Unilateral Pulmonary Artery Agenesis with Right Sided Aortic Arch
Hasan Erdogan, Fatma Zeynep Arslan and Meral Buyukterzi
DOI10.21767/2471-8041.100078
Hasan Erdogan*, Fatma Zeynep Arslan and Meral Buyukterzi
Department of Radiology, University of Health Sciences, Konya Education and Research Hospital, Turkey
- *Corresponding Author:
- Hasan Erdogan
Department of Radiology, University
of Health Sciences, Konya Education
and Research Hospital, 42090, Konya, Turkey
Tel: +90 506 473 0225
E-mail: dr.hasanerdogan@gmail.com
Received Date: July 09, 2017 Accepted Date: August 30, 2017 Published Date: September 2, 2017
Citation: Erdogan H, Arslan FZ, Buyukterzi M (2017) Unilateral Pulmonary Artery Agenesis with Right Sided Aortic Arch. Med Case Rep, Vol.3 No.4:43. doi: 10.21767/2471-8041.100074
Abstract
Unilateral pulmonary artery agenesis (UPAA) is a rare congenital anomaly due to a malformation of the sixth aortic arch during embryogenesis. It can occur as isolated or may be associated with other congenital cardiovascular malformations. Right-sided aortic arch (RAA) is infrequently seen entity that can be related to various forms of congenital heart disease. Among these, with mirror-image branching of the major arteries is the most encountered subtype. We have presented here a rare case of UPAA with RAA and Kommerell’s diverticulum.
Keywords
Unilateral Pulmonary Artery Agenesis (UAPA); Right-sided aortic arch; Kommerell’s diverticulum; Computer Tomography (CT)
Introduction
Unilateral absence of pulmonary artery (UAPA) is a rare congenital malformation that may develop in isolation or in association with congenital cardiovascular anomalies. UPAA can remain asymptomatic and diagnosis in adult age is possible, usually after an abnormal chest radiograph. A number of additional Computed tomographytechniques are available to aid the diagnosis. Physicians should consider the possibility of undiagnosed UPAA in adults [1].
Agenesis of the right pulmonary artery has a greater incidence than agenesis of the left. The affected pulmonary artery is most commonly opposite to the aortic arch. This explains why the more prevalent right UAPA occurs with a normal left-sided arch. UAPA is believed to result from the involution of the proximal sixth aortic arch, thereby forgoing expected embryological fusion with the pulmonary trunk. Most common symptoms experienced include recurrent pulmonary infections, hemoptysis, and shortness of breath upon exertion [2].
Case Report
A 24-year-old male patient was admitted to our hospital due to exertional dyspnea. The patient was a non-smoker with no history of exposure to noxious environmental or occupational factors. His physical examination revealed reduced pulmonary sounds on the left hemithorax.
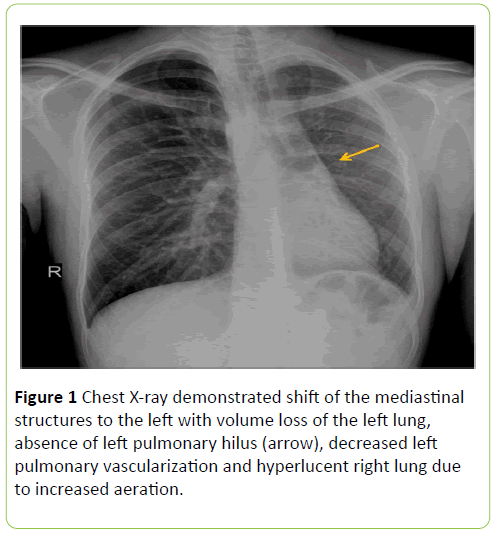
The rest physical examination and laboratory tests were normal. Chest X-ray demonstrated shift of the mediastinal structures to the left with volume loss of the left lung, decreased left pulmonary vascularization and hyperlucent right lung (Figure 1).
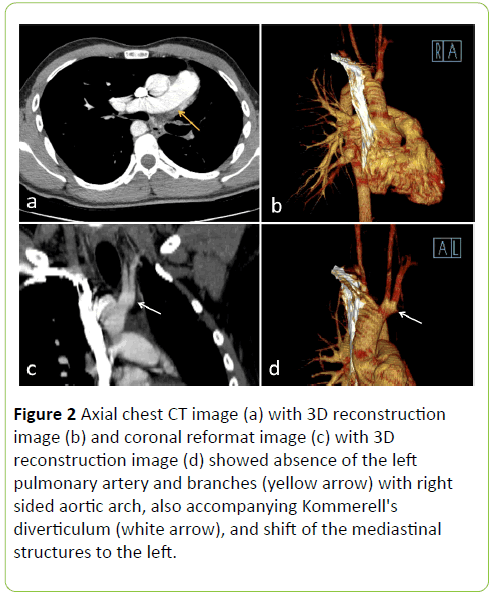
Pulmonary function tests showed a restrictive pattern. Chest CT with 3D reconstruction was performed showing absence of the left pulmonary artery with right sided aortic arch, Kommerell's diverticulum, a hypoplastic left lung and shift of the mediastinal structures to the left (Figure 2).
Figure 2: Axial chest CT image (a) with 3D reconstruction image (b) and coronal reformat image (c) with 3D reconstruction image (d) showed absence of the left pulmonary artery and branches (yellow arrow) with right sided aortic arch, also accompanying Kommerell's diverticulum (white arrow), and shift of the mediastinal structures to the left.
Discussion
UPAA is an infrequent condition which occurs in approximately 1 in 200,000 people [1-3]. UPAA is relatively uncommon on the left side. RAA is classified into three main groups based on anatomical structure. Type I, with mirrorimage branching of the major arteries; type II, with an aberrant subclavian artery, concomitant Kommerell diverticulum may be present; and type III, with isolation of the subclavian artery (where the subclavian artery is connected to the pulmonary artery through the ductus arteriosus [4]. Type I is the most common encountered subgroup [4,5]. While congenital heart diseases and vascular anomalies are associated with type 1, cardiovasculary disorders are rarely seen together with type 2. Our patient has another accompanying rare great vessel anomaly which is unusual for this subtype. UPAA and RAA are both postulated secondary to inaccruate embryological development of primitive aortic arches [6]. Patients with RAA only, those are generally asymptomatic and discovered only incidentally, however,complaints may vary depending on accompanying congenital cardiac anomalies. Symptoms can be seen related to compression of trachea and oesophagus due to malposition of aortic arch. Patients who had UPAA are generally presented with shortness of breath, recurrent pulmonary infections, chest pain, high-altitude pulmonary oedema [2,5]. The diagnosis can be made by plain radiograph, CT, MRI and angiography. CT scan shows unilateral absence of a pulmonary artery and also shows bronchiectasis by the reason of recurrent pulmonary infections in a patient with UPAA. MRI can be helpful in identifying concomitant cardiovascular abnormalities. But definitive diagnosis is pulmonary angiography. CT scan is also useful in demonstrating the RAA, mirror-image branching of the great arteries aberrant subclavian artery which arises as the last branch from the RAA then courses posteriorly to oesophagus anteriorly to the trachea in the thorax. CT scan can reveal Kommerell’s diverticulum that is a bulbous diverticulum from the proximal descending aorta at the level of origin of the aberrant left subclavian artery [6]. Treatment options for UPAA includes selective arterial embolisation and pneumonectomy in the setting of life-threatening haemoptysis or intractable pulmonary infections.
Conclusion
In conclusion, we have reported a unilateral pulmonary artery agenesis with right sided aortic arch. UPAA and RAA are rarely seen great vessel anomalies and radiologists should be familiar with these radiologic appearances. Clinicians and radiologists should consider the occurrence of undiagnosed cases in adults, with various atypical characteristics.
References
- Pool PE, Vogel JH, Blount SG Jr (1962) Congenital unilateral absence of a pulmonary artery. The importance of flow in pulmonary hypertension. Am J Cardiol 10: 706-732.
- Hastreiter AR, D'Cruz IA, Cantez T, Namin EP, Licata R (1966) Right-sided aorta. I. Occurrence of right aortic arch in various types of congenital heart disease. II. Right aortic arch, right descending aorta and associated anomalies. Br Heart J 28: 722-739.
- Cinà CS, Althani H, Pasenau J, Abouzahr L (2004) Kommerell's diverticulum and right-sided aortic arch: A cohort study and review of the literature. J Vasc Surg 39: 131-139.
- Stewart JR, Kincaid OW, Edwards JE (1964) An atlas of vascular rings and related malformation of the aortic arch system. Springfield, Ill: Charles C Thomas 3: 129
- Bouros D, Pare P, Panagou P, Tsintiris K, Siafakas N (1995) The varied manifestation of pulmonary artery agenesis in adulthood. Chest 108: 670-676.
- Weinberg PM (2006) Aortic arch anomalies. J Cardio Magnetic Res 8: 633-643.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences