Sebaceous Gland Ectopia of the Esophagus: A Challenging Clinical Diagnosis
Antonietta Baffa, Domenico Coppola*
Departments of Anatomic Pathology, Florida Digestive Specialists and Moffitt Cancer Center and Research Institute, Tampa, USA
- *Corresponding Author:
- Domenico Coppola
Departments of Anatomic Pathology,
Florida Digestive Specialists and Moffitt Cancer Center and Research Institute, Tampa,
USA,
E-mail: domenico.coppola@FDHS.com
Received date: August 16, 2022, Manuscript No. IPMCRS-22-14361; Editor Assigned date: August 19, 2022, PreQC No. IPMCRS-22-14361 (PQ); Reviewed date: August 29, 2022, QC No. IPMCRS-22-14361; Revised date: September 08, 2022, Manuscript No. IPMCRS-22-14361 (R); Published date: September 15, 2022, DOI: 10.36648/2471-8041.8.8.239.
Citation: Baffa A, Coppola D (2022) Sebaceous Gland Ectopia of the Esophagus: A Challenging Clinical Diagnosis. Med Case Rep Vol.8 No.8: 239.
Abstract
Sebaceous Gland Ectopia (SGE) is a term defining the presence of normal sebaceous tissue in an unusual location. This condition is rare and first has been described in ectodermal derived organs such as in oral cavity, palms and other locations. SGE has also been described in endodermal derived tissues including the esophagus. However, this latter condition is extremely rare and to date only a few cases have been reported in English medical literature. This phenomenon is believed to represent a form of acquired metaplasia. SGE is asymptomatic and usually is discovered during routine endoscopic examinations for other gastrointestinal complains and symptoms.
SGE is a benign entity and to date no cases of malignant transformation have been reported. Due to its benign nature, once the diagnosis of SGE has been confirmed, no further work up or follow up is necessary. There is also no need to treat this condition. However, careful histopathology examination is important to differentiate this entity from malignant and infectious conditions, which are more common and can be clinically and endoscopically similar. In this report we present two cases of SGE arising in the esophagus of two female patients, who presented with complaints of gastro-esophageal reflux and underwent endoscopy.
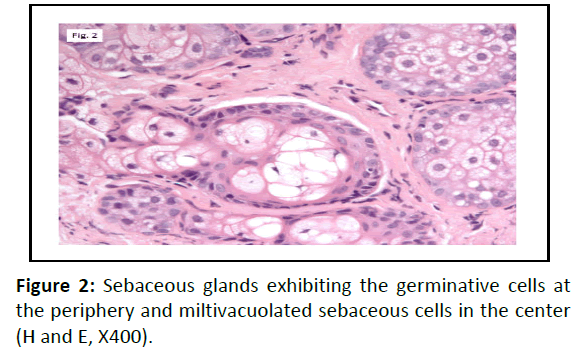
These lesions presented as patchy yellow-white nodules in the mid and upper esophagus and they were endoscopically interpreted as suggestive of candidiasis or glycogen acanthosis. Biopsies showed foci of non-keratinizing squamous mucosa overlying sebaceous glands. These glands exhibited a characteristic lobulated structure with germinative cells at the periphery and vacuolated well differentiated cells in the center of the lobules. After careful histologic examination and special stains the endoscopic impressions of candidiasis and acanthosis were ruled out and the final diagnosis of sebaceous ectopia was made. There was no evidence of dysplasia or malignancy in our cases.
Keywords
Sebaceous gland ectopia; Sebaceous ectopia; Esophageal sebaceous ectopia
Introduction
Sebaceous Gland Ectopia (SGE) is a term denoting the occurrence of normal sebaceous tissue in an unusual location [1]. The presence of ectopic sebaceous glands was first described in lips and oral cavity by Fordyce in 1896 as intra oral sebaceous granules and the condition was called Fordyce's disease [2,3].
SGE is a rare, commonly arising from the ectodermal derived tissues, such as oral cavity, genitalia, eyes, orbits, palms and soles. The occurrence of sebaceous ectopia in tissues with endodermal origin, e.g. esophagus, is extremely rare and only a few cases have been reported in English medical literature. In 1962 esophageal sebaceous ectopia was first described by La Pava and Pickren and since then less than 50 cases have been identified and presented in the medical literature. Before invention of endoscopic techniques, SGE was only a post mortem diagnosis [4,5].
The pathogenesis of esophageal sebaceous ectopia is not well known. It is postulated that the entity is an acquired metaplastic process but it could also represent a congenital abnormality. From the clinical standpoint, it is an asymptomatic condition with most of the cases being incidentally found during routine upper endoscopy for other reasons [4,6,7].
Macroscopically SGE is defined as multiple patchy yellowishgray nodules discovered during routine endoscopy. The number of nodules can be as high as 100 nodules and it can be located in any part of esophagus [6,8].
The presence of lobules of cells with sebaceous differentiation in the lamina propria and occasional proliferating basal cells within the epithelium are characteristic finding in SGE. The above histology is further supported by immunostains for keratins and epithelial membrane antigen which label both heterotopic sebaceous glands and bulbous nests [4,9]. As in a normal sebaceous gland, SGE includes an excretory duct. However, hair follicle within these ectopic glands have not been described [2,8,10].
Here we present two cases of esophageal SGE which were found during endoscopic studies for other GI complains and were endoscopically interpreted as possible fungal infection and glycogenic acanthosis.
Case Presentation
Case 1
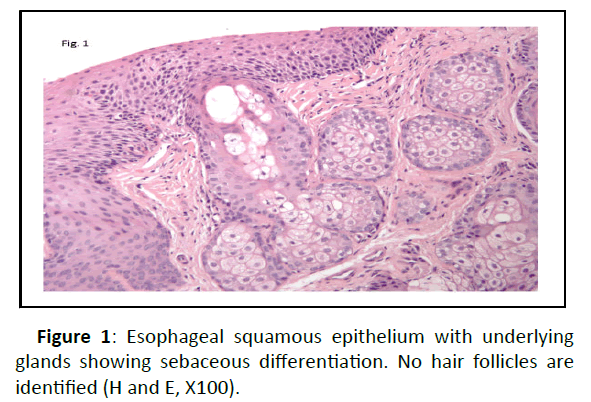
A 63 years old female patient underwent upper endoscopy for her GERD symptoms and dysphagia. The endoscopic study revealed multiple small, pale, submucosal plaques in esophagus. Multiple biopsies were taken with forceps and sent for further pathology examinations. Four fragments of tan tissue from mid/ distal esophagus measuring up to 8 x 2 x 1 mm were received in formalin. Histopathology examination result was consistent with squamous mucosa with atypical islands demonstrating apparent sebaceous differentiation (Figure 1) and reactive changes, negative for any dysplasia or malignancy. ABPAS study was negative for fungi and intestinal metaplasia.
Case 2
A 61 years old female underwent endoscopy following up her GERD, Barrett’s esophagus and gastroparesis symptoms. The endoscopic diagnosis was candidiasis and the sample was sent to pathology for further assessment. One fragment of tan tissue measuring up to 1 x 1 x 1 mm was received in formalin. Histopathology examination was consistent with reflux esophagitis. The squamous mucosa also revealed a focus of ectopic sebaceous glands (Figure 2). The ABPAS special stain was negative for fungi and intestinal metaplasia. There was no eosinophilic esophagitis, dysplasia or malignancy.
Discussion
It is hypothesized that metaplasia of a pluripotent stem cell, rather than derivation from islands of misplaced epidermis, is responsible for the development of ectopic tissue in a purely endodermal tissue [11]. Endoscopic and autopsy studies have not supported the embryological misplacement theory [2].
It has also been shown that ectopic Hedgehog signaling initiates the formation of sebaceous glands in areas of footpad normally lacking any hair follicles or its associated structures from epidermis. The Hedgehog pathway thus plays a key role in sebocyte cell development and might be a potential target for studying other similar disorders related to abnormal sebaceous gland function [12].
SGE have been described both in male and females. The SGE lesions are found mostly in the upper thoracic esophagus followed by middle and lower thoracic esophagus [13]. Histopathologically, it consists of lobules of polygonal cells with small nuclei and abundant clear cytoplasm showing typical sebaceous differentiation and is covered by a, 2-4 mm nonkeratinized stratified squamous epithelium with no to minimal lymphocytic infiltration [2].
SGE should be differentiated from infectious causes e.g. candidiasis and other noninfectious conditions such as glycogen acanthosis, sub mucosal and mucosal lesions including granular cell tumor, leiomyoma, papilloma2 ,carcinoid and xanthoma [7,14].
Xanthoma is an uncommon non-neoplastic lesion resulting from the accumulation of foamy histiocytes. In differentiating xanthoma from SGE it might help to know that in xanthoma the patient will have cutaneous manifestations associated with hyperlipidemia [14]. The most common site of Granular Cell Tumors (GCTs) is the esophagus where they are usually found as an incidental finding during endoscopy. In contrast to SGE, GCT presents as a single small nodule or plaque but with the same grayish-yellow appearance as seen in SGE [15]. Glycogenic acanthosis of the esophagus is a common benign entity, consisting of multifocal plaques of hyperplastic squamous epithelium and abundant intracellular glycogen deposits [16]. The cells containing intracytoplasmic glycogen are histologically empty and do not show the granularity seen in the sebaceous cells. Also, a PAS stain with diastase will confirm the presence of glycogen in glycogenic acanthosis.
Drinking, smoking or hyperlipidemias have not been implicated in the pathogenesis of SGE [13].
There was no evidence of dysplasia or malignancy detected in our cases. Surveillance follow up endoscopic studies at 8 months, 2 years and 5 years have shown no changes in number, size and behavior of sebaceous glands of SGE and there hasn’t been any malignant transformation reported within these lesions [2,10]. Due to the benign nature of this lesion, follow up endoscopic studies/or resection is not recommended [17].
If concomitant gastro esophageal reflux disease is present, it will be treated with anti-reflux regimens [2,7].
Conclusion
Considering the wide differential diagnosis that comes with this condition during endoscopic macroscopic studies, it is important to conduct careful histopathology examination and to properly differentiate this rare and benign condition from other commonly seen diagnoses. Exclusion of infections and malignant conditions will prevent further unnecessary work ups and treatments and will reassure patients.
Acknowledgements
We thank the Pathology Histology Laboratory at the Moffitt Cancer Center for the preparation of the stains.
References
- Marcial MA, Villafana M (1994) Esophageal ectopic sebaceous glands: Endoscopic and histologic findings. Gastrointes endosc 40: 630-632.
[Crossref], [Google Scholar], [Indexed]
- Bhat RV, Ramaswamy RR, Yelagondahally LK (2008) Ectopic sebaceous glands in the esophagus: A case report and review of literature. Saudi J Gastroenterol 14: 83-84.
[Crossref], [Google Scholar], [Indexed]
- De Felice C, Parrini S, Chitano G, Gentile M, Dipaola L, et al. (2005) Fordyce granules and hereditary non-polyposis colorectal cancer syndrome. Gut 54: 1279-1282.
[Crossref], [Google Scholar], [Indexed]
- Grube Pagola P, Vicuna Gonzalez RM, Rivera Salgado I, Alderete Vazquez G, Remes Troche JM, et al. (2011) Ectopic sebaceous glands in the esophagus. Report of three cases. Gastroenterol hepatol 34: 75-78.
[Crossref], [Google Scholar], [Indexed]
- Bae JY, Chon CY, Kim H (1996) Sebaceous glands in the esophagus. J Korean Med Sci 11: 271-274.
[Crossref], [Google Scholar], [Indexed]
- Bertoni G, Sassatelli R, Nigrisoli E, Conigliaro R, Bedogni G (1994) Ectopic sebaceous glands in the esophagus: Report of three new cases and review of the literature. Am J Gastroenterol 89: 1884- 1887.
[Crossref], [Google Scholar], [Indexed]
- Marin-Serrano E, Jaquotot-Herranz M, Casanova-Martinez L, Tur-Gonzalez R, Segura-Cabral JM (2010) Ectopic sebaceous glands in the esophagus. Rev Esp Enferm Dig 102: 141-142.
[Crossref], [Google Scholar], [Indexed]
- Hoshika K, Inoue S, Mizuno M, Iida M, Shimizu M (1995) Endoscopic detection of ectopic multiple minute sebaceous glands in the esophagus. Report of a case and review of the literature. Dig Dis Sci 40: 287-290.
[Crossref], [Google Scholar], [Indexed]
- Nakanishi Y, Ochiai A, Shimoda T, Yamaguchi H, Tachimori Y, et al. (1999) Heterotopic sebaceous glands in the esophagus: Histopathological and immunohistochemical study of a resected esophagus. Pathol Int 49: 364-368.
[Crossref], [Google Scholar], [Indexed]
- Wang WP, Wang WS, Tsai YC (2009) Multiple tiny ectopic sebaceous glands discovered throughout entire esophageal tract. Dig Dis Sci 54: 2754-2757.
[Crossref], [Google Scholar], [Indexed]
- Zak FG, Lawson W (1976) Sebaceous glands in the esophagus. First case observed grossly. Arch Dermatol 112: 1153-1154.
[Crossref], [Google Scholar], [Indexed]
- Allen M, Grachtchouk M, Sheng H, Grachtchouk V, Wang A, et al. (2003) Hedgehog signaling regulates sebaceous gland development. Am J Pathol 163: 2173- 2178.
[Crossref], [Google Scholar], [Indexed]
- Fukuchi M, Tsukagoshi R, Sakurai S, Kiriyama S, Horiuchi K et al. (2012) Ectopic sebaceous glands in the esophagus: Endoscopic findings over three years. Case Rep Gastroenterol 6: 217-222.
[Crossref], [Google Scholar], [Indexed]
- Bang CS, Kim YS, Baik GH, Han SH (2014) Xanthoma of the esophagus. Clin Endosco 47: 358-361.
[Crossref], [Google Scholar], [Indexed]
- Nie L, Xu G, Wu H, Huang Q, Sun Q, et al. (2014) Granular cell tumor of the esophagus: A clinicopathological study of 31 cases. Int J Clin Exp Pathol 7: 4000-4007.
[Crossref], [Google Scholar], [Indexed]
- Lopes S, Figueiredo P, Amaro P, Freire P, Alves S, et al. (2010) Glycogenic acanthosis of the esophagus: An unusually endoscopic appearance. Rev Esp Enferm Dig 102: 341-342.
[Crossref], [Google Scholar], [Indexed]
- Thalheimer U, Wright JL, Maxwell P, Firth J, Millar A (2008) Sebaceous glands in the esophagus. Endoscopy 40: E57.
[Crossref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences