Subarachnoid Hemorrhage Following Anticoagulation Therapy in a Patient with Infective Endocarditis Complicated by Ischemic Stroke
Seyma Eroglu and Ilhan Birsenogul
Published Date: 2022-04-29DOI10.36648/2471-8041.8.4.219
Seyma Eroglu1* and Ilhan Birsenogul2
1Department of Internal Medicine, Weiss Memorial Hospital, Chicago, Illinois
2Department of Internal Medicine, SBU Adana Sehir Egitim ve Arastirma Hastanesi, Adana, Turkey
- *Corresponding Author:
- Seyma Eroglu
Department of Internal Medicine; Weiss Memorial Hospital, Chicago, Illinois
E-mail:seroglu@weisshospital.com
Received date: April 1, 2022, Manuscript No. IPMCRS-22-13271; Editor Assigned date: April 4, 2022, PreQC No. IPMCRS-22-13271(PQ); Reviewed date: April 19, 2022, QC No. IPMCRS-22-13271; Revised date: April 25, 2022, Manuscript No. IPMCRS-22-13271(R); Published date: April 29, 2022, DOI: 10.36648/2471-8041.8.4.219
Citation: Eroglu S (2022). Subarachnoid Hemorrhage Following Anticoagulation Therapy in a Patient with Infective Endocarditis Complicated by Ischemic Stroke. Med Case Rep Vol.8 No.4:219.
Abstract
Infective Endocarditis (IE) can cause ischemic stroke from the embolization of endocardial vegetations, and neurological complications in IE are associated with high morbidity and mortality rates. Most cases of IE can be treated with antibiotics, and cardiac surgery is indicated in some cases. Despite cardiac surgery not being contraindicated for patients with IE complicated by ischemic stroke, it poses risks of hemorrhagic transformation due to required high-dose anticoagulation. We present a patient with Staphylococcus aureus infective endocarditis complicated by ischemic stroke who developed subarachnoid hemorrhage and died within two days after initiation of anticoagulation therapy.
Keywords
Endocarditis; Stroke; Emboli; Abscess; Hemorrhage
Introduction
Infective endocarditis is a heterogeneous disease due to highly variable etiology, clinical presentation, and complications. This case serves to broaden our knowledge of the clinical heterogeneity of S. aureus IE with a presentation of cerebral and cerebellar septic emboli, cervical spine epidural abscess, sternocleidomastoid muscle abscess, and renal emboli. Most cases of IE can be treated with antibiotics. However, surgical intervention is indicated in patients with congestive heart failure, prosthetic valve endocarditis, persistent sepsis, systemic embolism, and cerebrovascular complications [1]. Cardiac surgery is not contraindicated by an ischemic stroke in patients with IE if there is no evidence of cerebral hemorrhage and severe neurological complications [2]. However, anticoagulation, which is required for cardiac surgery with cardiopulmonary bypass, may increase the risk of hemorrhagic conversion of ischemic stroke in patients with S. aureus IE [3]. This case illustrates the fatal complications of the anticoagulation therapy in a patient with S. aureus IE complicated by an ischemic stroke.
Case Study
A 58-year-old previously healthy man presented to the emergency department with left upper extremity weakness and shortness of breath. His symptoms started a week ago but worsened in the last twenty-four hours prior to the presentation. He has a history of non-injecting drug use. On presentation, vital signs revealed a temperature of 38.3°C, heart rate of 113 beats/min, respiratory rate of 30 breaths/min, blood pressure of 107/67 mm Hg, and oxygen saturation of 90% on room air. His physical exam was remarkable for severe dysarthria, left arm flaccid paralysis, left leg weakness, and left sternoclavicular joint mass.
Blood tests revealed WBCs 37.9 K/mcL, Hb 12.3 g/dL, platelets 11 K/mcL, Na 142 mmol/L, K 2.8 mmol/L, BUN 42 mg/dL, creatinine 0.92 mg/dL, calcium 7.5 mg/dL, albumin 1.9 g/dL, ALP 185 IU/L, AST 143 IU/L, ALT 67 IU/L, and lactic acid of 4.0 mmol/L. Coagulation tests showed PT 12.7 seconds, INR 1.3, and PTT 32.6 seconds. Urinalysis showed WBC 40-50, bacteria 4+, trace leukocyte esterase, and positive nitrite. A urine toxicology screen was positive for cocaine and opiate. His blood ethanol level was less than 10 mg/dL.
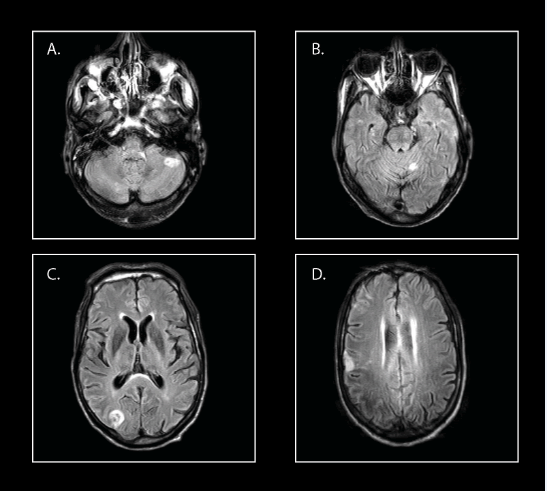
CT head without contrast was negative for intracranial hemorrhage. CT angiography head and neck demonstrated evolving areas of recent ischemia in the right parietal-occipital lobes posteriorly, the right precentral gyrus, the right frontal-parietal junction, and the left posterior superior frontal lobe, potentially embolic in etiology. MRI brain showed scattered subacute infarcts in all cerebral and cerebellar territories (Figure 1).
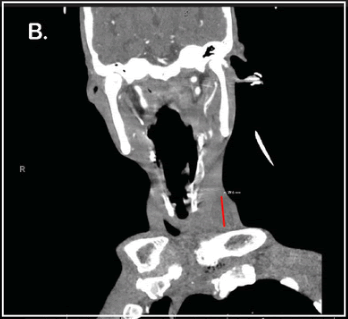
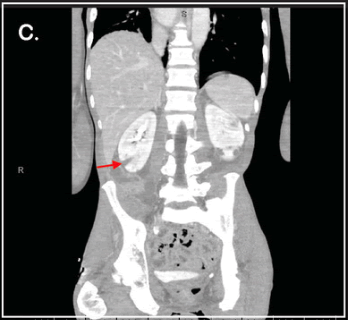
Broad-spectrum intravenous antibiotics including vancomycin, cefepime, and metronidazole were started. He was admitted to the medical intensive care unit due to acute respiratory failure requiring a high flow nasal cannula secondary to sepsis. Further imaging studies revealed cervical spine C6-C7 epidural abscess (Figure 2A), sternocleidomastoid muscle abscess measuring up to 3.0 cm (Figure 2B), and wedge-shaped hypodensities of the bilateral kidneys (Figure 2C). Transthoracic echocardiogram showed 1.8 cm × 1.3 cm ovoid echodensity associated with the posterior mitral leaflets and annulus, and large vegetation on the mitral valve consistent with endocarditis with possible abscess. Blood cultures and urine cultures were positive for Methicillin-Resistant Staphylococcus Aureus (MRSA).
The diagnosis of infective endocarditis was made according to the Duke criteria. He has undergone left sternoclavicular joint debridement, sternocleidomastoid muscle abscess incision and drainage, and C6-C7 anterior cervical discectomy and fusion. However, daily blood cultures persistently grew MRSA despite multiple surgeries and treatment with IV antibiotics. He later developed septic shock. Mitral valve replacement is indicated due to persistent sepsis despite adequate antibiotic therapy, systemic embolization, and large vegetation on the mitral valve.
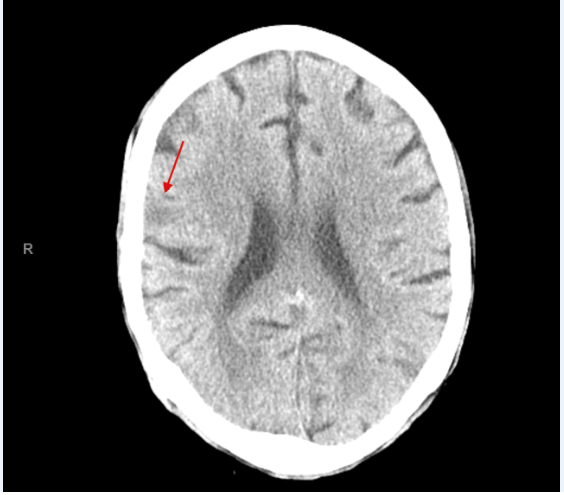
He needed to be therapeutically anticoagulated for mitral valve replacement surgery. He was transfused with platelets and anticoagulated with IV heparin prior to surgery. However, preoperative CT head without contrast demonstrated subarachnoid hemorrhage within the right parietal sulci (Figure 3). Anticoagulation was discontinued immediately, and cardiac surgery had to be postponed. Due to his poor prognosis and worsening clinical condition, comfort care was elected, and the patient died on the fifteenth day of admission.
Results and Discussion
In this case, the patient had a history of non-injection drug use as a risk factor for IE and was presented with sepsis and neurological symptoms. Further laboratory and diagnostic studies revealed MRSA bacteremia and mitral valve endocarditis with multi-organ septic emboli. He received appropriate antibiotic therapy and has undergone multiple surgeries for infectious source control. However, he had persistent sepsis, and cardiac surgery with mitral valve replacement is indicated.
Ischemic stroke is the most common neurological complication of infective endocarditis and is associated with a poor prognosis [4]. Questions have been raised about the safety of anticoagulation therapy in patients with ischemic stroke when cardiac surgery for IE is indicated due to concerns for hemorrhagic conversion of ischemic stroke. Literature review shows improved survival with early surgical treatment in patients with IE with cerebral septic embolisms [5,6]. According to the 2020 ACC/AHA heart valve disease guideline, in patients with IE with an indication for surgery who suffered a stroke without intracranial hemorrhage, surgery without delay may still be considered.
It is recommended to use short-acting anticoagulants such as intravenous heparin when surgery for IE is indicated [1]. Preoperative neurological imaging with CT or MRI is highly recommended for patients with IE and preexisting ischemic stroke due to an increased risk of hemorrhagic transformation. It is advised to delay cardiac surgery ≥ 4 weeks if there is evidence of intracranial hemorrhage [2]. Neurological complications in IE are associated with high morbidity and mortality rates [4]. Given its complexity, patients with IE and cerebrovascular complications should be managed by the IE team including infectious disease, cardiology, cardiac surgery, neurology, neurosurgery, radiology and other specialists when needed [7].
Conclusion
The management of ischemic stroke in the setting of IE is challenging, especially when cardiac surgery is indicated. Intracranial hemorrhage should be ruled out with neurological imaging prior to initiation of anticoagulation therapy, and follow-up preoperative imaging is recommended to monitor for the hemorrhagic transformation of ischemic stroke. Hemorrhagic stroke is associated with high mortality in patients with S. aureus IE as shown in this patient who died within two days after initiation of anticoagulation therapy.
Detailed Author’s Contribution
The authors fulfill the ICMJE criteria for authorship and contributed equally.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
- Prendergast BD, Tornos P (2010) Surgery for infective endocarditis: Who and when? Circulation 121: 1141-52.
[Crossref], [Google Scholar], [Indexed]
- Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP III, et al. (2021) 2020 ACC/AHA guideline for the management of patients with valvular heart disease: Executive summary: A report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. 143: e35-e71.
[Crossref], [Google Scholar], [Indexed]
- Tornos P, Almirante B, Mirabet S, Permanyer G, Pahissa A, et al. (1999) Infective endocarditis due to Staphylococcus aureus: Deleterious effect of anticoagulant therapy. Arch Intern Med 159: 473-5.
[Crossref], [Google Scholar], [Indexed]
- Novy E, Sonneville R, Mazighi M, Klein IF, Mariotte E, et al. (2013) Neurological complications of infective endocarditis: New breakthroughs in diagnosis and management. Med Mal Infect 43: 443-50.
[Crossref], [Google Scholar], [Indexed]
- Piper C, Wiemer M, Schulte HD, Horstkotte D (2001) Stroke is not a contraindication for urgent valve replacement in acute infective endocarditis. J Heart Valve Dis 10: 703-11.
[Crossref], [Google Scholar], [Indexed]
- Wan S, Sung K, Park PW, Kim WS, Lee YT, et al. (2014) Stroke is not a treatment dilemma for early valve surgery in active infective endocarditis. J Heart Valve Dis 23: 609-16.
[Crossref], [Google Scholar], [Indexed]
- Yanagawa B, Pettersson GB, Habib G, Ruel M, Saposnik G, et al. (2016) Surgical management of infective endocarditis complicated by embolic stroke: Practical recommendations for clinicians. Circulation 134: 1280-1292.
[Crossref], [Google Scholar]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences