Spontaneous Pneumomediastinum as a Complication of Covid-19 Infection
Rhiannon Worrall*, M. Marathe and S. Chand
DOI10.36648/2471-8041.21.7.196
Rhiannon Worrall*, M. Marathe and S. Chand
Renal Department, Royal Shrewsbury Hospital, UK
- *Corresponding Author:
Received: August 03, 2021; Accepted: August 17, 2021; Published: August 24, 2021
Citation: Worrall R, Marathe M, Chand S (2021) Spontaneous Pneumomediastinum as a Complication of Covid-19 Infection. Med Case Rep Vol.7 No.8.196
Abstract
A 46 year old male patient presented with worsening shortness of breath, productive cough, and mild central chest pain two weeks post positive polymerase chain reaction (PCR) test results for COVID-19 infection. Computed Tomography imaging revealed evidence of COVID-19 pneumonitis complicated by spontaneous pneumomediastinum (SPM). This patient was commenced on standard treatment for COVID-19 pneumonitis, whilst the SPM was managed conservatively. Unfortunately, the treatment plan was complicated further by steroid induced psychosis and hence dexamethasone was stopped prematurely. Despite this setback the patient made good recovery and was discharged home after 6 days.
Keywords
COVID Pneumonitis; COVID-19; Spontaneous Pneumomediastinum
Introduction
The Coronavirus 2019 (COVID-19) is multi system disease caused by the severe acute respiratory syndrome coronavirus-2 ( COVID-19). Whilst the typical presentation of the disease is now well documented [1], evidence surrounding complications of the disease is still emerging. Spontaneous pneumomediastinum (SPM) is defined as free air within the mediastinum that is not associated with trauma [2]. Predisposing factors for SPM include drug abuse, asthma, and other lung diseases such as chronic obstructive pulmonary disease and interstitial lung disease [3,4]. New evidence has begun to highlight SPM as a rare complication and presentation of patients with COVID-19 infection. This is particularly interesting as historically viral infections have rarely caused SPM, with only a few cases documented with CMV, measles pneumonia and influenza infections [5]. A recent review of the literature identified only 15 cases of SPM in patients with COVID-19 infection worldwide [6]. However, a significant proportion of these cases were associated with the use of mechanical ventilation and/or predisposing risk factors [7-9]. We therefore present a rare case of COVID-19 infection complicated by SPM in a patient with no predisposing factors and who had not received any form of mechanical ventilation. Unfortunately, this patient also suffered a brief episode of psychosis as a complication of high dose steroid treatment.
Case Presentation
A 46 year old male patient with a background history of migraines, sciatica, cervical spondylosis, and tinnitus presented to the Princess Royal Hospital Telford emergency department, with 2 day history of shortness of breath, productive cough and mild central chest pain which was non-radiating. The patient had previously tested positive for COVID-19 two weeks earlier and had been self-isolating at home. The patient had no pre-existing lung pathology and denied ever smoking or taking recreational drugs. This patient was a white male, height 5 ft 7 inch with a healthy BMI and no personal or family history of pneumomediastinum. Initial examination revealed that the patient was severely hypoxic, with oxygen saturations of 79% on air and tachypnoeic with a respiratory rate of 24. The patient was haemodynamically stable and apyrexial. Chest examination revealed bi-basal crackles, the rest of the physical examination was benign. There were no detectable findings specific to pneumomediastinum such as Hamman sign or subcutaneous emphysema.
Investigations
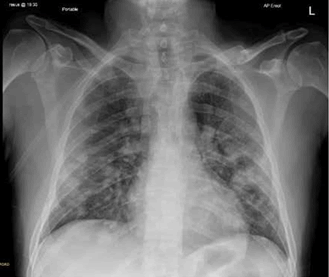
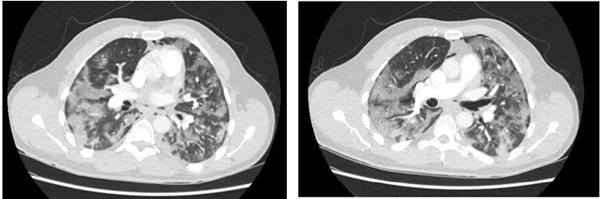
ECG showed normal sinus rhythm and initial chest Xray on admission was reported as bilateral patchy consolidation, in keeping with COVID-19 pneumonitis (Figure 1). Laboratory studies showed a markedly raised CRP of 130 with mildly raised white cell and neutrophil count, 12.3 X109/L and 10.3 X 109/L, respectively. Other relevant results included a lymphopenia of 1.0 X109/L and Lactate dehydrogenase (LDH) of 985 u/L. PCR on admission was also positive for COVID-19. Patient was commenced treatment for COVID-19 pneumonitis including 6 Litres of supplementary oxygen, dexamethasone 6 mg once daily, course of IV benzylpenicillin and clarithromycin and enhanced venous thromboembolism prophylaxis (Tinzaparin 4.500 units twice daily). Due to late presentation and increasing oxygen requirement, a computed tomography pulmonary angiogram (CTPA) was requested 24 hours post admission to rule out a pulmonary embolism. This was reported as showing extensive consolidation throughout the lungs, compatible with COVID-19 pneumonitis. No evidence of PE but there was evidence of small volume pneumomediastinum (Figure 2). This was discussed with the specialist respiratory team who advised for conservative management. During admission patient was noted to suffer acute confusion and paranoia. They became very suspicious of all treatment provided and regularly contacted their next of kin for reassurance and support. This was thought to be steroid induced psychosis and hence dexamethasone was stopped. Symptoms settled thereafter. Patient was eventually weaned off oxygen and discharged home after 6 days.
Differential Diagnosis
Given the context of worsening dyspnoea and hypoxia in the presence non cardiac sounding chest pain, the main working differential diagnosis was acute pulmonary embolism. This remains entirely reasonable given the well documented increased thromboembolic risk associated with COVID-19 infection and the late presentation of the patient. Additionally, there were no clinical signs suggestive of SPM or pneumothorax.
Treatment
Patient was commenced treatment for COVID-19 pneumonitis including 6 Litres of supplementary oxygen, dexamethasone 6 mg once daily, course of IV benzylpenicillin and clarithromycin and enhanced venous thromboembolism prophylaxis (Tinzaparin 4.500 units twice daily). Unfortunately, the treatment plan was complicated by the onset of steroid induced psychosis and hence the dexamethasone was stopped after 3 days. The oxygen requirement was eventually weaned off after 6 days and the IV antibiotics were switched to oral amoxicillin. This patient did not require any chest physiotherapy or any form of mechanical ventilation.
Outcome and Follow-up
This patient was successfully discharged from hospital after 6 days. The patient was oxygen independent and free of chest pain. The symptoms relating to the steroid induced psychosis had completely resolved. This patient is due a repeat CXR in six weeks post discharge and will be followed up by the respiratory team in one to two months.
Discussion
We hope that the current case presentation adds to the growing body of evidence regarding complications in COVID-19 infection. The undetectable clinical findings specific to SPM such as Hamman’s sign is not surprising in this case, given that they have been found to be present in only a 5th of SPM cases [10]. Similarly to previous cases, the SPM was associated with raised LDH which was managed conservatively with good recovery.
However, SPM remains an exceedingly rare presentation of COVID-19 infection, with many existing reports documenting the use of mechanical ventilation and or presence of predisposing factors. The lack of either of these elements in the current case, highlights the possibility that COVID-19 infection itself presents a significant risk factor for developing SPM. The pathophysiological mechanism proposed in earlier reports have suggested that air leak could be related to significant alveolar damage, making the alveolar wall more prone to rupture [5]. This critical learning point will encourage clinicians to firstly consider SPM as a possible differential, in COVID-19 positive patients with on-going hypoxia and chest discomfort. This is particularly important as the clinical presentation of SPM can often be ignored or misdiagnosed because of its vague symptoms [6] and hence a high degree of clinical suspicion is warranted. Furthermore, these reports will also encourage clinicians to take care in mitigating reasons of increased alveolar pressure in these patients as highlighted in previous reports [5].
Given the delay in presentation to hospital, it is important to consider whether this is a recovered case of COVID-19 in patient who has subsequently suffered a SPM or whether this is an acute case of COVID-19 complicated by SPM. Given the clinical history and radiological findings demonstrating extensive consolidation, it is likely that the current case represents on-going acute COVID-19 infection complicated by SPM. Furthermore, the patient did not describe any period of recovery since onset of symptoms. Therefore a recovered case of COVID-19 infection followed by SPM is unlikely [11].
Steroid induced psychosis on the other hand is a well-documented phenomenon, with high dose steroids being reported as a significant risk factor for psychosis. This patient was prescribed 6 mg dexamethasone once daily; they did not have any previous history of psychiatric illness and symptoms quickly resolved after the dexamethasone was stopped. The patient’s symptoms started approximately 2-3 days after starting dexamethasone treatment. This is in line with previous research that states typical time to developing symptoms is within 3-4 days [12] and is usually associated with taking equivalent of 40 mg prednisolone or more (6 mg dexamethasone is equivalent to 40 mg prednisolone). Collectively we can be confident that the psychotic episode was secondary to medication.
Conclusion
We have presented a rare care of COVID-19 infection complicated by SPM, which we hope adds to the growing body of evidence emerging from the COVID-19 Pandemic. The exact pathophysiology behind the development of SPM in these cases is unclear. However, the growing body of evidence of such complications cannot be ignored. Whilst it is possible that the two are independent diagnoses, the evidence in this case suggests otherwise. We hope that the current report helps to raise clinical suspicion of SPM in these patient’s, which will in turn lead to early diagnosis, treatment and also prevention.
Acknowledgement
The author would like to acknowledge their team for supporting the project.
Conflict of Interest
The author declared that there is no conflict of interest.
References
- Long-quan L, Huang T, Wang YQ, Wang ZP (2020) COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis J Med Virol 92(6):577-583.
- Ivan Macia, Juan Moya, Ricard Ramos (2007) Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg. 31(6):1110-4.
- Noppen M (2010) Spontaneous pneumothorax: epidemiology, pathophysiology and cause. Eur Respir Rev 19: 217â??219.
- Sahni S, Verma S, Grullon J (2013) Spontaneous pneumomediastinum: Time for consensus. N Am J Med 5(8):460-4.
- Elhakim TS, Abdul HS, Romero CP, Rodriguez-Fuentes Y (2020) Spontaneous pneumomediastinum, pneumothorax and subcutaneous emphysema in COVID-19 pneumonia: A rare case and literature review. BMJ Case Reports.
- Koullias GJ, Korkolis DP, Wang XJ, Hammond GL (2004) Current assessment and management of spontaneous pneumomediastinum: Experience in 24 adult patients. Eur J Cardiothorac Surg 25:852.
- Wang J, Su X, Zhang T (2019) Spontaneous pneumomediastinum: A probable unusual complication of coronavirus disease 2019 (COVID-19) pneumonia. Korean J Radiol 21(5): 627â??628.
- Wang W, Gao R, Zheng Y (2020) COVID-19 with spontaneous pneumothorax, pneumomediastinum and subcutaneous emphysema. J Travel 27(5):taaa062.
- Sun R, Liu H, Wang X (2020) Mediastinal emphysema, giant bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol 21(5):541-544.
- Sonu, Sameer, Jinette (2013) Spontaneous Pneumomediastinum: Time for Consensus. N Am J Med Sci 5(8): 460â??464.
- Brogna B, Bignardi E, Salvatore P (2020). Unusual presentations of COVID-19 pneumonia on CT scans with spontaneous pneumomediastinum and loculated pneumothorax: A report of two cases and a review of the literature. Heart Lung 2020 49(6): 864â??868.
- Gagliardi JP, Muzyk AJ, Holt S (2010) When steroids cause psychosis. October 1, 2010.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences