Mis-C in A Very Preterm Elbw Neonate Due To In Utero Maternal Sars-Cov-2 Igg Exposure
Atraya Samanta*1, Indranil Karmakar1, Ruchi Golash2, Arnab Haldar3
Atraya Samanta*1, Indranil Karmakar1, Ruchi Golash2, Arnab Haldar3
1Department of MBBS DNB Resident Calcutta Medical Research Institute
2Department of MBBS MRCPCH Calcutta Medical Research Institute
3Department of MBBS DCH DNB Resident Calcutta Medical Research Institute
- *Corresponding Author:
- Samanta A
Department of MBBS DNB Resident Calcutta Medical Research Institute, India
Tel: 083488022827
E-mail: atrayasamantajrb10@gmail.com
Received Date: July 31, 2021; Accepted Date: October 14, 2021; Published Date: October 14, 2021
Citation: Samanta A (2021) Mis-C in A Very Preterm Elbw Neonate Due To In Utero Maternal Sars-Cov-2 Igg Exposure, Med Case Rep, Vol: 8 No: 1.
Introduction
Cases of multi-systemic inflammatory syndrome in child (MIS-C) due to SARS- CoV-2 antibodies are increasing since this pandemic continues unabated. Although most reported cases were in the age group between 5 to 13 years and median age of children was 9 years [1], MIS-C in neonates is still very rare as a diagnosis. Though pregnant women are at a higher risk of contracting the infection but vertical transmission of SARS-CoV-2 infection occurs in minority of cases during third trimester of pregnancy [2] [3]. various case studies have demonstrated the presence of SARS-CoV-2 IgG in cord blood and placental transmission of maternal SARS-CoV-2 IgG from mother to fetus in cases of both asymptomatic and symptomatic infections during pregnancy [4] [5]. In this case report, we are presenting a very preterm ELBW neonate who suffered MIS-C due to maternal SARS-CoV-2 IgG exposure.
Case Report
A 29 weeks 1 day old, baby girl weighing 990 grams was delivered via lower uterine caesarean section (LUCS) at our institute to a covid-19 RTPCR negative primigravida mother with a history of preterm premature rupture of membranes. Antenatal sonography of mother and fetus did not reveal any abnormalities. Baby had cried immidiately after birth, APGAR score was 71 & 95. However, baby developed respiratory distress soon after birth, requiring positive pressure ventilation and later put on mechanical ventilator. As there was hypotension and tachycardia, inotropic support was provided. Blood gas analysis revealed respiratory alkalosis with metabolic acidosis.
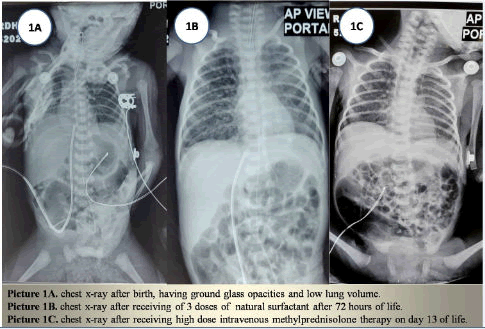
Chest X-ray (Picture.1A) done after birth, showed low lung volume along with ground glass opacities bilaterally. 1st dose of natural surfactant was administered. However, even after receiving 3 doses of surfactants, skiagram (Picture.1B) revealed no significant improvement.
Echocardiography revealed persistent pulmonary hypertension in neonate (PPHN), small patent ductus arteriosus (PDA) measuring 2-3 cm with wall hypokinesia. Sildenafil infusion and intravenous paracetamol was started.
Although initial sepsis screen was negative, considering the deteriorating condition of the baby, late onset sepsis was suspected. Antibiotics were upgraded to meropenem and tigecycline after sending blood culture.
On day 4 of life blood reports revealed Hb%-11.2 gram/deciLitre, TLC-4400 / milimeter3 (neutrophil-70%, Lymphocyte- 26%), platelet count-3.2 lakhs / microLitre, CRP-0.435 miligram/deciLitre (normal- <0.3), procalcitonin -15.8 nanogram/mililitre, blood culture showed no growth till day 5.
As sepsis screen was negative, nasopharyngeal swab for covid-19 RTPCR was sent and it came negative on two occasions. Considering a possibility of post covid-19 MIS-C, SARS-CoV-2 IgG was sent and it was reactive with a titre of 2.32 (Reference range- 0 to 1). Inflammatory markers’ study revealed, Ferritin-372.5 nanogram/miliLitre (ng/ml), D-dimer- 6074 nanogram Fibrinogen Equivalent Unit / miliLitre (ngFEU/ml), pro-B type Natriuretic Peptide (pro-BNP)- 25203 microgram / miliLitre ( mcg/ml), Lactate Dehydrogenase (LDH) -479 Units / Litre (U/L), Interleukin-6 - 71.12 picogram / miliLitre (pg/ml).
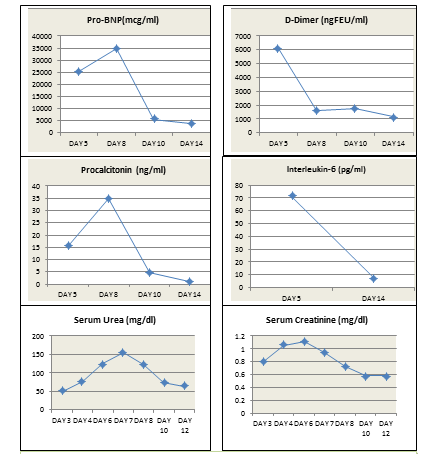
Hemoglobin was 9.2 gram/deciliter (gm/dl), hence, red blood cells were transfused. As urea, creatinine levels (Figure.2) were getting higher, intravenous fluid was increased and amino acid infusion was restricted to 2 gram/kilogram via total parenteral nutrition solution. Low dose intravenous corticosteroid was started on day 5 of life as well as Intravenous Immunoglobulin G (IVIgG) @ 2 gram/kilogram slow infusion. After 48 hours procalcitonin and proBNP levels had increased and the baby was still in shock with deteriorating arterial blood gas and serum lactate. Hence, from day 7 of life, intravenous methyl prednisolone @ 10 miligram / kilogram was started for 3 days which was then gradually tapered off over next 14 days. Gradually after 48 hours there was a steady improvement in blood gas, serum lactate and values of proBNP, procalcitonin, interleukin-6, D-dimer (Figure.1).
Figure 1: Inflammatory markers have shown no response after low dose corticosteroid administration on day 5. Gradual decline is seen in these values after starting of high dose corticosteroids from day 8. Trends of the values of urea and creatinine showing uptrend during first 7 days of life, followed by gradual decline from day 8 onwards.
Although, the mother was neither vaccinated, nor had history of SARS-CoV-2 infection, mother’s SARS-CoV-2 IgG report came positive with a titre of 4.32 (Reference range- 0 to1).
Baby was extubated and weaned off from mechanical ventilator to nasal continuous positive airway pressure on day 12 of life. She needed positive pressure support till day 16 of life followed by humidified oxygen via nasal prong. Chest x-ray (Picture.1C) showed improvement than previous ones. Repeat echocardiography revealed, regression of PAH, closed PDA and good biventricular function. Sildenafil infusion was stopped. Intravenous paracetamol was stopped after total 28 doses. Baby had developed hypertension (mean blood pressure >70 mm hg) which had lasted for 48 hours and which was treated with intravenous labetalol and furosemide infusion. Renovascular structural anomaly was ruled out by ultrasound.
Trophic feeding was started via nasogastric tube and gradually increased.
Baby is currently at our inpatient care, weighing 1.215 kilograms. She is maintaining saturation at room air, blood pressure has stabilised, vitals are normalised, tolerating feed orally on demand.
Discussion
We have found two case reports of multi-systemic inflammatory syndrome in term neonates temporally associated with maternal SARS-CoV-2 IgG exposure[6][7]. No case has been reported till date of MIS-C in a very preterm ELBW neonate. In our case, there was a diagnostic dilemma for starting steroids as many features of severe sepsis can mimic MIS-C in a neonate. As there are no specific guidelines available on dosage of corticosteroids and IVIgG in preterm neonates with MIS-C, first we opted for low dose corticosteroid. But, when there was no response, we have decided to go for high dose corticosteroid therapy.
Dustin D. Flannery, Sigrid Gouma, Miren B. Dhudasia et al had concluded in a cohort study that, maternal IgG antibodies to SARS-CoV-2 were transferred across the placenta after asymptomatic as well as symptomatic infection during pregnancy[8]. So, in utero SARS-CoV-2 IgG exposure is the likely cause of this hyper inflammatory response in our neonate.As the mother was neither vaccinated, nor had history of symptomatic covid-19 infection , it can be assumed that she had suffered an asymptomatic covid-19 infection leading to production of SARS- CoV-2 IgG in her body, which was later transferred to the fetus.
Though we could not document umbilical cord interleukin-6 level after birth, still, fetal inflammatory response syndrome (FIRS)[9] also should considered in cases of sudden preterm premature rupture of membrane (PPROM) in an uneventful pregnancy with normal antenatal ultrasound. A study conducted by Mariko Nakahara, Shunji Goto and others showed 66 patients were positive for FIRS among 158 cases of PPROM [10]. FIRS can be defined as elevated level of interleukin-6 (>11picogram/miliLitre) at the umbilical cord blood[11]. Estimation of cord blood Interleukin-6 levels at birth and serially for next few days will help in early detection of MIS-C in preterm neonates whose mothers have a history of preterm premature rupture of membranes.
A preterm neonate with respiratory distress syndrome, not responding to surfactant therapy , persistent pulmonary hypertension and shock after birth with no significant structural cardiovascular pathology, with a negative sepsis screen, must be evaluated neonatal MIS-C where timely administration high dose corticosteroids can be life saving.
References
- Kotlyar AM, Grechukhina O, Chen A, et al. Vertical transmission of coronavirus disease 2019: a systematic review and meta-analysis.Am J Obstet Gynecol. 2021;224(1):35-53.e3.
- Zaigham, M,Holmberg, A,Karlberg, ML,Lindsjö, OK,Jokubkiene, L,Sandblom, J,Strand, AS,Andersson, O,Hansson, SR,Nord, DG,Tannenberg, P.Intrauterine vertical SARS-CoV-2 infection: a case confirming transplacental transmission followed by divergence of the viral genome.BJOG2021
- Flannery DD, Gouma S, Dhudasia MB, et al. Assessment of Maternal and Neonatal Cord Blood SARS-CoV-2 Antibodies and Placental Transfer Ratios.JAMA Pediatr.2021; 175(6):594–600.
- Fenizia, C., Biasin, M., Cetin, I.et al.Analysis of SARS-CoV-2 vertical transmission during pregnancy.Nat Commun11,5128 (2020).
- Multisystem inflammatory syndrome in a neonate, temporally associated with prenatal exposure to SARS-CoV-2: a case report Kappanayil, Mahesh et al.The Lancet Child & Adolescent Health. 5(4), 304 – 308
- Khaund Borkotoky R, Banerjee Barua P, Paul SP, Heaton PA. COVID-19-related potential multisystem inflammatory syndrome in childhood in a neonate presenting as persistent pulmonary hypertension of the newborn.Pediatr Infect Dis J.2021
- Flannery DD, Gouma S, Dhudasia MB, et al. Assessment of Maternal and Neonatal Cord Blood SARS-CoV-2 Antibodies and Placental Transfer Ratios. JAMA Pediatr.2021;175(6):594–600.
- FetalInflammatoryResponseSyndromeAssociatedWithMaternalSARSCoV2Infection. L.McCarty,MeganTucker,GeneLee,VishalPandey PediatricsApr 2021,147(4)e2020010132
- Nakahara, M., Goto, S., Kato, E., Nojiri, S., Itakura, A. and Takeda, S. (2020), Maternal risk score for the prediction of fetal inflammatory response syndrome after preterm premature rupture of membranes. J. Obstet. Gynaecol. Res., 46: 2019-2026.
- Wolfsberger CH, Bruckner M, Baik-Schneditz N, Schwaberger B, Mileder LP, Avian A, Urlesberger B and Pichler G (2020) Fetal Inflammatory Response Syndrome and Cerebral Oxygenation During Immediate Postnatal Transition in Preterm Neonates.Front. Pediatr.8:401.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences