Modified Accelerated Infusion Thrombolysis and Heparinization Approach in Acute Ischemic Stroke Reocclussion
Rusly Rusly
Department of Accident and Emergency, Murni Teguh Memorial Hospital, Medan, North Sumatera, Indonesia
Published Date: 2022-05-30DOI10.36648/2471-8041.8.5.227
Rusly Rusly*
Department of Accident and Emergency, Murni Teguh Memorial Hospital, Medan, North Sumatera, Indonesia
*Corresponding author: Rusly Rusly, Department of Accident and Emergency, Murni Teguh Memorial Hospital, Medan, North Sumatera, Indonesia, E-mail: dr.rusly@gmail.com
Received date: May 1, 2022, Manuscript No. IPMCRS-22-13106; Editor Assigned date: May 3, 2022, PreQC No. IPMCRS-22-13106 (PQ); Reviewed date: May 18, 2022, QC No. IPMCRS-22-13106; Revised date: May 24, 2022, Manuscript No. IPMCRS-22-13106(R); Published date: May 30, 2022, DOI: 10.36648/2471-8041.8.5.227
Citation: Rusly R (2022) Modified Accelerated Infusion Thrombolysis and Heparinization Approach in Acute Ischemic Stroke Reocclussion. Med Case Rep Vol.8 No.5:227
Abstract
Acute stroke ischemic has a sudden onset. A 48 years old male was admitted to ER with estimated 30 minutes-60 minutes onset acute ischemic stroke. Firstly, he received a standardized dosage of alteplase. Unfortunately, reocclusion occurred after thrombolysis finished. He received another thrombolysis and heparinization without any side effects from thrombolysis during hospitalization.
Keywords: Alteplase; Heparinization; Thrombolysis; Acute ischemic stroke; Reocclussion
Introduction
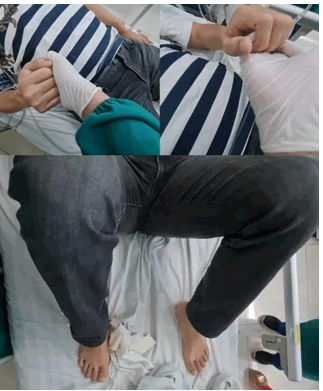
A 48 years old male was responded by EMT on 16th November 2021 with an estimated 30 minutes-60 minutes loss of consciousness history. EMT arrived with the patient in the recovery position. The patient could not speak nor move his right arm and leg. No history of seizure, vomiting or headache before this.
Ample: No allergic, no medication, no history of chronic disease(s), last meal within 2 hours before the loss of consciousness, he has a history of domestic travelling 2 days prior.
The primary survey of this patient was clear. Despite he has aphasia, he was fully responsive and cooperative.
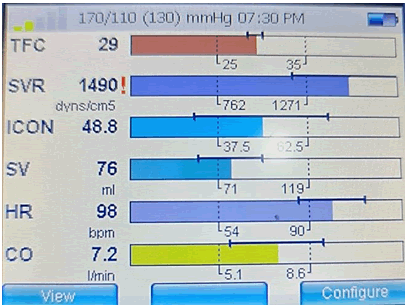
His vital signs presented with blood pressure 170/110 mmHg (left arm), heart rate 95 bpm sinus, respiratory rate 18 times per minute, SpO2 99% on room air and blood glucose result was 139 mg/dL. From the physical examination, he presented with aphasia and an absence of motor function in his right limbs and face.
He was treated with 30 degrees of head elevation, 2 litres of oxygen despite SpO2 result and maintenance intravenous fluid drips.
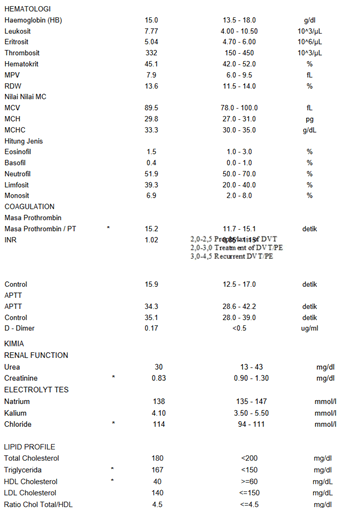
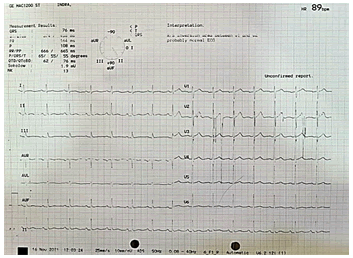
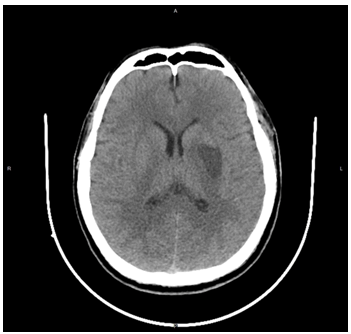
Arriving in the emergency room, his blood was withdrawn for complete blood count, renal function test, coagulation profile (APTT, PT, D-Dimer), Lipid profile and covid19 screening test. He was also sent immediately to the radiology department, running a non-contrast routine brain CT scan examination. Besides vital signs and 7 leads ECG monitor, he was also monitored by an electrical cardiometer which show his hemodynamic was optimal.
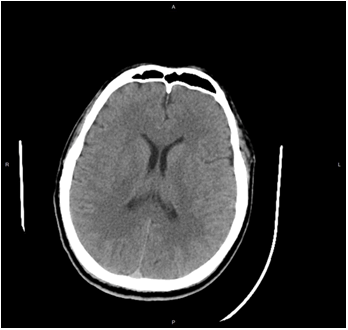
As the CT scan didn't show any bleeding, he was planned to receive thrombolysis therapy. Informed consent was obtained while preparing thrombolysis.
In the first plan, he was planned to receive a standardized dosage of alteplase for thrombolysis. Using his estimated body weight and last bodyweight measurement history [1]. He received a total of 72 mg alteplase (0.9 mg/kg for 80 kg estimated body weight) 10% of the total dosage was administrated intravenously within 1 minute while 90% of the total dosage was dripped intravenously for 60 minutes. Thrombolysis was started estimated 60 minutes-90 minutes onset.
Thirty minutes after starting thrombolysis, his language and motor function had improved. He had no deterioration or side effects after thrombolysis. However, reocclussion was suspected as aphasia and loss of motor function at 68th minutes. He had immediately received another 28 mg of alteplase infusion dripped for 2 hours. To prevent another reocclussion, he also received 15 i.u./kg/hour heparin for 3 hours. While 6 hours receiving thrombolysis continued with heparin, aphasia still occurs while motor function fully recovers and no side effect within the treatment.
He was transferred to ICU for further observation. Beside his slow environment recognition, he shows no other motor function deterioration or side effects of thrombolysis while in ICU, he was transferred to the ward and discharged by the third day of hospitalization.
The CT scan shows infarction around ventral stream which explain his slow response. Without intracranial hemorrhage or bleeding sign occurs after 3 days of hospitalization.
Discussion
Only intravenous thrombolysis with recombinant tissue Plasminogen Activator (rtPA) has proven to be effective for the treatment of ischemic stroke within 4.5 hours of the onset of symptoms. IV rtPA for recanalizing has a 30% to 40% success rate while reocclusion occurs in ≈20% to 30% of patients. More than half of ischemic stroke patients who received rtPA remain disabled at 3 months. Intravenous thrombolysis alone remained recommended by many guidelines [2-4].
However, in this case, IV rtPA alone was almost ineffective in treating acute ischemic stroke. I was trying to treat the patient by modifying accelerated infusion thrombolysis used in treating acute myocardial ischemic. In this modified thrombolysis, I started the standardized alteplase dosage, 10% of 0.9 mg/kg of alteplase being bolus intravenously and continued 90% was being dripped intravenously. As the maximum recommended thrombolysis dosage for acute ischemic stroke is 90 mg of alteplase, so the rest of alteplase was dripped intravenously for 2 hours. I also give anticoagulation after thrombolysis due to the previous reocclusion.
In my opinion, thrombolysis using the recommended dosage alteplase to this patient was almost successful. Suspected reocclussion was happened 8 minutes after thrombolysis. So the patient was planned to have another thrombolysis drip. To prevent another reocclusion, I consider heparin following thrombolysis instead of using low molecular heparin as anticoagulation due to its shorter half-life. In case bleeding occurs, heparin can be stopped as early as possible. Thrombolysis in this patient was started within 60 minutes -90 minutes onset and his NIHSS was 18 points at admission. He was at higher risk of reocclusion according to the predictor reocclussion study [5]. Despite fully motor function recovered, environment recognition still occurs in this patient. However, he also doesn't show any intracranial hemorrhage from combining anticoagulation following thrombolysis. These are supported by the CT scan prior to discharge [6].
Conclusion
Recommendation against antithrombic agents in thrombolysis for acute ischemic stroke needs to be reconsidered because improving IV rtPA is still a challenge today. Option for shorter half time anticoagulation, early anticoagulation initiation for high-risk reocclussion patients after rtPA and shorter duration anticoagulation drip might prevent bleeding while improving reocclusion after thrombolysis for acute ischemic stroke.
References
- Graves A, VerHage A, Richlik B, Makic MB (2013) Estimated versus actual weight when dosing rt-PA in acute ischemic stroke: Is there a difference? J Neurosci Nurs 45: 180-5.
[Cross Ref], [Google Scholar], [Indexed]
- Derex L, Chloe P, Norbert N (2018) Combining intravenous thrombolysis and antithrombotic agents in stroke: An update. J Am Heart Assoc 7: e007454 .
[Cross Ref], [Google Scholar], [Indexed]
- Pooja K, Marie Luise M (2013) Combining antithrombotic and fibrinolytic agents: can it be done? Stroke 44: 1489-91.
[Cross Ref], [Google Scholar], [Indexed]
- Harris S, Aliah A, Rasyid A, Kurniawan M, Mesiano T, et al. (2013) Protokol tata laksana trombolisis stroke iskemik akut. Neurona 1: 1-6.
[Cross Ref], [Google Scholar], [Indexed]
- Rubiera M, Sabin JA, Ribo M, Montaner J, Santamarina E, et al. (2005) Predictors of early arterial reocclusion after tissue plasminogen activator-induced recanalization in acute ischemic stroke. Stroke 36: 1452-6.
[Cross Ref], [Google Scholar], [Indexed]
- Ohman EM, Califf RM, Topol EJ, Candela R, Abbottsmith C, et al. (1990) Consequences of reocclusion after successful reperfusion therapy in acute myocardial infarction. TAMI study group. Circulation 82: 781-91.
[Cross Ref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences