Leiomyosarcoma of the Recto-Sigmoid Junction Prolapsing out of the Anus: A Case Report
Ginimal Bandaralage Kavinda Deshapriya Bandara
Department of Surgical Unit, National Hospital of Sri Lanka, Colombo, Sri Lanka
Published Date: 2024-02-05DOI10.36648/2471-8041.10.1.352
Ginimal Bandaralage Kavinda Deshapriya Bandara*, Arulprashanth Arulanantham and Merrenna Ishan Malith De Zoysa
Department of Surgical Unit, National Hospital of Sri Lanka, Colombo, Sri Lanka
- *Corresponding Author:
- Ginimal Bandaralage Kavinda Deshapriya Bandara
Department of Surgical Unit, National Hospital of Sri Lanka, Colombo,
Sri Lanka,
E-mail: gbkavindadb@gmail.com
Received date: January 04, 2024, Manuscript No. IPMCRS-24-18535; Editor assigned date: January 06, 2024, PreQC No. IPMCRS-24-18535 (PQ); Reviewed date: January 22, 2024, QC No. IPMCRS-24-18535; Revised date: January 29, 2024, Manuscript No. IPMCRS-24-18535 (R); Published date: February 05, 2024, DOI: 10.36648/2471-8041.10.1.352
Citation: Bandara GBKD, Arulanantham A, De Zoysa MIM (2023) Leiomyosarcoma of the Recto-Sigmoid Junction Prolapsing out of the Anus: A Case Report. Med Case Rep Vol.10 No.01: 352.
Abstract
Leiomyosarcoma is a rare mesenchymal neoplasm in the gastrointestinal tract which has similar microscopic and macroscopic characteristics to GISTs. In this article we present an unusual presentation of this rare tumour which posed us a management challenge. A 73-year-old male presented with bleeding per rectum and was found to have an obstructing growth at recto-sigmoid. While awaiting tissue diagnosis, this tumour prolapsed out of the anus with bleeding. To control bleeding and to relieve pain trans-anal excision of the tumour was done. Subsequently the patient underwent laparoscopic anterior resection for a recurrent tumour. Histology and immunohistochemistry confirmed the diagnosis of a leiomyosarcoma. Leiomyosarcomas carry a poor prognosis and should be always differentiated from GISTs using immunohistochemistry. Radical surgery is the main stay of management.
Keywords
Leiomyosarcoma; Prolapse; GIST
Introduction
Leiomyosarcoma is a mesenchymal neoplasm which can be found mainly in the uterus, retroperitoneum and rarely in the gastrointestinal tract [1-3]. Leiomyosarcoma share similar macroscopic and microscopic characteristics with Gastrointestinal Stromal Tumours (GIST). Accurate differentiation of the two is important in their management and prognosis which became possible only after the discovery of their immune-histochemical identities. Since then, diagnosing a primary leiomyosarcoma in the gastrointestinal tract became so rare to the extent that there is limited data on demography, clinical features and gross features of these tumours [1,4,5].
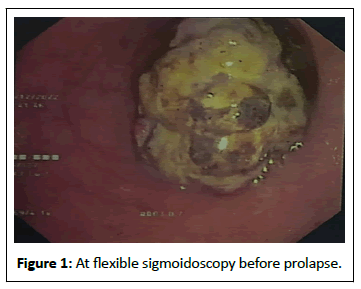
Bleeding per rectum and alteration of bowel habits are the commonest presentations of tumours of the le t sided colon and rectum [6]. Rare cases of colorectal adenocarcinomas presenting with rectal prolapse has been reported in literature [6-8]. There have been some case reports of patients with polyps and polyposis syndromes presenting with a prolapsed polyp [9-11]. In this background where tumour prolapse is an atypical presentation of cancer, a patient with a recto-sigmoid leiomyosarcoma causing tumour prolapse is an extreme rarity (Figure 1).
Case Presentation
A 73-year-old male patient with hypertension and stage II chronic kidney disease presented with bleeding per rectum and discomfort while passing stools for 3 months.
On examination, he was not pale and the abdominal examination was unremarkable. On digital rectal examination an apex of a mass was felt 5 cm from the anal verge. Flexible sigmoidoscopy showed a malignant looking polypoidal growth at 15 cm from the anal verge. The scope could not be negotiated beyond the lesion. Multiple biopsies were taken and the patient was admitted for further investigations for diagnosis and work up for surgery in suspicion of a rectal carcinoma.
Contrast Enhanced Computed Tomography Scan (CECT) demonstrated a large polypoidal growth almost completely obliterating the rectosigmoid junction with possible infiltration into the serosa. There was no evidence of regional lymphadenopathy or distant metastases.
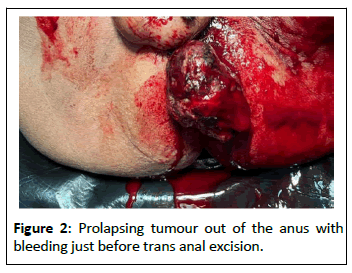
During the ward stay he developed several episodes of per rectal bleeding with his bowel motions. One day when passing stools, he had a severe bout of pain with a significant amount of blood and a mass prolapsing out of the anus. On the first occasion this was manually reduced without much difficulty. On the next day it prolapsed again and could not be reduced manually. As it was painful and the prolapsed mass was bleeding continuously, the patient was taken to theatre for examination under anaesthesia.
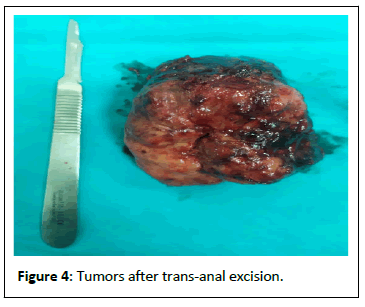
While the patient was in the lithotomy position, we noted a 10 × 10 cm sized mass with bleeding projecting out of the anus (Figure 2). It was connected by a narrow pedicle. Our plan was to divide this mass from the pedicle while ensuring haemostasis. We divided the pedicle using an ultrasonic dissector and by transfixing with 3-0 polyglactin sutures. Subsequent digital rectal examination did not reveal any active bleeding from the divided pedicle. The specimen was sent for histology.
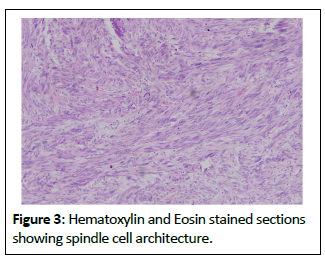
Post-operatively he was asymptomatic and was discharged with a plan to review with histology. The histology reported a leiomyosarcoma with its spindle cell architecture and supportive immunohistochemical studies. With our available resources, Smooth Muscle Actin (SMA), Desmin, S100 and CD34 studies were done. It was found to be SMA and Desmin positive and CD117, S100 and CD34 negative. It was reported independently by two consultant pathologists and final conclusion of a leiomyosarcoma was made. The resection margin was involved by the tumour (Figure 3).
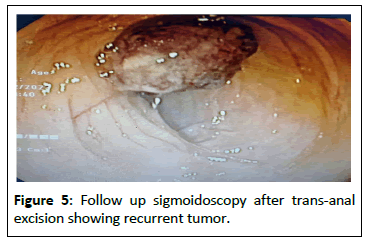
One month after the trans-anal excision, a flexible sigmoidoscopy was performed to see the status of the tumour bed and to plan further management. Sigmoidoscopy revealed a recurrence of the tumour at the recto-sigmoid junction. Following a multi-disciplinary team meeting, the patient was planned for an anterior resection (Figure 4).
After a brief period of prehabilitation, he underwent a laparascopic anterior resection. Post-operative recovery was uneventful and the patient was discharged home on day five following surgery. Histology confirmed the diagnosis of leiomyosarcoma with negative resection margins and two out of four lymph nodes showing tumour deposits. Tumour was of grade 3 under French Federation Nationale des Centers de Lutte Contre le Cancer (FNCLCC) system.
Subsequently the patient was referred to the oncologist for adjuvant therapy. While waiting for chemotherapy the patient developed a myocardial infarction from which he recovered. However, he was deemed unfit for further adjuvant therapy.
Result and Discussion
Cancers arising in the gastro-intestinal tract are mainly epithelial in origin and out of colorectal malignancies commonest is adenocarcinoma [12]. Primary mesenchymal sarcomas are so rare in the gastrointestinal tract out of which commonest is leiomyosarcoma [4]. However, following advances in immunohistochemistry, it was realized that most of the mesenchymal neoplasms previously identified as leiomyosarcomas turned out to be GISTs. Since then, diagnosis of a leiomyosarcoma in the gastrointestinal tract became a rare entity [4,5].
Individual case reports and case series identify abdominal pain, lower gastrointestinal bleeding and abdominal mass as common presentations of colorectal leiomyosarcomas [13-15]. Intestinal obstruction, perforation and acute suppurative peritonitis are rare presentations reported in individual case reports [4,14,15].
Tumour prolapse with or without full thickness rectal prolapse is a rare presentation even for colorectal adenocarcinomas [6-8]. Tumour prolapse percise is almost unheard of except for case reports of prolapsing polyps [10,11]. A clinical note published in Saudi Medical Journal in 2007 reports a rectal GIST presenting with prolapse [16]. Rectal and rectosigmoid carcinomas presenting with full thickness rectal prolapse have been reported. Presence of tumour at the apex of the prolapse in these cases indicate the fact that these tumours might have acted as the lead point for intussusception and subsequent prolapse [6-8].
The novelty of this presentation posed us a management challenge. This painful and bleeding tumour outside the anus needed to be attended to as soon as possible. Given the patient’s age and his comorbidities and fact that we did not have a proper tissue diagnosis at that time, relieving his symptoms with least morbidity was our objective. This trans-anal excision relieved of his symptoms but a definitive management strategy was needed after the tissue diagnosis (Figure 5).
GISTs and leiomyosarcomas are macroscopically and microscopically similar [17]. GISTs originate from the interstitial cells of Cajal and leiomyosarcomas has its origin from smooth muscle cells [1]. Owing to this difference in origin they have distinct immunohistochemical identities and prognosis [1,3-5,17,18].
Leiomyosarcomas carry a poor prognosis by being aggressive tumours with high chance of local recurrence and metastasis, poor overall survival, absence of a targeted therapy and poor response to chemotherapy [1,2,4,18]. In 1998, Hirota et al., discovered the oncogenic role of c-kit mutations in GISTs and it paved way for the place of targeted therapy with tyrosine kinase inhibitors [3,5,17]. Subsequently KIT (CD117), CD34 and DOG1 were identified as immunohistochemical markers with higher sensitivity and specificity in the diagnosis of GISTs. SMA, Desmin and h-caldesmon are immunohistochemical markers which indicate smooth muscle cell origin of leiomyosarcomas and these markers are absent in GISTs [3].
In this patient SMA and Desmin were positive while CD117 and CD34 were negative. S100 is a schwannoma marker protein which was also negative supporting the diagnosis of a leiomyosarcoma.
As the initial resection margin was positive and the subsequent endoscopic examination showed the presence of recurrent tumour, definitive surgery to achieve an oncological resection was warranted. According to the current literature radical resection is the main mode of management. The role and the effectiveness of chemotherapy and radiotherapy in management is still not established [4,17].
Conclusion
Leiomyosarcomas are a rare type of mesenchymal tumours occurring in the gastrointestinal tract which should be differentiated from GISTs. They are aggressive tumours with poor prognosis and surgery remains the mainstay of management.
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
This case report was prepared for publication with the informed written consent of the index patient and relatives. All images were taken and included with consent.
Conflicts of Interests
Non declared.
Funding
Not applicable.
Author’s Contributions
GBKDB collected relevant information and formulated the case report with guidance from AA and MIMDA. MIMDA did the final review. All authors read and approved the final manuscript.
Acknowledgements
Dr. Harshima Wijesinghe, Senior lecturer and Consultant Histopathologist, Department of Pathology, Faculty of Medicine, University of Colombo for providing images of histology slides.
References
- Kono M, Tsuji N, Ozaki N, Matsumoto N, Takaba T, et al. (2015) Primary leiomyosarcoma of the colon. Clin J Gastroenterol 8: 217-222.
[Crossref], [Google Scholar], [Indexed]
- Al Laham O, Albrijawy R, Atia F, Shaheen J, AlTabbakh H (2021) Spindle Cell Sarcoma (SCS); a case of primary Leiomyosarcoma (LMS) of the sigmoid colon presented as intestinal obstruction. J Surg Case Reports 2021: 1-5.
[Crossref], [Google Scholar], [Indexed]
- Aggarwal G, Sharma S, Zheng M, Reid MD, Crosby JH, et al. (2012) Primary leiomyosarcomas of the gastrointestinal tract in the post-gastrointestinal stromal tumor era. Ann Diagn Pathol 16: 532-540.
[Crossref], [Google Scholar], [Indexed]
- Crystal JS, Korderas K, Schwartzberg D, Tizio SC, Zheng M, et al. (2018) Primary leiomyosarcoma of the colon: A report of two cases, review of the literature, and association with immunosuppression for IBD and rheumatoid arthritis. Case Rep Surg 2018: 1-5.
[Crossref], [Google Scholar], [Indexed]
- Lugo-Fagundo E, Fishman EK (2022) Colorectal leiomyosarcoma: A case report. Radiol Case Reports 17: 2812-2814.
[Crossref], [Google Scholar], [Indexed]
- Chen CW, Hsiao CW, Wu CC, Jao SW (2008) Rectal prolapse as initial clinical manifestation of colon cancer. Z Gastroenterol 46: 348-350.
[Crossref], [Google Scholar], [Indexed]
- Montwedi D (2019) Rectosigmoid carcinoma presenting as full-thickness rectal prolapse. BMJ Case Rep12: e230409.
[Crossref], [Google Scholar], [Indexed]
- Juric O, Lisica Sikic N, Zufic V, Matak L, Karlo R, et al. (2023) Rectal prolapse as the initial presentation of rectal cancer-A case report. Front Surg 10: 1176726.
[Crossref], [Google Scholar], [Indexed]
- Nabar S, Bittar K (2023) Rectal polyp masquerading as rectal prolapse. J Pediatr Gastroenterol Nutr 77: e68.
[Crossref], [Google Scholar], [Indexed]
- Libânio D, Meireles C, Afonso LP, Henrique R, Pimentel-Nunes P, et al. (2016) Mucosal prolapse polyp mimicking rectal malignancy: A case report. GE Port J Gastroenterol 23: 214-217.
[Crossref], [Google Scholar], [Indexed]
- Cano-Contreras AD, Meixueiro-Daza A, Grube-Pagola P, Remes-Troche JM. Giant rectal polyp prolapse in an adult patient with the Peutz-Jeghers syndrome. BMJ Case Rep 2016: bcr2016215629.
[Crossref], [Google Scholar], [Indexed]
- Johnston L, Carey F (2020) Pathology of colorectal polyps and cancer. Surg 38: 12-17.
[Crossref], [Google Scholar]
- Wang Y, Wang H, Yuan ZL, Zhao JF, Dong DB, et al. (2020) A pooled analysis of risk factors of surgically treated leiomyosarcoma of the colon in adults. World J Surg Oncol 18: 1-8.
[Crossref], [Google Scholar], [Indexed]
- Iwasa K, Taniguchi K, Noguchi M, Yamashita H, Kitagawa M (1997) Leiomyosarcoma of the colon presenting as acute suppurative peritonitis. Surg Today 27: 337-344.
[Crossref], [Google Scholar], [Indexed]
- Al Laham O, Albrijawy R, Atia F, Shaheen J, AlTabbakh H (2021) Spindle Cell Sarcoma (SCS); A case of primary Leiomyosarcoma (LMS) of the sigmoid colon presented as intestinal obstruction. J Surg Case Reports 2021: rjab515.
[Crossref], [Google Scholar], [Indexed]
- Hussain D, Baliga SK, Al-Madhi S, Hartung RU (2007) Malignant gastrointestinal stromal tumor of the rectum with prolapse. Saudi Med J 28: 1291-1292.
[Google Scholar], [Indexed]
- Devriendt S, Leman G, Vanrykel F (2020) Primary leiomyosarcoma of the colon: A case report and review of the literature. Acta Chir Belg 120: 353-356.
[Crossref], [Google Scholar], [Indexed]
- Yahagi M, Ishii Y, Hara A, Watanabe M (2019) Laparoscopic surgery to treat leiomyosarcomas of the sigmoid colon: A case report and literature review. Surg Case Reports 5: 20.
[Crossref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences