Neoplasm of the Salivary Glands: A Rare Case Report
Niema Benkhraba
Department of ENT, Ibn Sina University Hospital, Rabat, Morocco
Published Date: 2024-02-22DOI10.36648/2471-8041.10.1.353
Niema Benkhraba1,3*, Zainab Benyahia1,3, Razika Bencheikh2,3, Mohamed Anas Benbouzid2,3, Abdelilah Oujilal2,3 and Leila Essakalli Houssyn2,3
1Department of ENT, Ibn Sina University Hospital, Rabat, Morocco
2Department of Otolaryngology, Head and Neck Surgery, Ibn Sina University Hospital, Rabat, Morocco
3Department of Medicine and Pharmacy of Rabat, Mohamed V University, Rabat, Morocco
- *Corresponding Author:
- Niema Benkhraba
Department of ENT,
Ibn Sina University Hospital, Rabat,
Morocco,
E-mail: niemabenkhraba@gmail.com
Received date: January 23, 2024, Manuscript No. IPMCRS-24-18575; Editor assigned date: January 25, 2024, PreQC No. IPMCRS-24-18575 (PQ); Reviewed date: February 08, 2024, QC No. IPMCRS-24-18575; Revised date: February 15, 2024, Manuscript No. IPMCRS-24-18575 (R); Published date: February 22, 2024, DOI: 10.36648/2471-8041.10.1.353
Citation: Benkhraba N, Benyahia Z, Bencheikh R, Benbouzid MA, Oujilal A, et al. (2024) Neoplasm of the Salivary Glands: A Rare Case Report. Med Case Rep Vol.10 No.01: 353.
Abstract
Myoepithelioma is a benign neoplasm of the salivary glands, which was first described in 1943 by Sheldon. It occurs most commonly between the age of 30 and 50 years. Because of its aggressive nature, in 1991, the World Health Organization (WHO) classified it as a distinct entity. Clinically, myoepitheliomas are present as slow-growing, painless, firm submucosal masses. Four cellular components have been described based on the histopathologic features: spindle cells, plasmacytoid or hyaline cells, epithelioid cells, and clear cells. Because of the varying characteristics, myoepitheliomas present a diagnostic challenge. We present a case of plasmacytoid myoepithelioma arising from the hard palate in a male patient of 64 years of age.
Keywords
Salivary glands neoplasms; Myoepithelioma; Hard palate
Introduction
Myoepitheliomas are benign salivary gland neoplasms consisting entirely or predominantly of cells with myoepithelial phenotype [1,2]. They represent approximately 1.5% of all salivary glands tumors [3] and usually involve the parotid gland or the minor salivary glands of the palate [1-4]. They show no age or gender predilection, but they are more common in middle-aged persons [1-4]. They present as asymptomatic, slowly growing and well-circumscribed tumors of normal color that may be soft to hard on palpation [2-4], and are not associated with neurological symptoms [3,4].
Microscopically, one or all types of neoplastic myoepithelial cells, i.e. spindle, plasmacytoid (hyaline), epithelioid, clear, polygonal, basaloid or oncocytic, may be seen, arranged in solid, myxoid, reticular, microcystic or cribiform growth patterns [1,3,5]. The preponderant cell type defines the tumor’s subtype, although neither cell type nor growth pattern correlate with the clinical presentation or biologic behavior of the lesion [1]. The spindle cells subtype is more common in the parotid gland and the plasmacytoid in the minor salivary glands of the palate [2]. Whether myoepithelioma is a distinct entity or a variant of pleomorphic adenoma with a preponderance of cells with myoepithelial phenotype is disputable.
The aim of this article is to gather up-to-date datas about epidemiological, clinical and histological features of myoeptihelioma, illustrated by a case report with emphasis on diagnostic and therapeutic approach.
Case Report
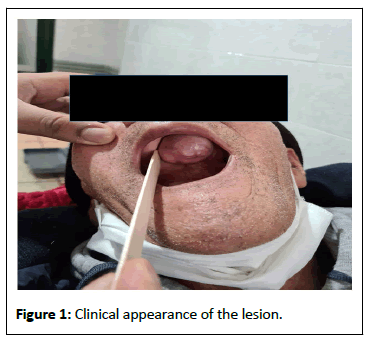
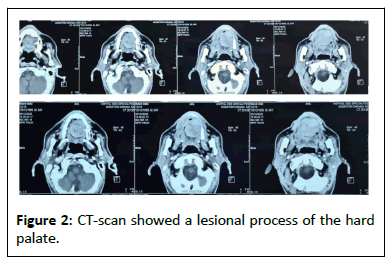
This is a 64-year-old diabetic patient, followed for pulmonary lesions resulting from tuberculosis. Who presented a tumor on the hard palatal that had gradually enlarged during the last few months (Figure 1). Oral examination revealed a round, wellcircumscribed mass covered by normal mucosa on the posterior hard palate. It measured approximately 4 × 3 × 3 cm and was non-tender on palpation. There was no regional lymphadenopathy. The CT-scan showed a lesion process of the hard palate, hypodense, of tissular density, oval, well limited, with regular contours, slightly enhanced after injection of the contrast product and measuring: 40 × 34 × 29 mm (AP × L × H). Topographically: It lyses the palatine and alveolar processes of the maxillary bone on the left with cortical break-in and bulge in the left maxillary sinus. An incisional biopsy was done that rendered the diagnosis of myoepithelioma. Consequently, total excision of the tumor under general anesthesia was performed. Postsurgical healing was uneventful and no recurrence has been recorded 14 months after treatment (Figure 2).
Results and Discussion
Accounting for about 1.5% of all salivary gland tumors and 5.7% of all benign minor salivary gland tumors. Incidence is the same in males and females, ranging from 9-85 years old, mostly during the third decade [6]. No risk factors have been clearly identified.
Although myoepithelioma might occur in any tissue with a secretory function (major and minor salivary glands, sweat glands, lacrimal glands, prostate, breast, nasopharynx, lungs, retroperitoneal region, skin and soft tissue) [7] they preferentially develop in the parotid gland (40%) and in minor salivary glands (21%), especially in the hard and soft palate (40% of reported cases) [6]. Those found in minor glands occur in slightly younger individuals, in compare with other sites [8]. Myoepitheliomas display non-specific, variable, clinical features, like other more frequent lesions such as pleomorphic adenoma, which can easily lead to a misdiagnosis. Biopsy is frequently nonspecific and fine-needle aspiration cytology possibly misleading. Indeed, depending on the sampling region, myoepithelioma can exhibit the same characteristics as other salivary glands tumors. Architectural examination combined with immunochemical profiles is thus crucial for thorough diagnosis.
Clinically, benign myoepithelioma is usually described as an asymptomatic, insidious mass that slowly enlarges over a period ranging from several months to years, rarely ulcerated (mostly resulting from a chronic local injury). The tumor is wellcircumscribed, firm but not hard, and its surface is lobulated without any associated nervous alterations or lymphadenopathy. Originally described as 1–5 cm swellings [9], tumors rarely exceed 3 cm in diameter at the time of the diagnosis. The surgical specimens of myoepitheliomas have a solid, yellow or gray appearance, with glistening cut surface. Apart from the mild pain, the observation in this cases conformed with this description.
Data available about CT and MRI imaging of myoepithelioma are limited. A few recent retrospective studies looked after imaging characteristics of benign and malignant parotid myoepithelioma.
Early findings about benign myoepitheliomas displayed isolated, unilocular (71%) or multilocular (22.2%), mostly round, with smooth contours and weel-defined margins tumors. Capsule are generally discernable on T2-Weighted and contrast enhanced T1-Weighted imaging. Tumors display homogeneous MRI signal intensities, with a T2-Weighted hypersignal [10]. Enhanced CT imaging may display enhancing nodules and nonenhencings areas of linear bands or with cystic configuration [11].
Myoepithelioma exhibits the variable nature of myoepithelial cells through the great variability of its structure and components from an area to another and from a tumor to another. Accordingly, biopsy is frequently non-specific and fineneedle aspiration cytology possibly misleading [12]. Indeed, depending on the sampling region, myoepithelioma can exhibit the same characteristics as other salivary glands tumors. A complete resection of the tumor is necessary for appropriate histological examination.
Cells types described in myoepithelioma include spindle, plasmacytoid (or hyaline), epithelioid, clear-cell and oncocytic types. Spindle and plasmacytoid are the most reported variants. Plasmacytoid type is frequent in minor salivary glands, whereas spindle cells are often reported in the parotid [7,9] Another recently described entity, called “mucinous myoepithelioma” displays intracellular mucin material [13]. Clear cells type can undergo cystic changes [14]. One type or mixture of different cell-type can be found in the same tumor. Plasmacytoid myoepithelioma should also be distinguished from rhabdomyoma and oncocytoma, the latter displaying granular cytoplasm on histological examination.
Other differential diagnoses of myoepitheliomas include hemangiomas, neurinomas, metastatic tumors, malignant tumors, solitary fibrous tumor, lymphoma, leiomyoma, hemangiopericytoma, tumors of the nerve sheath, leiomyosarcoma, fibrous histiocytoma, and few inflammatory diseases [15]. Histology plays an important role in confirmation of the diagnosis [16].
Recommended surgical management of myoepithelioma is a complete surgical excision with a safety margin of uninvolved tissue [7]. Although myoepithelioma is reported to have more aggressive behavior to pleomorphic adenoma [17]. Recurrence is associated with positive margins and this may occur in myoepitheliomas of minor salivary glands, especially of the palate, where tumor encapsulation is uncommon [1]. Recurrence rate of plasmacytoid myoepitheliomas of the palate is estimated to 15%-18% [18]. Malignant transformation may ensue, particularly in the spindle cell variant [19].
Conclusion
Plasmacytoid myoepithelioma, a rare tumor of salivary glands, is a painless and slow-growing lesion that most commonly occurs in the minor salivary glands. Histopathologic findings are necessary for a definitive diagnosis. Considering myoepithelioma as one of the differential diagnoses is important while dealing with any case of palatal swelling.
References
- Gnepp DR (2001) Diagnostic surgical pathology of the head and neck. (2nd ed) Philadelphia Saunders, London, UK.
- Hunt KT, Stevens MR, Abdelsayed RA, Nguyen CT (2011) Benign myoepithelioma of floor of mouth with mandibular involvement: A case report and literature review. J Oral Maxillofac Surg 69: 3001–5.
[Crossref], [Google Scholar], [Indexed]
- Ellis AL, Auclair PL (1996) Benign epithelial neoplasms. (3rd ed), Washington, USA.
- Barnes L, Appel BN, Perez H, El-Attar AM (1985) Myoepithelioma of the head and neck: Case report and review. J Surg Oncol 28: 21–8.
[Crossref], [Google Scholar], [Indexed]
- Savera AT, Zarbo RJ (2004) Defining the role of myoepithelium in salivary gland neoplasia. Adv Anat Pathol 11: 69-85.
[Crossref], [Google Scholar], [Indexed]
- EI-Naggar AK, Chan JKCG, Randis JR, Takata T, Slootweg PJ (2017) WHO Classification of head and neck tumours. (4th edition) IACR Publication, Lyon, France.
- Nair BJ, Vivek V, Sivakumar TT, Joseph AP, Varun BR, et al. (2014) Clear cell myoepithelioma of palate with emphasis on clinical and histological differential diagnosis. Clin Pract 4: 628.
[Crossref], [Google Scholar], [Indexed]
- Eveson JW, Auclair P, Gnepp DR, El-Naggar AK (2005) Tumours of the salivary glands. Introduction. In: Barnes L, Eveson JW, Reichart P, Sidransky D. World Health Organization classification of tumors. Pathology and genetics of head and neck tumors, IARC Press, Lyon, France.
- Simpson RH, Jones H, Beasley P (1995) Benign myoepithelioma of the salivary glands: A true entity? Histopathology 27: 1-9.
[Crossref], [Google Scholar], [Indexed]
- Ding J, Wang W, Peng W, Zhou X, Chen T (2016) MRI and CT imaging characteristics of myoepithelioma of the parotid gland. Acta Radiol 57: 837-843.
[Crossref], [Google Scholar], [Indexed]
- Wang S, Shi H, Wang L, Yu Q (2008) Myoepithelioma of the parotid gland: CT imaging findings. AJNR Am J Neuroradiol 29: 1372-1375.
[Crossref], [Google Scholar], [Indexed]
- Mejia-Hernandez IJ, Valdez AC, León-Trenado DD, Luna-Ortíz K (2013) Malignant myoepithelioma of the soft palate. Auris Nasus Larynx 40: 231-234.
[Crossref], [Google Scholar], [Indexed]
- Gnepp DR (2013) Mucinous myoepithelioma: A recently described new myoepithelioma variant. Head Neck Pathol 7: S85–S89.
[Crossref], [Google Scholar], [Indexed]
- Agarwal AK, Sethi A, Chopra S, Sareen D (2007) Clear cell myoepithelioma of the hard palate. Internet J Head Neck Surg 2.
[Crossref], [Google Scholar]
- Yadav AK, Nadarajah J, Chandrashekhara SH, Tambade VD, Acharya S (2013) Myoepithelioma of the soft palate: A case report. Case Rep Otolaryngol 2013: 642806.
[Crossref], [Google Scholar], [Indexed]
- Kim HS, Lee WM, Choi SM (2007) Myoepitheliomas of the soft palate: Helical CT findings in two patients. Korean J Radiol 8: 552-5.
[Crossref], [Google Scholar], [Indexed]
- Yang S, Li L, Zeng M, Zhu X, Zhang J, et al. (2010) Myoepithelial carcinoma of intraoral minor salivary glands: A clinicopathological study of 7 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110: 85-93.
[Crossref], [Google Scholar], [Indexed]
- Zormpa MT, Sarigelou AS, Eleftheriou AN, Assimaki AS, Kolokotronis AE (2011) Plasmacytoid myoepithelioma of the palate: Case report. Head Neck Pathol 5: 154-8.
[Crossref], [Google Scholar], [Indexed]
- Alós L, Cardesa A, Bombi JA, Mallofre C, Cuchi A, et al. (1996) Myoepithelial tumors of salivary glands: A clinicopathologic, immunohistochemical, ultrastructural, and flow-cytometric study. Semin Diagn Pathol 13: 138-47.
[Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences