Spontaneous Pseudomeningocele of a Sphenoid Sinus: An Case Report
Zuzana Horakova and Hana Binkova
| Zuzana Horakova1, Hana Binková1* and Marta Pa?ourková2 |
| Corresponding Author: Hana Binkova,Department of Otorhinolaryngology and Head and Neck Surgery, St. Anne´s University Hospital and Faculty of Medicine, Masaryk University Brno, Czech Republic.Tel: +420543182951 E-mail: hana.binkova@fnusa.cz |
| Received: November 13, 2015 Accepted: December 22, 2015 Published: December 28, 2015 |
| Related article at Pubmed, Scholar Google |
Abstract
Introduction: A spontaneous pseudomeningocele (PMC) (e.g.without previous surgery or injury) is a rare pathology that may be mimicked as an unilateral polypoid mass in endoscopy or as a mucocele on CT /MRI, which only very exceptionaly doesn’t present with rhinoliquorhea. PMC develops when cerebrospinal fluid (CSF) becomes trapped behind the paranasal sinus mucosa or extracranial soft tissues, and may be associated with bony erosion.
Case presentation: We present an exceptional case of a 47-year-old man with a rare spontaneus pseudomeningocele of the sphenoid sinus without any obvious clinical symptoms, which resembles a mucocele on CT and MRI scans and which was first correctly diagnosed after an exploratory sphenoidotomy. Due to postsurgical complications (a significant rhinoliquorhea), an endoscopic obliteration of the sphenoid cavity was necessary.
Conclusion: In the report we intend to stress the pitfalls of an exceptional skull base pathology and its surgical complications in patients with atypical manifestations. For successful treatment, a wide exposure to address all potential skull base defects and following duroplasty is recommended.The biggest challenge of spontaneous PMC is a correct diagnosis, especially when typical symptoms are absent. In the case report we want to point out the pitfalls of an endonasal surgery, which may result in another surgical revision after futher investigation.
Keywords |
||||||
| Pseudomeningocele; Sphenoidal sinus; Liquorrhea; Skull base | ||||||
Abreviation list |
||||||
| PMC-Pseudomeningocele; CSF-Cerebrospinal fluid; SS-Sphenoid Sinus | ||||||
Introduction |
||||||
| Small bony defects in the skull base may stay clinically silent while larger ones may lead to spontaneous herniation and meningocele or meningoencephalocele development. These typically present with cerebrospinal fluid (CSF) rhinorrhea and a pulsatile or compressible nasal mass. Pseudomeningocele (PMC) is a collection leaking CSF retained underneath the mucosa in the soft tissue of the skull base without meningeal capsula. Most commonly localized in the thoracic or lumbar spine, occurrence in the head and neck is exceptional and almost exclusively related to a history of trauma or neurosurgical intervention. | ||||||
Case Report |
||||||
| A 47-year-old man was referred from neurology where he was examined for a sudden episode of unconsciousness with convulsions; epilepsy was suspected. | ||||||
| He had experienced a previous episode of convulsive paroxysmus 20 years before, which was thought to be epilepsy, without any pathology on CT at that time. As it did not recur, it was not treated. | ||||||
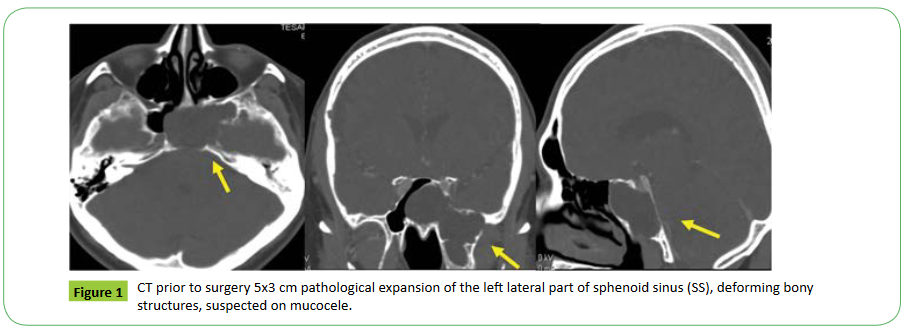
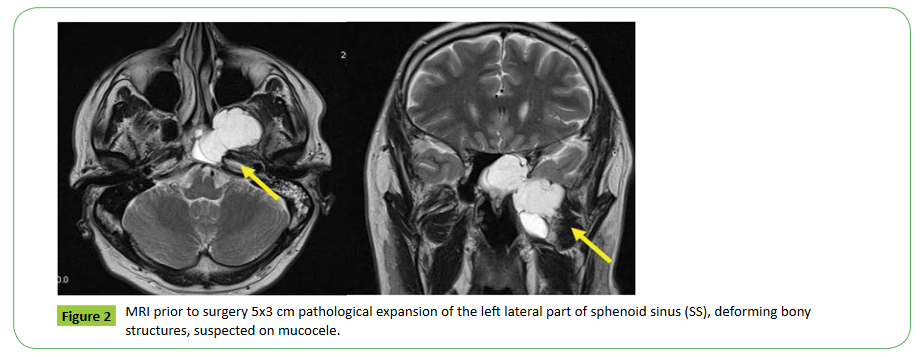
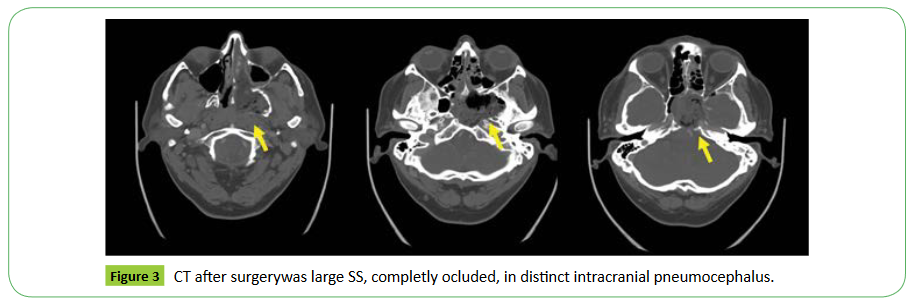
| The CT showed a 5x3cm pathological expansion of the left lateral part of sphenoid sinus (SS), deforming bony structures, which was suspected on mucocele (Figures 1 and 2). The patient had no history of craniotrauma or skull base surgery, was completely free from rhinogenic symptoms and showed no pathology during nasal endoscopy. Endoscopic exploratory sphenoidotomy was suggested (transnasal paraseptal access), which revealed serous fluid retention in the SS, an osteolytic defect of the skull base, with exposure of dura and dehiscent bony covering of a carotid artery and an extensive lateral recess of the SS. There was no sign of tumor or CSF leak after a detailed exploration, and the operation was finished with a gauze pack. But on the second day after surgery, a few hours after the nasal pack was removed, a massive serous nasal discharge occurred (CSF was verified biochemically), which demanded an acute surgical exploration. The entire SS was endoscopically examined without locating any evident location of the CSF leak, but was filling in Trendelenburg position with cerebrospinal fluid, but the origin of CSF leak was not identified. As no duroplasty could thus be performed, only complete sinus pack with use of multilayer technic (fibrin glue, fascia, muscle) was executed. The post-surgical CT showed a large SS, completely occluded, and an indistinct intracranial pneumocephalus (Figure 3). On the second postoperative day the patient developed a headache, inflammatory markers increased in the blood (Leu13, CRP 200) and CSF (admixture of activated forms of lymphocytes and monocytes). He was treated with metronidazole and carbapenem for three weeks; bed rest in the reverseTrendelenburg position resulted in a rapid response, and favourable healing without liquor hea. Now, the patient is completly symptom free (both neurological and rhinoliquorhea) 3 years post-surgery. | ||||||
Discussion |
||||||
| A lateral type of SS means the presence of a lateral recess extending to pterygoid process, large wing or both, which is an uncommon variety of SS as in our case [1]. However, unlike most spontaneous CSF leaks via pre-existing dehiscence or preformed pathways where CSF extravasates directly into the SS, in spontaneous pseudomeningocele of the skull base, the CSF accumulates behind the mucosa of the paranasal sinus and may extend into the soft tissue of the infratemporal or pterygopalatine fossa. Fluid accumulation by a valve mechanism might result in bone resorption and subsequent enlargement of the bone defects [2]. | ||||||
| In the few cases of spontaneous PMC of SS published so far (6 to our knowledge), most of them presented with CSF nasal liquorrhea; endoscopically this may mimick a nasal polyp, compressible mass. On CT and MRI scans, they usually resemble a mucocoele. In the absence of rhinoliquorrhea, the correct diagnosis is even more challenging [3-5]. And as in our case, it might become a possible trap/pitfall for the surgeon. In our patient, the pathology was asymptomatic, with possible presentation of neurological symptoms, and an episode of paroxysmus. But most probably due to history of another paroxysmal episode, although 20 years ago, it might be also regarded as accidental coincidence in which causality was not confirmed. Relation to PMC was not probable, although it could not be excluded. No similar case has been published so far, nor has any theory been suggested. | ||||||
| Diagnostics prior to surgery CT (HRCT resp.) is regarded as necessary for estimating skull base variability and landmarks for the surgeon. MRI can complement CT (focusing on soft tissue and excluding meningocele). CSF leak diagnostics enable cisternografy (CT or MRI) with contrast dye injected into subarachnoid space, or scintigraphy (application of fluorescein during surgery), as well as the Valsalva manoeuvre executed by an anesthesiologist. Rhinoliquorhea, is a laboratory confirmed test on Beta 2-transferrin. | ||||||
| A surgical endoscopic approach to sphenoid sinus preferred. After a sufficient exposure of the whole area, endoscopic surgery: transethmoidal or more preffered transpterygoidal way and subsequently duroplasty is performed, followed by coverage with a vascularized mucosal pedicled flap (nasoseptal flap) or free tissue grafts, (fat, fascia, muscle). The success rate is over 90% in expert hands. Among the major complications (1%) we might expect meningitis, subdural hematoma, intracranial abscess, chronic headaches, pneumocefalus, intracranial hematoma or abscess, or fistula recurrence [6]. | ||||||
| If the leak is not accessible for duroplasty, or identified, in patients with pituitary fossa, posterior or lateral SS segment leak location, obliteration of SS with facia or fat is recommended. After previous complete mucosa removal an external transcranial access remains for recurring leaks in an extensive pathology. | ||||||
Conclusion |
||||||
| A spontaneous PMC (e.g.without previous surgery or injury) is a rare pathology that may be mimicked as an unilateral polypoid mass in endoscopy or as a mucocele on CT /MRI, which only very exceptionaly doesn’t present with rhinoliquorrhea. | ||||||
| PMC develops when CSF becomes trapped behind the paranasal sinus mucosa or extracranial soft tissues, and may be associated with bony erosion. | ||||||
| For successful treatment, a wide exposure to address all potential skull base defects and following duroplasty is recommended. If this is not possible, sinus occlusion after complete mucosa removal might be executed. | ||||||
| The biggest challenge of spontaneous PMC is a correct diagnosis, especially when typical symptoms are absent. | ||||||
| In the case report we want to point out the pitfalls of an endonasal surgery, which may result in another surgical revison after futher investigation. | ||||||
Consent |
||||||
| Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in- Chief of this journal. | ||||||
Competing Interests |
||||||
| The authors declare that they have no competing interests. | ||||||
Authors' Contributions |
||||||
| ZH performed the presurgical diagnostic procedures, data acquisition and interpretation, including CT scansand was a major contributor in writing the manuscript. | ||||||
| HB analyzed and interpreted the patients clinical and radiological data, monitored the patient during postsurgical follow up. | ||||||
| All authors read and approved the final manuscript. | ||||||
Funding |
||||||
| Supported by grant GA16-12454S. | ||||||
Figures at a glance |
||||||
|
||||||
References |
||||||
|

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences