Report on a Rare Case of Acute Coronary Syndrome with Suspected Vasculitis in a Young Girl
Shwetha S* and Thabit Ahmed
DOI10.36648/2471-8041.21.7.198
1Department of Pharmacy, Rajiv Gandhi University of Health Sciences, Bangalore
2Department of General Medicine, Baptist Hospital, Bangalore
- *Corresponding Author:
- Shwetha S Department of Pharmacy, Rajiv Gandhi University of Health Sciences, Bangalore, Tel: +9949595690; E-mail: shwethaklr@gmail.com
Received: August 03, 2021; Accepted: August 17, 2021; Published: August 24, 2021
Citation: Shwetha S, Ahmed T (2021) Report on a Rare Case of Acute Coronary Syndrome with Suspected Vasculitis in a Young Girl. Med Case Rep Vol.7 No.8.198
Abstract
Globally, cardiovascular disease remains a major cause of morbidity and mortality among young individuals, though with less predisposition to CVS risk factors compared to elderly. ACS in young, especially women has been very rarely reported and here we describe a case of ACS with suspected vasculitis in a 15 year old girl with pre-existing comorbidities of optic atrophy, renal hypoplasia.
Keywords
Acute coronary syndrome; Optic atrophy; Vasculitis; Renal hypoplasia; Aortoarteritis
List of Abbreviations
(CVS) Cardiovasvular System; (CVD) Cardiovaascular Disease; (ACS) Acute Coronary Syndrome; (AMI) Acute Myocardial Infarction; (CAD) Coronary Artery Disease; (ANA) Anti-Nuclear Antibody; (APLA) Antiphospholipid Antigen; (HIE) Hypoxic-Ischemic Encephalopathy; (PND) Paroxysmal Nocturnal Dyspnea; (RWMA) Regional Wall Motion Abnormality; (CAG) Coronary Artery Angiography; (LCX) Left Circumflex Artery; (PCI) Primary Coronary Intervention; (ESR) Erythrocyte Sedimentation Rate; (CRP) C-Reactive Protein; (RPR) Rapid Plasma Reagin; (TPHA) Treponema Pallidum Haemagglutination (SLE) Systemic Lupus Erythematosus; (DAPT) Dual Antiplatelet Agent; (TA) Takayasu Arteritis
Introduction
Cardiovascular disease (CVD) has been the leading cause of death throughout the world. In particular, acute coronary syndrome (ACS) is the main complication of CVD which includes unstable angina as well as an acute myocardial infarction (AMI). The characteristics and clinical course of the disease are rarely studied in younger individuals, as the incidence of ACS in younger people is much lower compared to older patients. It is reported that the incidence of AMI in those younger than 40 years of age is only about 5% in total, and 90% of these cases are men [1]. Previous studies have indicated that patients with early onset of coronary artery disease (CAD) exhibit preponderance of single-vessel disease and dominance of coronary risk factors such as hypercholesterolemia, family history of CAD and, cigarette smoking as compared to older patients [2]. Other possible contributing factors include substance abuse, coronary artery anomalies, hypercoagulable state and, oral contraceptive use in young women [3]. Based on angiographic characteristics, ACS in the young patients was found to be associated with both atherosclerotic and non-atherosclerotic CAD which includes arteritis, thrombosis, embolization, and spasm (cocaine abuse). Coronary artery thrombus can be noticed in hypercoagulable states such as protein C and S deficiency, antiphospholipid antigen (APLA), and nephrotic syndrome.
Coronary vasculitis is the least noticed cause of ACS. Vasculitis is a general term for inflammation of the blood vessel walls which can result in stenosis, occlusion, aneurysm or, rupture. It can be primary or secondary to an autoimmune disease or can be precipitated such as drugs, infections or, malignancy. Cardiac involvement occurs with variable frequency and can affect any of the cardiac layers [4].
Case Presentation
A 15 year old female presented to the hospital with complaints of retro-sternal chest pain for 3 days, worsening dyspnea for 7 days and, a history of paroxysmal nocturnal dyspnea (PND) gradually progressed to orthopnea. Past medical history includes right kidney hypoplasia with secondary hypertension diagnosed 5 months ago, for which she was on Amlodipine (5 mg) with Ramipril (2.5 mg). Bilateral optic atrophy with complete blindness at the age of 8 years following post meningoencephalitic sequelae.
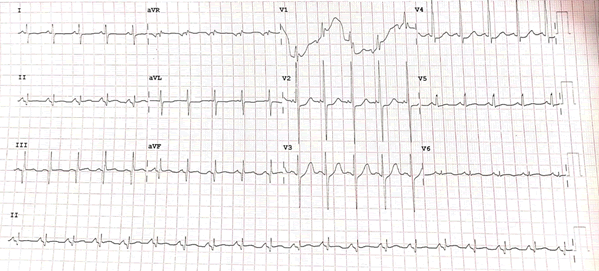
On examination she was tachycardic (PR-116/min), tachypneic (40/ min), and loud S3 gallop heard with a blood pressure of 90/60 mmHg. Electrocardiogram (ECG) showed ST depression in lateral leads with T wave inversions in V2-V4, Q waves in II, III, aVF (Figure 1). Cardiac enzymes were elevated. Bedside echocardiogram revealed regional wall motion abnormality (RWMA) involving the basal and mid-posterolateral wall and inferior wall hypokinesia with mild left ventricular systolic dysfunction, moderate MR (Mitral regurgitation) and, bilateral pleural effusion.
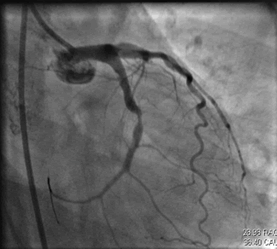
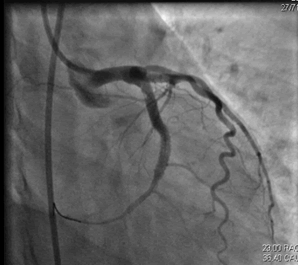
Initial differentials considered were ACS/Myocarditis/Vasculitis/ Takayasu arteritis. She was started on loading doses of dual antiplatelets (T. Aspirin 300 MG+ T. Clopidogrel 325 mg), high dose statin (T. Atorvastatin 80 mg), empirical antibiotics, diuretics, NIV and, supportive management. Given RWMA and elevated troponin I, coronary artery angiography (CAG) was performed which was suggestive of proximal LCX (Left Circumflex Artery) thrombus containing lesion with total occlusion Single vessel disease with a thrombotic lesion (Figure 2). Revascularization was considered as the preferred treatment strategy and successful angioplasty was done with stenting to the mid LCX (Figures 3 and 4). The procedure was uneventful as she developed spikes of fever and hypotension post PCI. Culture revealed Enterococcus in urine; hence antibiotics were hiked from Piperacillin tazobactum to Linezolid accordingly.
Laboratory tests showed a rise in cardiac enzymes, leukocyte count (16000 mm3), ESR, and CRP (135.5 mg/dl). Kidney and liver function with lipid profile and coagulation profile were normal. Results for syphilis (RPR and TPHA) were negative. Immunological markers, ANA and APLA were negative with low C3 levels.
An extensive workup for the cause of MI was done. Ophthal consult was sought opined as bilateral optic atrophy with probable vasculitis or syphilitic origin, however, RPR (Rapid Plasma Reagin) and other autoimmune serological markers were negative with only low C3 levels. Hence, SLE (Systemic Lupus Erythematosus) was ruled out and TA was considered. Optic atrophy is also not a typical feature of TA, hence it was attributed to past CNS infection.
Given hypoplastic kidney and optic atrophy, CT aortogram, cerebral and neck angiography was done to rule out aortoarteritis, which showed bovine aortic arch with mild wall thickening of the ascending aorta, part of aortic arch and origin of innominate and left common carotid artery, hypoplastic right kidney with chronic right renal artery stenosis and sub-endocardial fat deposits in the lateral and inferior wall of LV. But the criteria for the diagnosis of TA framed by the American college of rheumatology weren’t fulfilled.
CT chest showed bilateral effusion and alveolar hemorrhage. US chest revealed bilateral small pleural effusion attributed to pulmonary edema with sub-segmental atelectasis of the lung. USG abdomen with renal Doppler showed no evidence of significant renal artery stenosis in the visualized arteries. She was discharged on DAPT, statin, beta-blocker, and an ACE inhibitor.
Three months later repeat MR aortogram was done to look for aortoarteritis, which showed complete resolution, and hence the possibility of Takayasu arteritis was completely ruled out. As TPHA (Treponema pallidum hemagglutination assay) was non-reactive, syphilitic arteritis was also ruled out.
Two years later she presented with complaints of sudden onset bilateral lower limb pain with a tingling sensation from the past one week. Nerve conduction analysis was completely normal and MR angiogram head to toe was done to compare it with the previous CT angiogram, which showed no features of arteritis. She was medically managed for pain and was discharged at request.
Discussion
ACS is a life threatening condition with common risk factors of dyslipidemia, diabetes mellitus, hypertension and coronary vasospasm [5]. AMI in young adults remains a challenge in the present era, as the associated risk factors are different from that of the elderly population. As for the etiology is concerned, many factors contribute to an acute event. When a group of young patients were analyzed, a great proportion of them were free from significant atherosclerotic lesions, which indicates different mechanisms causing a coronary obstruction. A few of them which can trigger an ischemic event are non-atherosclerotic coronary disease, hypercoagulable states such as hyperhomocysteinemia and antiphospholipid syndrome, and substance abuse [6]. One of the least appreciated causes of ACS which is always subject to neglect by clinicians is coronary vasculitis, which makes this case a distinct one.
Coronary artery disease (CAD) in patients with vasculitis is due to active, uncontrolled coronary artery inflammation. Coronary arteritis (CA) may be asymptomatic in some cases, in others clinically significant CAD may be secondary to accelerated atherosclerosis rather than active inflammation of the arterial wall. The exact prevalence of CA among patients with systemic vasculitis is largely unknown because of the relative rarity of these conditions as well as the lack of standardized prospective imaging studies systemically evaluating the coronary vasculature [4].
Optic atrophy is the condition that affects the optic nerve, which carries impulses from the eye to the brain thereby causing significantly reduced vision. The causes of optic atrophy include hypoxic ischemic encephalopathy (HIE), hydrocephalus, infective, traumatic, congenital, inflammatory etiologies, of which HIE is the most frequent cause [7].
Renal hypoplasia refers to a congenitally small kidney where there is essentially normal residual parenchyma but smaller calyces, lobules and, papillae [8]. This predisposes the patient to develop urinary tract infections (UTI) and hypertension [9].
Vascular changes can lead to complications like hypertension, most often due to renal artery stenosis or more rarely due to stenosis of the suprarenal aorta, aortic insufficiency due to aortic valve involvement, pulmonary hypertension, and aortic or arterial aneurysm.
CT angiography showed mild wall thickening of ascending aorta, aortic arch, and left common carotid artery, suggesting likely arteritis. Though there was an elevation in the inflammatory markers, the diagnosis of TA was ruled out as other autoimmune serological markers were negative and the criteria for the diagnosis of TA according to the American college of rheumatology weren’t fulfilled [10]. On the basis of clinical manifestations, laboratory findings and angiographic findings, diagnosis of vasculitis was suspected, but all the immunological markers were negative. Hence, the patient was managed with successful angioplasty to the LCX artery and no immunosuppressant therapy was initiated.
Conclusion
Coronary vasculitis should always be considered as the differential diagnosis in young women with no medical history, presenting with myocardial infarction. In this clinical case, though there were no evident risk factors for AMI, other underlying inflammatory mechanisms may have contributed to this episode. More research is needed to evaluate chronic inflammatory profiles in patients with premature coronary disease.
Acknowledgement
None
Conflict of Interest
None
Funding
None
References
- Hamsten A, Bjorkholm M, Norberg R, De Faire U, Holm G (1986) Antibodies to cardiolipin in young survivors of myocardial infarction: an association with recurrent. Lancet.18;327(8473):113–6.
- Deora S, Kumar T, Ramalingam R, Manjunath CN (2016) Demographic and angiographic profile in premature cases of acute coronary syndrome: Analysis of 820 young patients from South India. Cardiovasc Diagn Ther. 6(3):193–8.
- Gupta S, Lakhani KK, Munshi H (2017) A study of risk factors in young patients of acute coronary syndrome. Int J Contemp Med Res. 4(10).
- Vasculitis of the Coronary Arteries: American College of Cardiology.
- Owlia MB, Sadoughi S (2016) Is acute coronary syndrome secondary to coronary vasculitis underestimated in daily cardiology practice?. Dly Cardiol Pract J Cardiol Ther. 23;3(2):504–5.
- Lisowska A, Makarewicz-Wujec M, Filipiak KJ (2016) Risk factors, prognosis, and secondary prevention of myocardial infarction in young adults in Poland. Kardiologia Polska. Via Medica p. 1148–53.
- Chinta S, Wallang BS, Sachdeva V, Gupta A (2014). Etiology and clinical profile of childhood optic nerve atrophy at a tertiary eye care center in South India. Indian J Ophthalmol. 62(10):1003–7.
- Renal hypoplasia | Radiology Reference Article | Radiopaedia.org.
- Renal hypoplasia. A congenital anomaly of the kidneys and urinary tract | infoKID.
- Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, et al. (1990) The American College of Rheumatology 1990 criteria for the classification of takayasu arteritis. Arthritis Rheum. 33(8):1129–34.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences