Pseudo Aneurysm of the Right Hepatic Artery after Laparoscopic Cholecystectomy a Case Study
Menoura R*, Bennia B, Rahmouni R, Satta S and Delmi A
Department of Surgery, B Constantine University Hospital, Algeria
- *Corresponding Author:
- Menoura R
- Department of Surgery, B Constantine University Hospital, Algeria,
- Tel: 213542573386;
- E-mail: raoufmenoura25@gmail.com
Received date: June 29, 2022, Manuscript No. IPMCR S -22-11902; Editor Assigned date: July 01, 2022, Pr QC No. IPMCR S -22-11902 (PQ ); Reviewed date: July 13, 2022, QC No. IPMCRS-22-11902; Revised date: July 22, 2022, Manuscript No. IPMCRS-22-11902(R); Published date: July 29, 2022, DOI: 10.36648/2471-8041.8.7.214.
Citation: Menoura R, Bennia B, Rahmouni R, Satta S, Delmi A (2022) Pseudo Aneurysm of the Right Hepatic Artery after Laparoscopic Cholecystectomy A Case Study. Med Case Rep Vol:8 No:7
Abstract
Post laparoscopic cholecystectomy traumatic pseudo aneurysms are rare and manifest as late hemobilia which is difficult to diagnose and manage. This condition mainly affects the right branch of the hepatic artery and the prognosis is poor. We report a case study of an individual diagnosed with a pseudo aneurysm 10 days after laparoscopic cholecystectomy.
Following radiological exploration, a hemobilia was identified on the 10th postoperative day. In this case, selective embolization was not possible, and therefore a ligation of the right hepatic artery was initiated. The postoperative period was marked by the reappearance of hemobilia evoking the diagnosis of vascular shunts in the hepatic hilum, and double ligation of the right hepatic artery was required.
Keywords
Pseudo aneurysm; Laparoscopic vascular trauma; Right hepatic artery trauma; Hemobilia
Introduction
Laparoscopic cholecystectomy carries the risk of iatrogenic vascular and biliary trauma, especially in countries where this technique is not commonly practiced. Pseudo aneurysms represent one of these rare but poor prognostic complications. They are difficult to diagnose because they are asymptomatic [1]. The potential evolution of pseudo aneurysms towards rupture requires rapid diagnosis and management. Surgery is the last resort if interventional radiology fails.
Case Report
The patient was KZ, 44 years old, with a medical history of gravidic hypertension, operated for vesicular lithiasis for which a laparoscopic cholecystectomy was performed. The surgeon noted a hemorrhagic accident which he controlled with several clips.
On the 10th postoperative day, the patient presented with a hemorrhagic syndrome with melena, hematemesis, jaundice, dark urine and discolored stools. She was readmitted to the hospital in her home town. A biological examination was performed identifying a cholestasis syndrome made of: total bilirubin at 2 × N, direct bilirubin at 3.5 × N, PAL at 3.5 × N and a hepatic cytolysis syndrome: TGO at 2 × n, lipasemia at 19 × N. An abdominal CT scan was performed and identified dilatation of the intra- and extra-hepatic bile ducts without detectable obstruction with stage B pancreatitis.
The patient was referred to our center where a fibroscopy was performed to explore her bleeding and identified erythematous antral gastritis and a blood clot attached to the papilla asserting the diagnosis of hemobilia [1]. A hepatic echodoppler was performed and identified a vascular structure at the level of the hepatic hilum dilated to 20 mm, partially thrombosed, with arterial flow corresponding to an aneurysm of the partially thrombosed hepatic artery. An abdominal angioscan confirmed the diagnosis of a false aneurysm and the presence of surgical metal clips around the right hepatic artery and the absence of a biliary fistula. The patient was put on proton pump inhibitor in electric syringe pump, sandostatin and absolute young. Due to the unavailability of an embolization center, the patient was brought to the operating room for surgical exploration which revealed aneurysmal sac in the hepatic hilum, and an undiluted bile duct and clear bile.
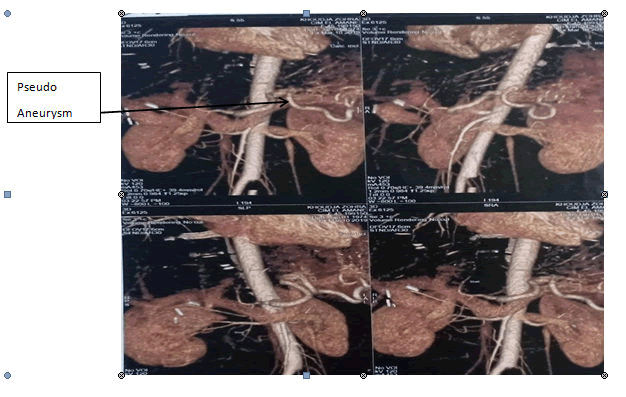
Dissection of the hepatic hilum elements, dissection of the common hepatic artery, gastro duodenal artery, dissection and ligation of the right hepatic artery arising from the superior mesenteric artery without sectioning was performed. The postoperative evolution was marked 10 days later by hypertensive peaks, reappearance of abdominal pain and bleeding syndrome (Figure 1).
Discussion
Pseudo aneurysms are distinguished from true aneurysms by the wall of the artery which is preserved, pseudo aneurysms which are a blood mass caused by vascular trauma surrounded by the tissues surrounding the affected vessel. The hepatic arteries tend to become the first location of traumatic aneurysms due to the development of numerous radiological techniques, particularly laparoscopic techniques on the liver and interventional radiology and hepatobiliary surgery [2-5]. Their evolution is classically described as an increase in size with a risk of rupture in the bile ducts, portal system, jejunum, or peritoneal cavity.
However, in the absence of complications, these false aneurysms remain asymptomatic, and are discovered either on the occasion of the appearance of clinical signs: hepatic colic, jaundice and haemobilia, the triad of Quincke [6,7,8]. A recent study showed that laparoscopic cholecystectomy was associated with an increased risk of hemobilia compared to the conventional open approach [1,9,10]. Laparoscopy has replaced the open route for cholecystectomy but the risk of biliary injury is increased. It is 0.5% while it is 0.2% by open approach [11]. The mortality rate in the laparoscopic approach is around 20% in case of rupture [12,13]. The exact incidence of these traumas under laparoscopy is not known.
On the one hand, this type of accident is rarely published; on the other hand it is likely that ligation of the right branch of the hepatic artery can sometimes go unnoticed [3]. The importance of the clinical manifestations as well as their early or delayed onset depends on the mechanism, location and complexity of the lesions. In the case we report, the injury to the arterial wall resulted in the formation of a false right branch aneurysm of the hepatic artery which was revealed secondarily by a hemobilia. Several cases of post cholecystectomy aneurysms have been described [13]. Pulsed echodoppler can guide the diagnosis of arterial aneurysm and guide percutaneous embolization [13,14]. Coeliomesenteric arteriography is the essential examination to make the diagnosis and identify the lesion and specify its exact location [14,15]. Radiological embolization provides the most effective way to control the bleeding. This will avoid the surgical difficulties associated with inflammatory lesions of the hepatic pedicle and the risk of injury to the hepatic artery or the main bile duct during dissection [2].
It is considered the most effective therapeutic weapon for treating pseudo aneurysm [16]. Having become the therapy of choice after selective catheterization, the use of micro-coils allows the exclusion of the false aneurysm and the preservation of the arterial branch. The success rate ranges from 81 to 96% [17]. Percutaneous embolization represents an effective alternative in interventional radiology centers [16]. In our case, since arterial embolization was not possible, we decided to perform a surgical procedure in which a ligation of the right hepatic artery was performed.
On the tenth postoperative day, the reappearance of hemobilia j was noted, highlighting the importance of the vascular anastomoses within the hepatic hilar plaque, particularly between the right and left hepatic arteries [14]. Consequently, proximal and distal ligation of the right hepatic artery has become the treatment of choice, successfully performed in our case. Patient who progressed well postoperatively and was discharged after 7 days.
Conclusion
Laparoscopic cholecystectomy carries the risk of trauma to the hepatic artery, particularly its right branch. Hemobilia is the main clinical sign and the diagnosis is made by mesenteric arteriography. The importance of the vascular anastomoses of supplements (shunt) within the hepatic hilar plaque, in particular between the right hepatic artery and the left hepatic artery, imposes a double high and low ligation with respect to the pseudo aneurysm of the right hepatic artery or the left hepatic artery.
References
- Green MHA, Johnson CD, Jamienson NV (2001) Br J Surg 88:773-786
- Pilleul F (2001) Prise en charge des hepatic artery aneurysms. Press Med 30:1139-1142
- Shanley CJ, Messina LM, Shah NL (1996) Common splanchnic artery aneurysm: splenic, hepatic, and celiac. Ann Vasc Surg 10:315-322
- Fabian TC, Stanford GG (1991) Factors affecting morbidity following hepatic trauma: a prospecting analysis of 482 injuries. Ann Surg 213:540-541
- Marcheix B, Cron C (2004) Embolisation transhépatique percutannée d’un pseudoanevrysme posttraumatique de l’artère hépatique. Ann chir 129:603-606
- Regent D, Meyer-Bisch L, Barbary-Lefèvre C, Corby-Ciprien S, et al. (2006) La douleur biliaire : comment la reconnaître ? Comment l’explorer ? J Radiol 87:413-428
- Sandblom P (1948) Hemorrhage into the biliary tract following trauma: ‘‘traumatic hemobilia’’. Surg 24-571-586[Crossref]
- QUINKE H (1871) Ein Fall von Aneurysma der Leberarterie. Bert k/in Wschr 8:349-351
- Stewart BT, Thomson KR, Collier NA (1995) Postcholecystectomy haemobilia: enjoying a renaissance in the laparoscopic era? Aust N Z J Surg 65:185-188
- Antonio BSK, Fabiani P, Benizri EI, Sophie (1995) Place de l’endoscopie dans le diagnostic et le traitement des complications biliaires après cholecystectomie laparoscopique. Gastro Clin Biol 19:95-96
- Club SS (1991) A prospective analysis of 1518 laparoscopic cholecystectomies. N Engl J Med 324:1073-1078
- Saltzberg SS, Lamparello PJ (2005) Is Endovascular Therapy the Preferred Treatment for All Visceral Artery Aneurysms? Ann Vasc Surg 19:507-515
- Kelley CJ, Hemingway AP, Mcpherson GAD, Allison DJ, Blumgart LH, et al. (1983) Non-Surgical management of post cholecystectomy hémobilia. 70:502-504
- Abboud B, GA, Thome C, Atallah N, Ghanem S, Farah P, et al. (1994) Hepatic artery aneurysm treated by embolization. J Chir (Paris) 131:252-256
[PubMed]
- Laccarino V, Santini G, Noce DM, Trivellini V (1995) Non-surgical treatment of pseudoaneurysm of the hepatic artery and its branches. Radiol Med 89:841-845
- Genyk YS, KF Halpern NB, (1994) Hepatic artery pseudoaneurysm and hemobilia following laser laparoscopic cholecystectomy. Surg Endos 8:201-204
- Akin T, Harlaftis NN (1977) Hemobilia from ruptured hepatic artery aneurysm: Report of a case and review of the literature. Am J Surg 133:229-232

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences