Large Infantile Hemangioma in Chest and Neck Location Causing Subglottic Narrowing and Dyspnoea
Wiktoria Nowak, Marek Bochnia, Monika Kochman and Anna Kołtowska
Wiktoria Nowak*, Marek Bochnia, Monika Kochman and Anna Kołtowska
Medical University of Silesia Piasts, Wroclaw, Lower Silesia, Poland
- *Corresponding Author:
- Nowak W
Medical University of Silesia Piasts, Wroclaw, Lower Silesia, Poland
Tel: +48 71 784 10 01
E-mail: nowakwiktoria@gmail.com
Received date: October 16, 2018; Accepted date: March 15, 2019; Published date: March 18, 2019
Citation: Nowak W, Bochnia M, Kochman M, Kołtowska A (2019) Large Infantile Hemangioma in Chest and Neck Location Causing Subglottic Narrowing and Dyspnoea. Med Case Rep Vol.5 No.2:97.
Abstract
Infantile haemangiomas (IH) are the most common softtissue tumours of infancy with a prevalence of 4·5%. Most tumours do not require intervention. Infants with hemangiomas that are life threatening, at risk of ulceration, or at risk of causing significant functional impairment, psychological impact or physical deformity should be however intensively treated. We present a case of 4-month-old female patient who was admitted to the Otolaryngology Clinic due to inspiratory and expiratory dyspnoea gradually intensifying from the first month of life. Endoscopic examination exposed normal larynx with subglottic narrowing of the trachea. CT and MR revealed a large tumour, approximately 10 cm in the CC dimension. The image primarily spoke for a large IH with neck and chest location, causing serious dyspnoea due to affection of subglottic area. Propranolol was administered at a dose of 2 mg/kg per day. In subsequent MR studies gradual regression of the lesion was observed with good clinical course. Lack of visible cutaneous presence likely delayed proper diagnosis and treatment.
Keywords
Infantile hemangioma; Infantile dyspnoea; Large infantile tumour; Propranolol; Subglottic narrowing; Subglottic tumour
Introduction
Infants with hemangiomas that are life threatening, at risk of ulceration, or at risk of causing significant functional impairment, psychological impact or physical deformity should be however intensively treated. IH are vascular neoplasms, that arise from endothelial stem cells and later proliferate by vasculogenesis, the recruitment of endothelial precursor cells to the sites of new vessel, formation followed by maturation of the cells. They may develop either from intrinsic endothelial progenitor cells (EPCs) or from angio- blasts of placental origin. IH are mistaken for those of infectious, inflammatory croup or reactive airway disease and might be present for several weeks before diagnosis.
Case Presentation
A 4-month-old female patient was admitted to the Otolaryngology, Head and Neck Surgery Clinic due to inspiratory and expiratory dyspnoea, accompanied by difficulties in feeding, without changes in voice color. On admission the patient didn’t present cyanosis or auditory alterations of a whistling and whortling nature over the pulmonary fields. Previous history included dyspnoea gradually intensifying from the first month of life, 5 hospitalizations in pediatric departments due to bronchitis with dyspnoea, reducing after treatment with antibiotics and steroids.
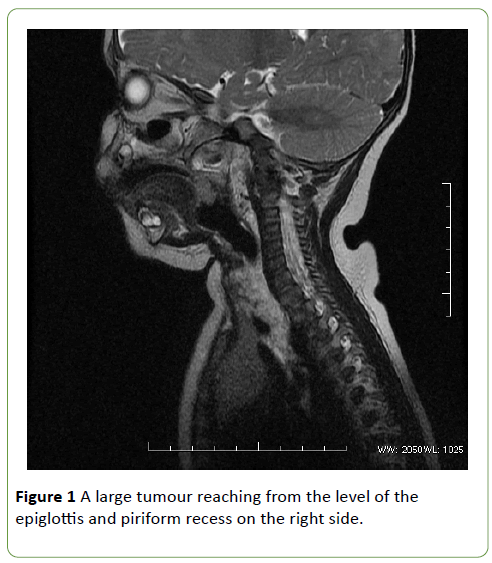
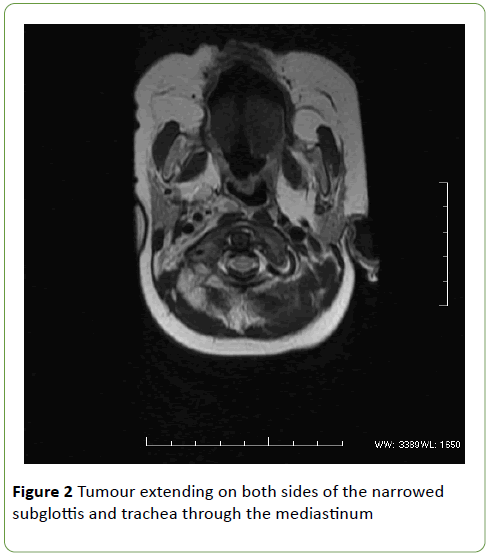
Endoscopic examination exposed normal larynx with subglottic narrowing of the trachea. CT and MR revealed a large tumour reaching from the level of the epiglottis and piriform recess on the right side, extending on both sides of the narrowed subglottis and trachea through the mediastinum (backward from the thyroid gland and around the tumour reached dimensions 30 mm TR × 16 mm AP) on both sides until the level of the trachea bifurcation (Figures 1 and 2).
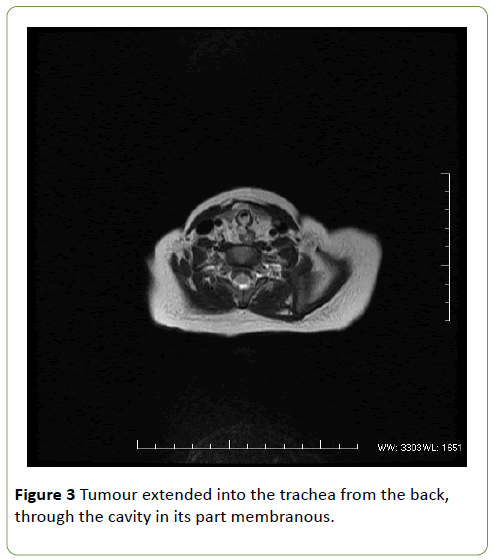
Upwards, the tumour also extended in the space of the large neck vessels and on the right side occupied the space under the sternocleidomastoid muscle at this location reached 2 × 4 cm and down to the pterygopalatine fossa. Lateral and backwardly, it grew into the space of the neck muscles and in the paraspinal space. The tumour extended into the trachea from the back, through the cavity in its part membranous (2 mm wide) to a depth of 4 mm and width 6 mm, narrowing its diameter to 1.4 mm on a length of 9 mm (Figure 3). The total length of the tumour was approximately 10 cm in the CC dimension. The tumour exhibited intense contrast enhancement, with small twisting signal voids corresponding to small vessels.
Final Diagnosis
The image primarily spoke for a large Infantile Hemangioma (IH) with neck and chest location, causing serious dyspnoea due to affection of subglottic area. Lack of visible cutaneous presence likely delayed proper diagnosis and treatment.
Hospital Course
The girl was consulted with a pediatric surgeon and cardiologist. Before starting treatment, ECG and echo of the heart were performed, the glucose level was determined. Propranolol was administered at a dose of 2 mg/kg per day.
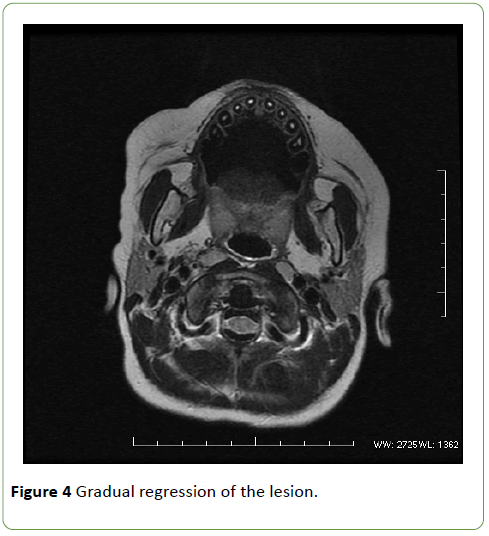
The first control MR was performed after 3 months. In the study the extent of hemangioma was partially reduced-on the right side at the height of the trachea it measured the maximum of 17 mm in the transverse dimension (previously 20 mm), leftsided 8 mm (previously 20 mm), tracheal constriction up to 3 mm (previously 2 mm). In subsequent MR studies further, gradual regression of the lesion was observed (Figure 4).
Discussion
IH are vascular neoplasms, that arise from endothelial stem cells and later proliferate by vasculogenesis, the recruitment of endothelial precursor cells to the sites of new vessel, formation followed by maturation of the cells. They may develop either from intrinsic endothelial progenitor cells (EPCs) or from angio-blasts of placental origin. IH growth is affected by intrinsic influences, such as angiogenic and vasculogenic factors within the IH, and by external factors such as tissue hypoxia and developmental field disturbances. A unifying theory proposes that circulating endothelial progenitor cells (EPCs) migrate to locations in which conditions are favorable for growth into placentalike tissues [1-3].
They are more common among female (with a range of 1.4:1 to 3:1), in Caucasians, in multiple births, and increased among preterm infants, affecting 22% to 30% of infants weighing less than 1 kg [1].
Although there is no official guidelines on treatment of IH, consensus report suggests use of oral propranolol at a dose 2 mg/kg per day, which is safe, cheap and causing relevantly few side effects (mostly accelerations of pre-existing asthma, bradycardia, hypoglicemia, sleeping disorders) [4-8].
The most dramatic improvement using propranolol for IH occurs within 3 to 4 months of initiation of therapy. However, many investigators continue therapy until patients reach an age when IH would normally begin to regress without treatment (until at least 8 to 12 months of age in most studies) [1-9].
Dyspnoea at infancy might be caused by several conditions, e.g., infectious (croup), foreign body aspiration, recurrent papillomas and congenital causes: Subglottic stenosis, laryngomalacia, vocal cord paralysis, laryngeal membranes, laryngocele.
IH with subglottic localisation are extremally rare cause of infants distress. Patients usuallly present symptoms like biaphasic stridor and barky caugh within the first 6 months old life. Often they are mistaken for those of infectious, inflammatory croup or reactive airway disease and might be present for several weeks before diagnosis. Usually they are not causing difficulties in feeding. Approximately half of infants have some cutaneous presentation [1-12].
Conclusion
Infantile haemangiomas (IH) are the most common soft-tissue tumours of infancy with a prevalence of 4·5%. They are characterized by an initial proliferation followed by spontaneous involution over the next 5–10 years, often leaving a fibro-fatty residuum. Most tumours do not require intervention. Infants with hemangiomas that are life threatening, at risk of ulceration, or at risk of causing significant functional impairment, psychological impact or physical deformity should be however intensively treated.
References
- Darrow DH, Greene AK, Mancini AJ, Nopper AJ (2015) Diagnosis and management of infantile hemangioma. Pediatrics 136: e1060-e1104.
- Léauté-Labrèze C, Harper JI, Hoeger PH (2017) Biology of infantile hemangioma. Semin Perinatol 18: 131-133.
- Itinteang T, Withers AHJ, Davis PF, Tan ST (2014) Biology of Infantile Hemangioma. Front Sur 1: 1-10.
- Fette A (2013) Propranolol in use for treatment of complex infant hemangiomas: Literature review regarding current guidelines for preassessment and standards of care before initiation of therapy. Sci World J 2: 1.
- Carlyle WC, Mcclain JB, Tzafriri AR, Bailey L, Zani BG, et al. (2015) HHS Public Access 162: 561-567.
- Drolet BA, Frommelt PC, Chamlin SL, Haggstrom A, Bauman NM, et al. Initiation and use of propranolol for infantile hemangioma: Report of a consensus conference. Pediatrics 131: 128-140.
- Smithson SL, Rademaker M, Adams S, Bade S, Bekhor P, et al. (2017) Consensus statement for the treatment of infantile haemangiomas with propranolol. Australas J Dermatol 58: 155-159.
- Xiao Q, Li Q, Zhang B, Yu W (2013) Propranolol therapy of infantile hemangiomas: Efficacy, adverse effects and recurrence. Pediatr Surg Int 29: 575-581.
- Chang L, Gu Y, Yu Z, Ying H, Qiu Y, et al. (2017) When to stop propranolol for infantile hemangioma. Sci Rep 7: 1-7.
- Sherrington CA, Sim DKY, Freezer NJ, Robertson CF (1997) Subglottic haemangioma. Arch Dis Child 76: 458-459.
- Léauté-Labrèze C, Harper JI, Hoeger PH (2017) Infantile haemangioma. Lancet 390: 85-94.
- Lee KC, Bercovitch L (2013) Update on infantile hemangiomas. Semin Perinatol 37: 49-58.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences