Treatment of Gastric Lymphoma Bleeding Due to Erosion of the Splenic Artery with Transcatheter Arterial Embolization via the Superior Mesenteric Artery Approach
Tai-Lun Chang*
Department of Medical Imaging, Kaohsiung Medical University Hospital, KMU, Kaohsiung, Taiwan
- Corresponding Author:
- Tai-Lun Chang,
Department of Medical Imaging,
Kaohsiung Medical University Hospital, KMU, Kaohsiung, Taiwan
E-mail: poseidonhephaes@hotmail.com
Received date: January 23, 2023, Manuscript No. IPMCRS-23-15662; Editor assigned date: January 25, 2023, PreQC No. IPMCRS-23-15662 (PQ); Reviewed date: January 31, 2023, QC No. IPMCRS-23-15662; Revised date: February 06, 2023; Manuscript No. IPMCRS-23-15662 (R); Published date: February 10, 2023, DOI: 10.36648/2471-8041.9.1.260
Citation: Chang TL (2023) Treatment of Gastric Lymphoma Bleeding Due to Erosion of the Splenic Artery with Transcatheter Arterial Embolization via the Superior Mesenteric Artery Approach. Med Case Rep Vol.9 No.1:260.
Abstract
Lymphoma is one of the most common neoplasms of the stomach but a rare cause of upper gastrointestinal bleeding. We present a case of sudden onset bloody vomitus and tarry stool in an 87-year-old female. Computed tomography angiography suggested a gastric lymphoma with splenic artery erosion that probably led to pseudoaneurysm formation and massive bleeding. Transcatheter arterial embolization was performed because endoscopic hemostasis failed and her hemodynamic status was unstable. Ostial stenosis of the celiac trunk was observed, so we chose the superior mesenteric artery as an alternative approach. We used a microcatheter via the gastroduodenal artery and a retrograde approach to the celiac trunk to engage the distal splenic artery. Hemostasis was achieved by infusion of gelatin sponge particles through a microcatheter. Endoscopic biopsy of the gastric lymphoma indicated a mucosa-associated lymphoid tissue lymphoma.
Keywords
Case report; Lymphoma; Transcatheter arterial
Introduction
The most frequent cause of non-variceal upper Gastrointestinal (GI) bleeding is a peptic ulcer and other causes include benign and malignant tumors, gastritis, vascular malformations and trauma and Mallory–Weiss tears [1]. The GI tract is the most common extranodal site involving lymphomas and accounts for 5%–20% of all lymphomas [2]. Non-variceal GI bleeding from a GI lymphoma is a life-threatening condition. The initial treatment is a combination of medical therapy and endoscopic management [3]. However, failure of hemostasis occurs in ≤ 20% of cases [4]. Surgical intervention and Transcatheter Arterial Embolization (TAE) can be an alternative treatment in patients with refractory hemostasis or unstable hemodynamics. TAE is a reasonable and less hazardous alternative to surgery and has become the preferred therapeutic approach for the treatment of refractory non-variceal GI bleeding [5]. We present a case of sudden onset bloody vomitus and tarry stool in an 87-year-old female that was caused by a gastric Mucosa-Associated Lymphoid Tissue (MALT) lymphoma with splenic artery erosion that had caused pseudoaneurysm formation and massive bleeding.
Case Report
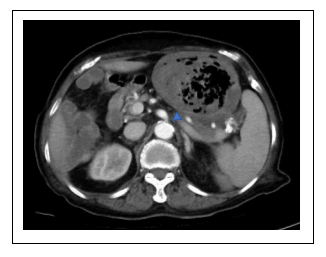
The 87-year-old female had a history of essential thrombocythemia and was undergoing phosphodiesterase inhibitor treatment. She was sent to the emergency room because of sudden onset of massive bloody vomitus and tarry stool. In recent months, she also had a poor appetite and experienced body weight loss. She denied a family or personal history of GI cancer or previous abdominal surgery. Physical examination revealed upper abdominal tenderness with mild abdominal distention. Hypovolemic shock status and normocytic anemia were noted. Urgent abdominal Computed Tomographic Angiography (CTA) was performed and showed circumferential wall thickening of the stomach (Figure 1a), which suggested a pseudoaneurysm at the gastric fundus and gastrosplenic fistula formation (Figure 1b).
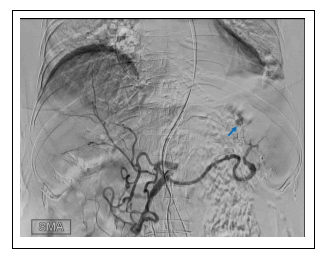
Emergent endoscopic hemostasis was tried but failed because of a poor visual field caused by massive bleeding. The patient was transferred to our department for TAE. We used the Seldinger technique to create a working channel with a 5-Fr sheath at the right common femoral artery. A 5-Fr Yashiro catheter (Terumo) with a 0.038-inch Terumo guidewire was chosen for the guiding system initially. However, difficult engagement of the celiac trunk due to ostial stenosis of the celiac trunk occurred (Figure 2) even though we changed to a 4-Fr RC-1 catheter (COOK) subsequently.
A superior mesenteric angiogram showed contrast medium reflux to the celiac trunk via the collateral pathway of the Gastroduodenal Artery (GDA). A pseudoaneurysm at the distal splenic artery with contrast medium extravasation could be clearly seen by digital subtraction angiography (Figure 3).
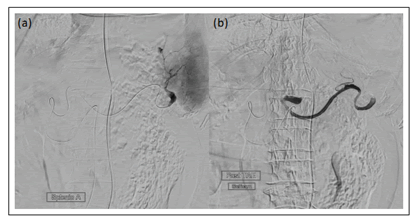
For selective TAE, we used an Asahi microcatheter (180 cm) to further proceed along the distal splenic artery via a retrograde path from the GDA (Figure 4a). We attempted to perform coil embolization, but the microcatheter suddenly jumped off because of a poor supportive system. Instead, hemostasis was achieved by infusion of gelatin sponge particles via a microcatheter. Hypovolemic shock resolved after successful hemostasis (Figure 4b). The patient was discharged in the following weeks without surgical intervention or repeat TAE. Endoscopic biopsy of the gastric lymphoma indicated a MALT lymphoma.
Results and Discussion
In general, endoscopic intervention, including epinephrine injection, sclerotherapy and metal clip placement, is the primary technique used for the diagnosis and treatment of GI bleeding [6]. One study conducted in 4478 patients with non-variceal upper GI bleeding showed that TAE was more effective and safer than surgery for the management of bleeding after failure of endoscopic therapy [7]. In our case, emergent endoscopy was performed without advanced hemostasis procedures because of a poor visual field caused by massive bleeding. Surgical intervention was not favored because of the patient’s old age and comorbidities. In general, the left gastric, right gastric, gastroepiploic and gastro duodenal arteries contribute to upper GI bleeding. CTA has been used to accurately (sensitivity ≤ 86%) diagnose acute GI bleeding and can show the precise location and etiology of bleeding [8]. Decreased procedure durations and less radiation exposure and contrast medium consumption can be expected with the help of pre-procedural CTA, although vascular anatomical variations can make the procedure more difficult. We chose to use gelatin sponge particles as embolic materials, but other options, such as a coil or N-butyl cyanoacrylate, could be considered. However, there are few reports in the literature about the efficacy of embolic materials in these gastric lymphoma patients. Many studies have reported rebleeding rates ranging from 9% to 66% [9]. Repeated TAE or surgical intervention may be considered if bleeding persists.
Conclusion
Upper GI bleeding is a common medical problem associated with substantial morbidity or even mortality. For treatment, TAE is an alternative to endoscopic hemostasis and surgical intervention. Anatomical vascular variations add to the difficulties of the procedure. It is important to choose suitable equipment and embolization agents to achieve successful hemostasis.
Acknowledgment
I would like to thank the operation assistance staff of the digital subtraction room, Kaohsiung Medical University Hospital.
Ethical Statement
This case has been performed in accordance with the ethical standards laid down in the 1964 declaration of Helsinki and its subsequent amendments.
Conflicts of Interest
The author declares that they have no conflict of interest.
Author’s Contributions
Tai-Lun Chang contributed to the study conception and design. Material preparation, data collection and analysis were performed by Tai-Lun Chang. The first draft of the manuscript was written by Tai-Lun Chang and commented on previous versions of the manuscript. The author read and approved the final manuscript.
Data Availability
No data were used to support this study.
Consent
No written consent has been obtained from the patients as there is no patient identifiable data included in this case report/series.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Huang C, Lichtenstein DR (2003) Non-variceal upper gastrointestinal bleeding. Gastroenterol Clin North Am 32: 1053–78.
[Crossref], [Google Scholar], [Indexed]
- Pyo JH, Lee BJ, Lee HJ, Kim JW, Kim KJ, et al. (2013) A case of ileal mucosa-associated lymphoid tissue lymphoma accompanied by luminal stricture and arterial spurting. Korean J Gastroenterol 62: 365–9.
[Crossref], [Google Scholar], [Indexed]
- Lee HH, Park JM, Chun HJ, Oh JS, Ahn HJ, et al. (2015) Transcatheter arterial embolization for endoscopically unmanageable non-variceal upper gastrointestinal bleeding. Scand J Gastroenterol 50: 809–815.
[Crossref], [Google Scholar], [Indexed]
- Targownik LE, Nabalamba A (2006) Trends in management and outcomes of acute non-variceal upper gastrointestinal bleeding: 1993–2003. Clin Gastroenterol Hepatol 4: 1459–66.
[Crossref], [Google Scholar], [Indexed]
- Loffroy R, Guiu B, Cercueil JP, Lepage C, Latournerie M, et al. (2008) Refractory bleeding from gastroduodenal ulcers: Arterial embolization in high-operative-risk patients. J Clin Gastroenterol 42: 361–7.
[Crossref], [Google Scholar], [Indexed]
- Ramaswamy RS, Choi HW, Mouser HC, Narsinh KH, McCammack KC, et al. (2014) Role of interventional radiology in the management of acute gastrointestinal bleeding. World J Radiol 6: 82–92.
[Crossref], [Google Scholar], [Indexed]
- Jairath V, Kahan BC, Logan RF, Hearnshaw SA, Dore CJ, et al. (2012) National audit of the use of surgery and radiological embolization after failed endoscopic haemostasis for non-variceal upper gastrointestinal bleeding. Br J Surg 99: 1672–80.
[Crossref], [Google Scholar], [Indexed]
- Miller JM, Smith TP (2005) Angiographic diagnosis and endovascular management of non-variceal gastrointestinal hemorrhage. Gastroenterol Clin North Am 34: 735–52.
[Crossref], [Google Scholar], [Indexed]
- Loffroy R, Rao P, Ota S, Lin MD, Kwak BK, et al. (2010) Embolization of acute non-variceal upper gastrointestinal hemorrhage resistant to endoscopic treatment: Results and predictors of recurrent bleeding. Cardiovasc Intervent Radiol 33: 1088–100.
[Crossref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences