Vertebral Artery Transection in Non-Penetrating Cervical Spine Injury: A Case Report
Chi-Man Yip, Jui-Hsun Fu, Shuo-Hsiu Hsu and Shu-Shong Hsu
DOI10.21767/2471-8041.100054
Chi-Man Yip1, Jui-Hsun Fu2, Shuo-Hsiu Hsu2 and Shu-Shong Hsu1
1Division of Neurosurgery, Department of Surgery, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, Republic of China
2Department of Radiology, Section of Neuroradiology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, Republic of China
- *Corresponding Author:
- Chi-Man Yip
Division of Neurosurgery, Department of Surgery, Kaohsiung Veterans General Hospital
Kaohsiung, 386, Dazhong 1st Road, Kaohsiung 81362, Taiwan, Republic of China
Tel: 07-3422124
Ext: 3017
E-mail: yip_chiman@yahoo.com
Received Date: May 22, 2017; Accepted Date: May 28, 2017; Published Date: May 30, 2017
Citation: Yip CM, Fu JH, Hsu SH, et al. Vertebral Artery Transection in Non-Penetrating Cervical Spine Injury: A Case Report. Med Case Rep, 2017, 3:2. DOI: 10.21767/2471-8041.100054
Abstract
Introduction: Vertebral artery injury associated with blunt cervical trauma has been infrequently reported. The prevalence of traumatic vertebral artery injury is approximately 0.5-2.0% to overall trauma patients, usually occurs in the setting of high-energy trauma. The most common mechanism of injury was high-speed motor vehicle collisions and pedestrian-versus-automobile collision. Here, we would like to report a case of cervical spine fracture with cord injury and left vertebral artery transection after a slipping down event that was successfully managed by endovascular intervention with favourable outcome.
Case report: A 42-year-old man having medical history of alcoholic liver disease and hepatitis C was sent to our ER in December 2016 in a conscious disturbance and hypotension state after suffering a slipping down event at a slope in a market after drinking. After resuscitation, a series of trauma imaging survey was arranged.
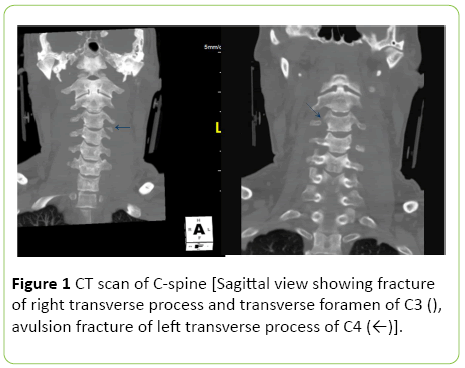
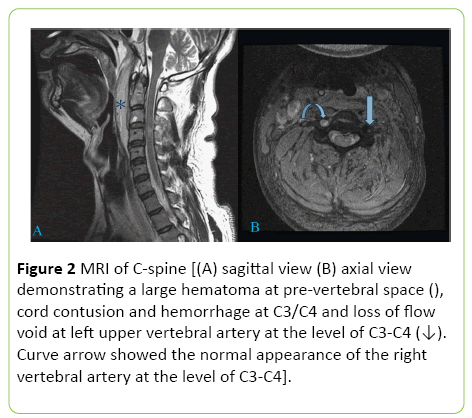
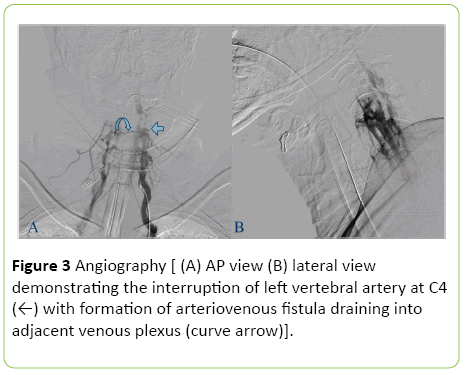
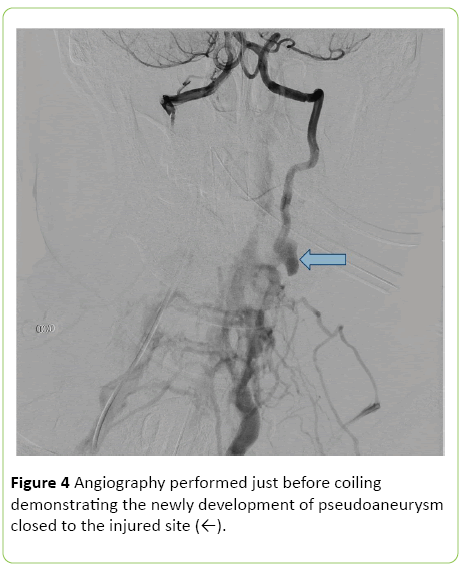
Results: His CT scan of brain showed essentially negative finding; his CT scan of C-spine demonstrated fracture of right transverse process and transverse foramen of C3, avulsion fracture of left transverse process of C4; his MRI of C-spine disclosed a large hematoma at pre-vertebral space, cord contusion and hemorrhage at C3/C4 without significant compressive lesion and loss of flow void at left upper vertebral artery at the level of C3-C4. Angiography was arranged to identify his vascular injury and it showed the interruption of left vertebral artery at C4 with formation of arteriovenous fistula draining into adjacent venous plexus. After evaluating his vital signs, liver function, and family discussion, endovascular intervention was preferred to manage his left vertebral artery injury. After the detachable coils were approved, successful trapping of the left vertebral artery was done by endovascular embolization. The angiography performed just before coiling showed the newly development of pseudoaneurysm closed to the injured site. 27 days after admission, he was discharged with stable vital signs, clear consciousness, but the muscle power of his right upper limb was grade 2/5 while the muscle power of his other extremities was grade 4/5 and he had no sphincter problem.
Conclusion: There is a particularly high risk for vertebral artery injury in the setting of cervical spine fractures with subluxation, and/or extension to the foramen transversarium. Under such circumstances, the vascular injury most likely occurs when tensile or shear strain exceeds the mechanical limits of arterial tissue during hyperflexion, hyperextension, anteroposterior translation, and/or forcible rotation. Displaced bone fragments can injure the artery directly especially when the foramen transversarium is disrupted. The clinician must be aware of the presence of vertebral artery injury in cases of cervical spine trauma.
Keywords
Cervical spine fracture; Endovascular intervention; Vertebral artery transection
Introduction
Blunt traumatic vertebral artery injury is relatively rare and its prevalence is approximately 0.5 to 2.0% to overall trauma patients [1,2]. 70% of all traumatic vertebral artery injury patients have an associated cervical spine fracture [3]. There are three types of cervical spine fractures associated with higher risk of vertebral artery injury: (1) fractures involving a transverse foramen; (2) subluxation; (3) fractures involving the upper cervical spine (C1-C3) [2-4]. Outcomes for patients suffering from vertebral artery injury can range from asymptomatic to posterior circulation stroke and even death [2,4].
Based on the angiographic appearance, blunt cerebrovascular injuries, including carotid artery injury and vertebral artery injury, have been graded as followings: grade I=irregularity of vessel wall or a dissection/intramural hematoma with less than 25% luminal stenosis; grade II=intraluminal thrombus or raised intimal flap is visualized, or dissection/intramural hematoma with 25% or more luminal narrowing; grade III=pseudoaneurysms; grade IV=vessels occlusions; grade V=vessel transaction or hemodynamically significant arteriovenous fistula [1-4].
Case Presentation
A 42-year-old man having medical history of alcoholic liver disease and hepatitis C was sent to our ER in December 2016 in a conscious disturbance and hypotension state after suffering a slipping down event at a slope in a market.
At ER, his initial recorded Glasgow Coma Scale (GCS) score was E3V2M5; his pupils size was 2.0/2.0 with light reflex and his initial recorded vital signs were as followings: BP=91/76 mmHg, HR=81/min, RR=18/min, O2 saturation=93%. His alcohol level was 319 mg/dL. Soon after arrival, his blood pressure dropped to 78/55 mmHg, and air hunger was noted.
After resuscitation, a series of trauma imaging survey was arranged. His computed tomography (CT) scan of brain showed essentially negative finding; his CT scan of C-spine demonstrated fracture of right transverse process and transverse foramen of C3, avulsion fracture of left transverse process of C4 (Figure 1); his magnetic resonance imaging (MRI) of C-spine disclosed a large hematoma at pre-vertebral space, cord contusion and hemorrhage at C3/C4 and loss of flow void at left upper vertebral artery at the level of C3-C4 (Figure 2).
Figure 2: MRI of C-spine [(A) sagittal view (B) axial view demonstrating a large hematoma at pre-vertebral space (), cord contusion and hemorrhage at C3/C4 and loss of flow void at left upper vertebral artery at the level of C3-C4 (↓). Curve arrow showed the normal appearance of the right vertebral artery at the level of C3-C4].
From imaging, there was no significant cord compression, so no emergent surgical intervention was arranged.
This patient was admitted to intensive care unit (ICU) for intensive care and monitoring. Angiography was arranged to identify his vascular injury and it showed the interruption of left vertebral artery at C4 with formation of arteriovenous fistula draining into adjacent venous plexus (Figure 3).
After evaluating his vital signs, liver function, and family discussion, endovascular intervention was preferred to manage his left vertebral artery injury. After the detachable coils were approved and his vital signs were stabilized, 18 days after admission, endovascular intervention to his left vertebral artery injury was done and he tolerated the procedure well. The angiography performed just before coiling showed the newly development of pseudoaneurysm closed to the injured site (Figure 4).
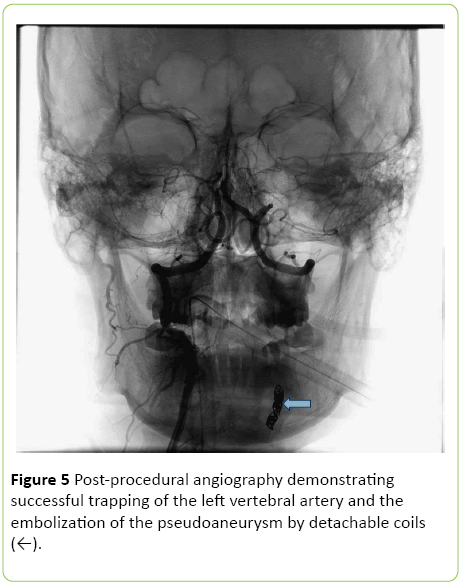
The post-procedural angiography demonstrated successful trapping of the left vertebral artery and the embolization of the pseudoaneurysm by detachable coils (Figure 5).
27 days after admission, he was discharged with stable vital signs, clear consciousness, but the muscle power of his right upper limb was grade 2/5 while the muscle power of his other extremities was grade 4/5 and he had no sphincter problem. Intensive rehabilitation program was arranged in a local hospital closed to his habitation after discharge.
Discussion and Conclusion
There is a particularly high risk for vertebral artery injury in the setting of cervical spine fractures with subluxation, and/or extension to the foramen transversarium [3,4]. The vascular injury most likely occurs when tensile or shear strain exceeds the mechanical limits of arterial tissue during hyperflexion, hyperextension, anteroposterior translation, and/or forcible rotation [4,5]. Displaced bone fragments can injure the artery directly especially when the foramen transversarium is disrupted [4]. Traumatic vertebral artery injury can present as occlusion, dissection, thrombosis, intimal injury, pseudoaneurysm, rupture, arteriovenous fistula and division [1,2,5]. The incidence of neurologic deficits secondary to vertebral artery injury ranges from 0% to 24% in published series [2]. Angiography has been the gold standard for the diagnosis of vertebral artery injury [2,4]. The treatment options to this particular vascular injury include close observation in asymptomatic patients, antiplatelet agents, heparin anticoagulation, thrombolytics, surgery and endovascular treatments [1,2,5]. The clinician must be aware of the presence of vertebral artery injury in cases of cervical spine trauma.
References
- Lee MA, Choi KK, Lee GJ, Yu BC, Ma DS, et al. (2016) A blunt traumatic vertebral artery injury: A case report. Journal of Trauma and Injury 29:28-32.
- Fassett DR, Dailey AT, Vaccaro AR (2008) Vertebral artery injuries associated with cervical spine injuries: A review of the literature. J Spinal Disord Tech 21:252-258.
- Cothren CC, Moore EE, Ray Jr CE, Johnson JL, Moore JB, et al. (2007) Cervical spine fracture patterns mandating screening to rule out blunt cerebrovascular injury. Surgery 141:76-82.
- Maloney E, Lehnert B, McNeeley MF (2015) Vertebral artery transection in non-penetrating trauma: A series of 4 patients. Ann VascSurg29:1450.
- Parbhoo AH, Govender S, Corr P (2001) Vertebral artery injury in cervical spine trauma. Injury Int JCare Injured 32:565-568.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences