoas abscess had disappeared and the patient was in an excellent neurological condition. | ||||
Discussion |
||||
| It is our impression that in this patient the fracture of the coccyx produced a local hematoma that, due to the latent diabetes mellitus, was the substrate of Staphylococci colonization [4,5]. The psoas abscess gave rise to the spinal epidural abscess through the neural foramina and due to the close relation to the ureter the infection contaminated the urinary tract. | ||||
| Despite the patient’s neurological status prior to surgery the outcome was excellent. The immediate surgical decompression yielded a good neurological outcome and the minimal surgical technique with laminectomies at nonadjacent levels was adequate for pus drainage as well as for preventing spinal instability. | ||||
| The incidence of SEA has been doubled in the past two decades, probably owing to an aging population, increasing use of spinal instrumentation and vascular access as well as the spread of injection-drug use [1-3,6]. Although, the source of infection is not identified in many patients, it seems that most cases arise from hematogenous seeding of the epidural space from a distant source of infection and a few cases are the result of direct extension of infection from the spine or paraspinal tissues. | ||||
| The patients usually present with motor or sensory deficits, with pain alone or less frequently with sepsis [7]. Of special notice is the fact that patients with pyogenic SEA may progress to complete paralysis within minutes to hours, even while receiving optimal antibiotic therapy. The pathophysiological background of the clinically significant effects of the epidural abscess seems to be mostly from involvement of the vascular supply to the spinal cord and subsequent infarction rather than direct compression [1,2,6,8]. | ||||
| The routine laboratory studies should include WBC count, blood cultures, ESR and CRP. The WBC count will show leucocytosis with polymorphonuclear predominance in more than two thirds of the patients, while, ESR and CRP will be increased in almost all of them [8]. Blood cultures might be able to determine the pathogen. Spinal epidural abscess is primarily a bacterial infection, and the gram-positive Staphylococcus aureus is the most common organism cultured from abscesses, though many other bacteria have been implicated, including Staphylococcus and Pseudomonas species, Escherichia coli and Mycobacterium tuberculosis. Methicillin-resistant Staphylococcus aureus (MRSA) is increasingly reported, particularly in patients after spinal surgery with implanted devices [1]. | ||||
| Plain x-ray films are usually nonspecific and MRI, if available, is the imaging modality of choice [9]. In T1 weighted images SEA appears iso- to hypointense to the spinal cord, in T2 weighted images it is hyperintense and is strongly enhancing in T1 with Gadolinium. Although, lumbar puncture is relatively contraindicated, because it entails the risk of spreading bacteria into the subarachnoid space with consequent meningitis, if MRI is unavailable, CT myelography or conventional myelography can reveal an intraspinal extramedullary mass. In cases of suspected SEA the whole spine should be scanned by MRI to exclude the possibility of multilevel involvement. | ||||
| Medical treatment with or without aspiration of the epidural space is increasingly used in patients without neurological deficits. On the other hand, when neurological deficits are present, the importance of early decompressive laminectomy and debridement of infected tissues should be emphasized since the preoperative neurological stage is the most important predictor of the final neurological outcome and the rate of progression of neurological impairment is difficult to predict. About 5% of patients with spinal epidural abscess die, usually because of uncontrolled sepsis, evolution of meningitis, or other underlying illnesses [3]. | ||||
| The usual duration of antibiotic therapy is at least 6 weeks because vertebral osteomyelitis exists in most patients with spinal epidural abscess [10]. Since, noncompliance and limited bioavailability may impede the effectiveness of oral therapy, intravenous administration of antibiotics is preferred. | ||||
Figures at a glance |
||||
|
||||
References |
||||
|

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences