Precocious Puberty: Case Series
Emmanuel Ameyaw
DOI10.21767/2471-8041.100051
Emmanuel Ameyaw*
Department of Child Health, Komfo Anokye Hospital, Ghana
- *Corresponding Author:
- Emmanuel Ameyaw
Head, Department of Child Health
Komfo Anokye Hospital
P.O. Box 1934, Kumasi, Ghana
Tel: +233-20-8403784
E-mail: ekameyaw@yahoo.com
Received Date: April 30, 2017; Accepted Date: May 15, 2017; Published Date: May 17, 2017
Citation: Ameyaw E. Precocious Puberty: Case Series. Med Case Rep, 3:2. DOI: 10.21767/2471-8041.100051
Abstract
Precocious puberty is a condition characterized by the development of secondary sexual characteristics before the median age for sex. It can be central (gonadotropin dependent) also called true precocious puberty or peripheral (gonadotropin independent) also known as pseudo precocious puberty. Two Ghanaian children with central and pseudo precocious puberty are being presented. The central precocious puberty was due to arachnoid cyst in the brain of a 4-year-old boy whilst the pseudo precocious puberty was as a result of granulosa cell tumour of the right ovary. No such cases have, previously, been reported in Ghana.
Keywords
Precocious puberty; Children; Ghana
Introduction
Precocious puberty is defined as the onset of secondary sexual characteristics before 9 years in males and before 8 years in females [1,2]. This is due to excessive production of sex steroids which could be due to activation of hypothalamicpituitary- gonadal axis or due to a non-hypothalamic mediated increase in sex steroid production [3]. Out of these two, central precocious puberty is more common and accounts for more than 90% in girls and about 50% in boys presenting with the disorder.
Arachnoid cyst is a rare congenital cerebral malformation that has been reported as a cause of central precocious puberty [4,5]. Over the past several decades granulosa cell tumour of the ovary has been reported as a cause of peudo precocious puberty in girls [3,6-8]. No case of precocious puberty, in the past, has been reported in Ghana. The author reports two cases of precocious puberty in Ghana.
Case Presentation
Case 1
A 4-year-old boy presented with big head, acne, axillary and pubic hair, big penis and testes.
Parents realized that his head was growing big at 8-months of age and reported to a hospital but they were assured that he was growing well. The head continued to increase in size and at the age of 3 years it was realized that he was growing axillary and pubic hair and had developed adult body odor and acne.
The penis had further increased in size. About the same time, he was seen to have grown taller and bigger than his classmates. The parents at this time thought the child had developed a “spiritual disease” and so they took him to a spiritualist.
However, after several months of follow up at the spiritualist shrine the child did not improve and so he was brought to the pediatric endocrine clinic at Komfo Anokye Teaching Hospital.
He was delivered at term via spontaneous vaginal delivery, birth weight 3.2 kg, height not taken, cried at birth, was healthy and normal in the neonatal period.
He had neck control at 9 months, sat at 1 year, walked at 2.5 years.
The mother is 28 yrs and a house wife, father is 34 yrs, and he is a business man. They are not married but cohabiting, non-consanguineous.
On examination weight=33 kg (> 97th percentile), height=129.5 cm (> 97th percentile), head circumference=61.5 cm (> 97th precentile), (father: weight=92 kg, height=184 cm, mother: weight=72 kg, height=160 cm) he looked big for his age, he has extensive acne of the face, big head, no café au lait spots on the body, no goiter.
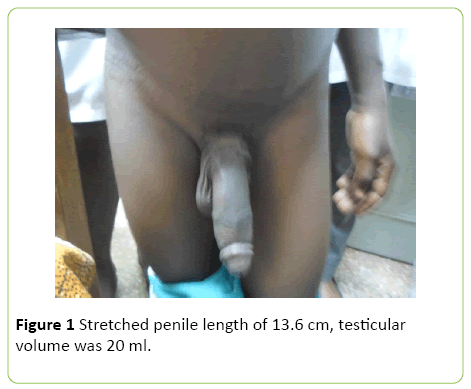
He has axillary hair, pubic hair=Tanner stage 5, Stretched penile length of 13.6 cm, testicular volume was 20 ml (Figure 1).
Laboratory Investigations:
17 hydroxyprogestrone 2.4 nmol/L (0.1-2.7)
Testosterone 9.2 nmol/L (0.07-1.04)
Growth hormone 0.11ug/L (random) (<5.4)
FSH Basal 2.3 U/L (Basal follicular phase 3.0-8.1, Adult Male 13-70 yrs 1.0-12.0)
sFSH at 20 min=2.4 U/L
sFSH at 30 min=2.5 U/L
sFSH at 60 min=2.2 U/L
LH Basal=1.8 U/L (Basal follicular phase=2.9-21.7; Adult male 20-70 yrs=1.8-8.2)
sLH at 20 min=3.1 U/L
sLH at 30 min=2.8 U/L
sLH at 60 min=1.9 U/L
TSH=0.77 uIU/ml (0.7-5.9)
FT4=10.9 pmol/L (8.7-16.2)
S- Prolactin=12.70 ug/L (2.64-13.13)
Cortisol 427.1 ng/ml, early morning (50-250)
Dexamethasone suppression test: < 25
Hemogram:
Hemoglobin 14.2 g/dl, WBC=9 × 109/L,
Neutrophils 38%,
Lymphocytes 51%,
Electrolytes:
Sodium=141 mmol/L
Potassium=4.1 mmol/L
Chloride=107 mmol/L
Urea and creatinine:
Urea=3.5 mmol/L (2.5-7.5)
Creatinine=80 umol/L (Male: 53-125, Female: 40-110)
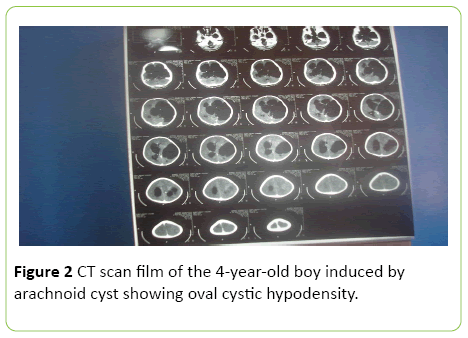
CT scan report: A large left cystic hypodensity in the left temporo-parietal region. Also, another oval cystic hypodensity in the midline causing widening of the 3rd ventricle and extends to the sella/supra sella region. Associated hypoplasia of the left temporo-occipito-parietal lobe is seen, there is associated asymmetrical dilatation of the lateral ventricles. Mid line shift to the right, 4th ventricle appears normal.
Cerebral CT scan film:
Case 2
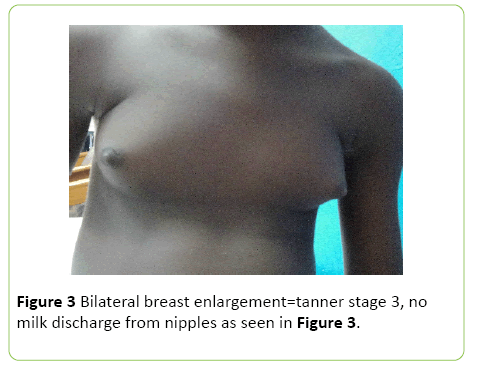
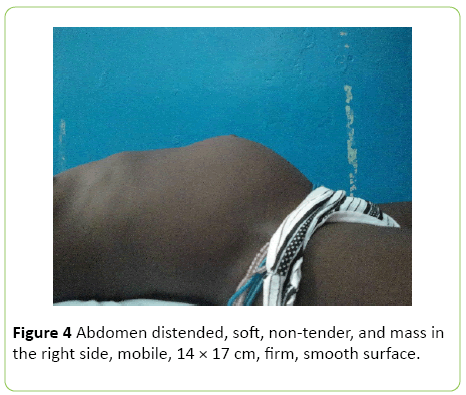
A 5-yr-old girl was referred to the pediatric endocrine clinic with abdominal mass of 2 months duration, bilateral breast enlargement 1½ months.
She was well till about 2 months prior to presentation she developed abdominal mass which was slowly enlarging. Breast was also noticed to be progressively enlarging.
She was a product of a term delivery, neonatal and post neonatal period was uneventful. She received all immunization. There has been no concern with developmental milestone till she developed above clinical features.
She has 5 other siblings who are all well and they are attending school at various grades. Parents were married, nonconsanguineous, father 45 years, an electrical welder, mother 39 years, petty trader.
Examination revealed a well looking girl, weight=20 kg (75th percentile on WHO growth chart) height=113 cm (90th percentiles on WHO growth chart), no skin lesions, no palpable lymph, no goiter.
Pubic hair=Stage 2,
Breasts were bilaterally enlarged, Tanner stage 4.
Pulse is 90 min, Blood pressure 90/60 mmHg.
Vaginal exam: No active bleeding, no spotting, no vaginal discharge, no digital examination was done.
Laboratory Investigations:
Biochemistry:
Cholesterol 2.64 mmol/L (3.90-5.20)
Urea 5.33 mmol/L (2.50-8.30)
Creatinine 44 umol/L (44-106)
Phosphate 5.56 mmol/L (0.87-1.45)
Uric acid 180 umol/L (143-339)
Hematology:
Hemoglobin=7.6 g/dl
WBC=13.01 (2.60-8.50)
HCT=23% (40-54)
MCV=75.6 fl (80-100)
MCH=24.1 pg (27-30)
PLT=661 × 10 (150-400)
Neutrophiles 65.3% (25-75)
Lymphocytes=22.4% (25-60)
s-17β estradiol=242 pmol/L
Range for non-pregnant women
Mid follicular phase 88-416
Peri ovulatory 226-1949
Mid luteal phase 292- 996
S Follitropin (FSH)=0.98 IU/L
FSH reference ranges for non-pregnant women
Mid follicular phase 3.83-8.78
Mid cycle 4.54-22.51
Mid lutheal phase=1.79-5.12
s-LH=0.67 IU/L
Abdominal USG: Large solid cystic supra-pubic mass, with central necrosis, measuring 14.1 × 13.7 × 97 cm, minimal flow noticed on color Doppler. Normal appearance of the left ovary is seen; as well as normal uterus and bladder. Their mass was consistent with the right ovary. No pelvic fluid collection, normal liver, spleen and kidneys, no intra-abdominal lymadenopathy.
USG revealed right ovarian tumour.
Histology of the ovarian mass: Granulosa cell tumour of the right ovary.
Impression: Peripheral precocious puberty in a 5 year old girl secondary to right ovarian granulose tumour.
Discussion
Central precocious puberty occurs as a result of the premature release of luteinizing hormone releasing hormone (LHRH) from the hypothalamus in a child. The LHRH stimulates the secretion of pituitary gonadotropins, luteinizing hormone (LH) and follicle stimulating hormone (FSH), which in turn stimulate the gonads to produce sex steroids [3,5]. The levels of LH, FSH, and LHRH stimulation help differentiate central precocity from the peripheral one. Cerebral arachnoid cysts are a rare but known cause of central precocious puberty [4,5,9]. Other central nervous system lesions resulting in sexual precocity include hypothalamic hamartomas, postencephalitic scars, tubercular and bacterial meningitis, head trauma, hydrocephalus, tuberous sclerosis, various brain tumors, meningomyelocele and primary hypothyroidism [3]. Case 1 had central precocious puberty because he presented with bilateral testicular enlargement, penile enlargement, rapid somatic and skeletal growth and increased gonadotropins. His had a bone age 12.5 years at 4 years of age, implying that he would have final short stature in adult life due to early fusion of epiphyseal growth plates [3,5]. Arachnoid cysts are intraarachnoid collections of cerebrospinal fluid (CSF) and account for 1% of all intracranial space occupying lesions [9,10]. They cause neurological dysfunction through expansion that can compress neural tissue and obstruct CSF flow [3].
In peripheral precocious puberty, secondary sex characteristics appear without maturation of gonads and there is no activation of hypothalamo-pituitary-gonadal axis. It is due to endogenous and/or autonomous secretion of sex steroids or iatrogenically due to exogenous administration of sex steroids [6,8]. Causes of peripheral precocious puberty include ovarian tumours, ovarian cysts, adrenal tumours and congenital adrenal hyperplasia [3,6,7]. McCune Albright syndrome can both stimulate the ovaries and testes to produce excessive sex steroids, without the involvement of the hypothalamus and the pituitary gland, to produce precocious puberty [3]. Case 2 had pseudo-precocious puberty due to over stimulation of the right ovary from granulosa cell tumour. Granulosa cell tumors of the ovary are relatively uncommon neoplasms, representing approximately 5% to 10% of all ovarian malignancies [3,6,7]. These tumours belong to the group of ovarian sex-cord stromal tumors. The majority of patients with these tumours are adults, but 5% are pre-or peripubertal. They are thought to arise from the granulosa cells of the ovary [8]. Granulosa cells constitute the somatic component of the ovarian follicle and function to produce sex steroids and other growth factors required for folliculogenesis and ovulation [6,8,11].
Conclusion
Early diagnosis and appropriate management of children with precocious puberty is important to avert associated complications due to the primary cause and to improve on the final adult height [3]. For males with central precocious puberty neuroradioimaging is mandatory [9,10]. Case 1 had cerebral CT scan that showed cerebral arachnoid cyst and hydrocephalus. Parents thought he rather had a “spiritual disease” and so they rather sought the assistance of spiritualist [12]. For nearly one year he was treated and followed up at a spiritualist center without improvement. This practice whereby people with chronic illnesses eventually seek assistance from alternative medical practitioners including spiritualists is common in Ghana. This leads to delay in diagnosis and management of otherwise treatable conditions.
All girls with precocious puberty should have abdominopelvic ultrasound examination done to look at the ovaries, the uterus and the adrenal glands [3,6]. Case 2 had right ovarian tumour which on histology was found to be granuloma cell tumour.
Case 1 had normal thyroid profile, prolactin and 17 hydroxyprogesterone whilst gonadotropins and testosterone levels were increased. Case 2 had low gonadotropins but increased estrogen levels.
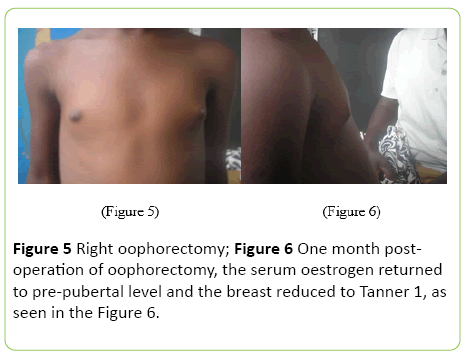
Case 1 had cerebral surgery to excise the arachnoid cyst and to drain the excessive CSF and a shunt was put in. He was then put on intra muscular leuprolide acetate every three months. Case 2 had right oopherectomy and one month post operation the serum oestrogen returned to pre-pubertal level and the breast reduced to Tanner 1, as seen in Figures 4 and 5. The two patients are being followed up in the clinic.
References
- Parent AS, Teilmann G, Juul A, Skakkebaek NE, Toppari J, et al. (2003) The timing of normal puberty and the age limits of sexual precocity: Variations around the world, secular trends, and changes after migration. Endocr Rev 24: 668-693.
- Nathan MB, Palmert MR (2005) Regulation and disorders of pubertal timing. EndocrinolMetabClin N Am 34: 617-641.
- Rosenfield RL, Cooke WD, Radovick S (2008) Puberty and its disorders in the female, Pediatric Endocrinology. Pennsylvania: Saunders Elsevier, (3rd edn), USA, 530-593.
- Ming-Yung L, Chun-Jung J, Chang-Hsien L, Hueng-Chuen F, Mu-Ling H, et al. (2002) Central precocious puberty in a child with the suprasellar arachnoid cyst. J Med Sci 22: 127-130.
- Muir A (2006) Precocious puberty. Pediatr Rev 27: 373-381.
- Hashemipour M, Moaddab MH, Nazem M, Mahzouni P, Salek M(2010) Granulosa cell tumor in a six-year-old girl presented as precocious puberty. J Res Med Sci 15: 240-242.
- Chan LF, Storr HL, Scheimberg I, Perry LA, Banerjee K, et al. (2004) Pseudo-precocious puberty caused by a juvenile granulosa cell tumour secreting androstenedione, inhibin and insulin-like growth factor-I. PediatrEndocrinolMetab 17: 679-684.
- Schumer ST, Cannistra SA(2003) Granulosa cell tumor of the ovary. J ClinOncol 21: 1180-1189.
- Starzyk J, Kwiatkowski S, Urbanowicz W, Starzyk B, Harasiewicz M, et al. (2003) Suprasellararachnoidal cyst as a cause of precocious puberty-Report of three patients and literature overview. J PediatrEndocrinolMetab 16: 447-455.
- Krawchenko J, Collins GH (1979) Pathology of an arachnoid cyst-case report. J Neurosurg 50: 224-228.
- Jamieson S, Fuller PJ(2012) Molecular pathogenesis of granulosa cell tumors of the ovary. Endocr Rev 33: 109-144.
- Akpomuvie OB (2014) The perception of illness in traditional Africa and the development of traditional medical practice. Int J of Nurs 1: 51-59.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences