Hairy Cell Leukemia - Case Reports
Karla Hernández-Ruano, Diana Morales-Santos, Polet Portillo-Cálix, Jorge Escoto- Theodoracopoulos and Cristian Alvarado-Medina
Karla Hernández-Ruano1,Diana Morales-Santos2,Polet Portillo-Cálix3,Jorge Escoto-Theodoracopoulos4 and Cristian Alvarado-Medina5
1Medical Doctor, Universidad Nacional Autónoma de Honduras.
2General Doctor, Health Center Ojojona, Francisco Morazan
3Forensic Physician, Dirección de Medicina Forense/Ministerio Público, Honduras
4Emergency Chief Hospital, Santo Hermano Padre, Catacamas, Olancho, Honduras
5Hemato-Oncology Department and Blood Bank Department, Hospital Escuela Universitario, Honduras
- *Corresponding Author:
- Diana Morales-Santos
General Doctor, Health Center Ojojona, Francisco Morazan, Honduras.
Tel: (504)32419696
E-mail: morales.diana88@gmail.com
Received date: March 10, 2016; Accepted date: May 21, 2016; Published date: May 30, 2016
Citation: Hernández-Ruano K, Morales-Santos D, Portillo-Cálix P, et al. Hairy Cell Leukemia - Case Reports. Med Case Rep. 2016, 2:2.
Abstract
Hairy cell leukemia (HCL) is a lympho-proliferative disease with an indolent course that is located within the group of mature B-cells neoplasias. It represents 2 to 3% of all leukemias types, with an estimated incidence of 600 and 1600 cases per year in the United States and Europe, respectively. It is characterized by persistent bicytopenia and splenomegaly. We present two cases of different gender, treated at Hospital Escuela Universitario located in the city of Tegucigalpa, Honduras, with clinic symptoms marked by weight loss and chronic fatigue. Hematological tests indicated pancytopenia and an abdominal ultrasound splenomegaly; followed by bone marrow biopsy that morphologically suggested hairy cells. Flow cytometry analysis, determined the diagnosis of hairy cell leukemia, that was treated with interferon and rituximab (in one of the cases), with a satisfactory clinical outcome. HCL diagnosis is sometimes difficult, because it is a disease with an indolent course and is often confused with other lympho-proliferative processes. Patients have a good prognosis and clinical improvement if the disease is detected and treated early. Here we present the sequence of events with their results and a literature review.
Keywords
Hairy cells; Splenomegaly; Cytopenia; Rituximab; Cladribine
Introduction
Hairy Cell Leukemia (HCL) was first described in 1920 [1-3] and had different denominations (leukemic reticuloendotheliosis, histiocytic leukemia, malignant reticulosis, y-lymphoid mielofibrosis). Recognized as a clear clinical and pathological entity by Bouroncle and colleagues in 1958 [4,5].
According to the World Heatlh Organization (WHO), HCL is a lympho-proliferative disease, classified within mature B-cell neoplasias of indolent course that is characterized by bicytopenia, splenomegaly and the presence of hairy cells in bone marrow and peripheral blood samples. It represents 2 to 3% of all leukemia types [6,7] with an estimated incidence of 600 and 1600 cases per year in The United States and Europe, respectively. Related to gender, it’s more often to be found in men, with a 4:1 ratio, and a median age of 52 years [8].
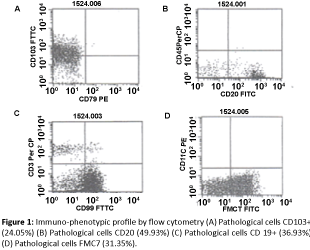
Immuno-phenotype through flow cytometry, comprehends B cell expression of CD20, CD22y CD11c, and T cell expression of CD103, CD25, CD123, CD72 y FMC7 [9,10] On treatment, there is an agreement, aiming a complete disease remission, because it is a chronic disease with an excellent prognosis. Initial treatment consists of purine analogues (cladribine and pentostatin) [11] and monoclonal antibodies like rituximab in case of relapse and treatment resistance [12]. The aim of this article is to release one of the first cases of this type of leukemia in Honduras, given it is a rare entity, of a chronic course and prevalent in male. However, treatment therapies have transformed it into a highly treatable disease with a normal life expectancy for patients.
Case No. 1
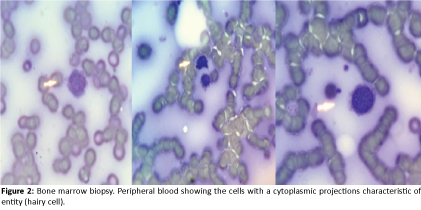
73 year old male patient, black ethnicity from Comayagua, Honduras (north central), former worker of a soap factory, with a history of fatigue, weight loss and diagnosed with Non Hodgkin lymphoma, who had received chemotherapy, presented recurrent pneumonia and persistent bicytopenia, that led to at least 3 hospital admissions, being referred to hematooncology department at Hospital Escuela Universitario for study. Clinically he presented high fever 40°C, bilateral crackles in both lungs, increase in abdominal circumference due to massive splenomegaly. Blood samples revealed pancytopenia (hemoglobin 7.7 g/dl, hematocrit 23.5%, platelets 86,000/mm3, White blood cells 4.8 × 103/mm3) y Lactate dehydrogenase 586 U/L. Abdominal ultrasound reported splenomegaly of 13.4 cm and hepatomegaly of 16 cm. Bone marrow biopsy highlighted diffuse infiltration of small, round cells, morphologically suggesting hairy cells, which formed over 50% of the erythroid and myeloid cells. The flow cytometry analysis observed a group of lymphoid B cells, evidence of a lymph proliferative syndrome (Figure 1) resulting positive CD103, CD19, CD20, FMC7, establishing diagnosis of Hairy Cell Leukemia and dismissing the previous diagnosis of Non Hodgkin Lymphoma. Treatment began with Interferon 5 MU SC, 3 times a week and later on added Rituximab on initial doses of 500 mg IV each 21 days. Given the good clinical evolution, outpatient management was established, keeping the patient stable for 3 weeks and relapsing due to a severe pneumonia, deciding to start a second dose of Rituximab, with a satisfactory result. The patient continues monitoring, with excellent outcome 2 months after relapse.
Case No. 2
A 67 year old female patient, from a village located in Francisco Morazán, Honduras previously diagnosed and treated for Chronic Lymphocytic Leukemia (CLL), with history of one year of chronic fatigue, hematomas in upper and lower limbs and weight loss. With these symptoms she went to a private clinic, where blood tests showed hemoglobin of 10.6 g/dl, hematocrit of 33%, platelets 94,000/mm3, white blood cells 1.59 × 103/mm3. Referred to the hemato-oncology department of Hospital Escuela Universitario for study, findings in physical examination were splenomegaly. Abdominal ultrasound reported splenomegaly of 13.3 cm. Bone marrow biopsy revealed mononuclear cells with a basophile cytoplasm and circumferential projections suggesting hairy cells (Figure 2). Flow cytometry had presence of CD20, CD19, CD103, FMC7; compatible with hairy cell leukemia, dismissing the previous diagnosis of CLL. Treatment began with alpha Interferon 3 MU, 3 times a week. She was given outpatient management, with slightly side effects from medication, without presenting recurrent infections, with a good clinical outcome. Patient continues monitoring every 3 months with the Hematooncology department at Hospital Escuela Universitario.
Discussion
Frequent symptoms described in Hairy Cell Leukemia are weakness and fatigue; findings in patients are splenomegaly in 96% of cases and hepatomegaly in 58% of cases. However, this disease is usually diagnosed early, as a result of abnormalities found in blood tests, like pancytopenia which is present in all patients at the moment of diagnose [7]. In these case reports, both patients presented chronic fatigue as an initial symptom, added to this, splenomegaly and hepatomegaly demonstrated by ultrasound and pancytopenia in blood samples. It’s still unknown and under study, why male gender has a higher ratio 4:1 and it can be present at any age in adulthood.
Epidemiologically, it is associated with jobs that expose to fuel, organic dissolvent, farming, pesticides and herbicides, with our male patient; he has as a background working in a soap factory, being constantly exposed to chemical components that may be related to the development of this disease. Also the presence of the BRAF V600E mutation recently has been described in this type of neoplasia, with a prevalence of 85% of the cases, demonstrating to be an oncogenic controller 5. In Honduras, resources are limited for the genetic testing, not making it possible to identify or demonstrate this genetic mutation on patients.
The diagnosis of HCL must be precise and detailed, because the clinical profile of this disease can imitate other lymphoproliferative B cell syndromes. In both patients, bone marrow biopsy was done as a first step and then proven with flow cytometry, which has a high sensibility, where patients with the classic form of this disease have a clear inmuno-phenotypical profile in their malignant leukemic cells: CD20+, CD19+, CD11c+, CD25+, CD103+ and CD123. It is also worth mentioning HCL has a variant form, included by the WHO, as a provisional entity, due to its clinical and pathological characteristics, that vary from HCL, Classic HCL is always positive for CD25 y CD103 and its variant is negative for CD25 and occasionally positive for CD103 y CD123. This difference is therapeutically important; because patients with variant type of HCL are resistant to treatment with alpha interferon they do not have a good outcome with conventional therapy [13].
The patients described in this report, started treatment with rituximab, because cladribine is unavailable in Honduras. Usually, patients respond to initial treatment with cladribine, some patients using rituximab present recurrence. Diverse studies, like the Cervetti et al., demonstrated that schemes with rituximab 4 through 8 cycles are highly effective in eradicating hairy cells by the end of the treatment, but it suppresses the immune system and promotes the development of infections during treatment [14]. It’s important to consider that a monoclonal antibody (anti- CD20) has advantages in the security profiles, tolerability and low medullar toxicity.
The use of Interferon has demonstrated capability to alter the clinical course of the patients with this rare leukemia form since its introduction in 1984. However, the mid survival rate was only 4 years. Though, it is not the first line treatment, it is used as an initial therapy to improve hematological parameters and immunesuppression control. Cladribine produces a longer remission, so the use of Interferon in HCL is limited.
In most patients, Interferon has been part of the initial therapy, helping the spleen reduce its size. The diagnosis of HCL can be difficult, due to its indolent course and it may be confused with other similar diseases and that it only represents 2% of all leukemia forms. Nevertheless, an abnormal blood count that indicates bicytopenia, associated to unspecific symptoms such as fatigue, splenomegaly, must bring suspicion of this type of clinical entities, and refer patients to Hemato-oncologists as soon as possible, for bone marrow tests that may lead to a proper diagnosis and a prompt pharmacological treatment, given the excellent response to interferon, purine analogues and monoclonal antibodies.
References
- Bustamante, Rodriguez M, Ocqueteau M, Bertin P (2010) Hairycellleukemiaduringpregnancy. Clinical case. Red Med Chile 130:1422-1426.
- Monnereau A, Slager L, Hughes M, Smith A, Glimelius B, et al. (2014) Medical history, lifestyle, and occupationalriskfactorsforhairycellleukemia: TheInterLymph non-Hodgkinlymphomasubtypesproject. Journal of theNationalCancerInstitute – Monographs14:115-124.
- Solessi S, Ledesma I, Aliano R, Bezares F (2012) Hairy cell leukemia:therapeutic strategy. Hematología 16: 33-41.
- Grever M, Blanchy S, Andritsos A (2014) Hairy cell leukemia: update on molecular profiling and therapeutic advances. Blood reviews 28: 197-203.
- Grever M (2010) How I treat hairy cell leukemia. Blood 115: 21-27.
- Lopez-Rubio M, Garcia-Marco J (2015) Current and emerging treatment options for hairy cell leukemia. OncoTargets and therapy 8: 2147- 2155.
- Payandeh M, Sadeghi M, Sadeghi E (2015) Hairy cell leukemia: A retrospective study on 11 patients in the Western Iran. IJHOSCR 9: 133-136.
- Gonzales-RodriguezT, Vargas-Ruiz A, Lopez-Karpovitch X (2012) Respuesta Terapéutica y supervivencia en pacientes con leucemia de células peludas en un hospital de tercer nivel. GacMedMex 148: 425-429.
- Rudolf-Oliveira M, Pirolli M, Santos de Souza F, Michels J, Santos-Silva C (2015) Hairy cell leukemia variant: the importance of differential diagnosis. Rev Bras HematolHemoter 37:132-135.
- Gaman A, Dobrea M, Gaman M (2015) A case of hairy cell leukemia variant. Rom J MorpholEmbryol 56:553-556.
- Naik R, Saven A (2012) My treatment approach to hairy cell leukemia. Mayo clinproc87: 67-76.
- Kaushansky K, Lichtman M,Kipps T,Seligsohn U,Prchal J et al. (2010) William’s hematology. (8thedn). McGraw-Hill.
- Robak T, Matutes E, Catovsky D, Zinzani P, Buske C (2015) Hairy cell leukaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann oncol 26: 100-107.
- Cervetti G, Galimberti S, Andreazzoli F (2004) Rituximab as treatmentforminimal residual disease in hairycellleukaemia. Eur J Haematol 73: 412–417.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences