Laparoscopic Cholecystectomy of Gallbladder Stone Presenting as Empyema in a 9 Year-Old Boy: A Case Report
Sidoun M*, Elfageh M, Belhaje A and Elfageh W
1Department of Surgery, National Cancer Institute, Misurata, Libya
2Department of Anaesthesiology, National Cancer Institute, Misurata, Libya
- *Corresponding Author:
- Mohamed Alhashmi Sidoun
Department of Surgery, National Cancer Institute
Misurata, Libya
Tel: +218914058503
Email: dr.sidoun.mohamed1982@gmail.com
Received Date: January 25, 2020; Accepted Date: February 12, 2020; Published Date: February 19, 2020
Citation: Sidoun M, Elfageh M, Belhaje A, Elfageh W (2020) Laparoscopic Cholecystectomy of Gallbladder Stone Presenting as Empyema in a 9 Years-Old Boy: A Case Report. Med Case Rep Vol.6 No.1: 132.
DOI: 10.36648/2471-8041.6.1.132
Abstract
Background: The gall bladder stones (GBS) are common disease related to diet habit, obesity, hematological diseases, diabetes mellitus and receiving total parenteral nutrition. GBS is a rare cause of hospitalization of pediatric patients but have been increasingly diagnosed in recent years due to widespread use of ultrasonography. The aim of this case report study is to determine the clinical presentation, risk factors, valuable diagnostic procedures and outcome of laparoscopic management of cholelithiasis in children. Case report: Our case is a 9-year-old boy with empyemic gallbladder complaining of attacks of colicky epigastric pain associated with recurrent vomiting. On abdominal palpation, there is positive sign of deep tenderness at hypochondrium area and positive murphy sign. He has central obesity with BMI 29.9, skin folds more than 3.5 cm and waist circumference more than 90 cm. He has History of high cholesterol and fatty diet and fast food habit, prolonged intake of vitamin D and positive family history. While, no other associated risk factors were detected in our patient. All laboratory investigations were within normal ranges even for his lipid profile. Although, empyema was present, no leukocytosis was detected. Abdominal ultrasound showed the gall bladder wall is slightly thick surrounded by pericholycystic fluid, solitary gall bladder stone of 3 cm size and normal CBD. While, post-operative histopathological examination revealed thick wall gallbladder with multiple tiny stones of cholesterol type. The patient was treated with laparoscopic cholecystectomy with promising outcome and no complications. Conclusion: Pediatric surgeons should consider cholecystolithiasis as from differential diagnosis of abdominal pain associated with vomiting in children. Empyema of gallbladder should be considered once murphy sign is positive in such child patients. Child obesity, fatty diet, vitamin D deï¬Ãƒâ€šÃ‚Âciency and family history are possible risk factors. Ultrasonography is the mainstay of diagnosis. Laparoscopic cholecystectomy is the appropriate management for symptomatic cholelithiasis in children.
Keywords
Gallstones; Empyema; Children; Boy; Laparoscopic cholecystectomy
Introduction
Gallbladder disease today is a common health problem affecting 10% to 15% of the adult population [1]. In contrast to adulthood, gallstones in childhood are rare. However, the incidence is increasing with the diagnosis of asymptomatic gallstones with the widespread use of ultrasonography [2]. Risk factors for gallstones in children include hemolytic disease, obesity, prematurity, sepsis, total parenteral nutrition (TPN), chronic liver disease, inflammatory bowel diseases, diuretic use, and ceftriaxone use [3]. Sickle cell disease is the most important cause of cholelithiasis in children. Pigment gallstones affect 15% of children with SCD younger than 10 years of age and more than 80% of those older than 30 years [4]. Gallstones found in adults are primarily cholesterol stones or mixed stones but in children pigment stones formed as a consequence of hemolytic diseases like sickle cell anemia, thalassemia and hereditary spherocytosis are more common [5]. In general, gallstones are uncommon in children, with patients under 15-year-old, comprising only 0.1-0.2% of the incidence of the disease [6]. Even so, define the association between the obesity and gall bladder stones in pediatric population were very few studies and taking long time on the PubMed. These few clinical reports suggest that hemolytic diseases are no longer the most frequent cause of pediatric gallbladder disease. Concomitant with the epidemic of childhood obesity and the shift towards extreme childhood obesity, the prevalence of gallstones in children and adolescents may be increasing due to childhood obesity [7]. In addition of risk of GBS in obese youngest children now days, the risk of choledocholithiasis had significantly higher with high BMI than those with simple cholelithiasis [8]. Cholelithiasis is sometimes diagnosed in patients incidentally or as silent stones. In some other cases, they are reported in association with clinical symptoms such ascholecystitis and cholangitis [9,10]. However, there is little information about the epidemiology of GBS in children from Libya and no consensus among Libyan pediatric surgeons regarding management of gallstones in children. We want to report our experience of a rare case of 9 years-old with gall bladder large stone and sludge bile, complicated with empyema, operated straight forward by urgent laparascopic cholecystectomy.
Case Presentation
Obese male child 9-year-old presented to our outpatient clinic after having attended several other facilities, complaining of attacks of colicky epigastric pain associated with recurrent vomiting 2 months back, aggravated by fatty meal, relieved by IV medications and vomiting. History taking revealed high cholesterol and fatty diet and fast food habit; long duration of Vitamin D intake and a positive family history of laparoscopic cholecystectomy (LC) for his mother and Uncle (his mother`s brother). No history of easily bruising, oral mucosa petechial rash, bleeding tendency, blood transfusion or previous operations. Physical examination revealed normal vital signs (temperature, pulse rate, blood pressure) were normal. The child was obese with abdominal skin fold 5 cm, axillary skin folds 3 cm, Height 140 cm, weight 58 kg, body mass index (BMI) is 29.9 (normal range in this age is between 14.2 and 19.4), waist circumference 93 cm, mid-arm circumference 29cm and mid-thigh circumference 55 cm. No jaundice, no pallor and no edema were present and oralmucosa and nostrils were completely normal. Per abdominal examination showed no distension, normal movement with breathing, no scratch markings, no visible mass. Generally, the abdomen was soft by palpation with positive sign of deep tenderness at hypochondrium area and positive murphy sign. Bowel sounds was normally heard.
Laboratory findings
Routine laboratory examination was done including WBC, full blood count, ESR renal function test, liver function tests, serum amylase and lipase, serum sodium and potassium, HBA1C and blood sugar. All the previous investigations were within normal limits. Total bilirubin was 0.2 mg/dl and Alkaline phosphatase was 302 U/L which is not considered to be high in this age group. Other was normal levels. In addition, lipid profile (triglycerides, cholesterol, HDL, LDL) was normal No other laparotomy investigations were indicated.
Radiological findings
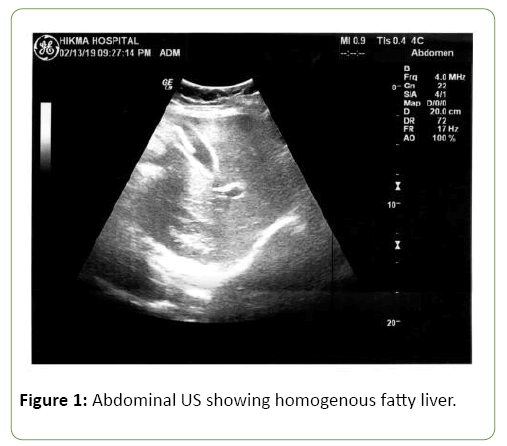
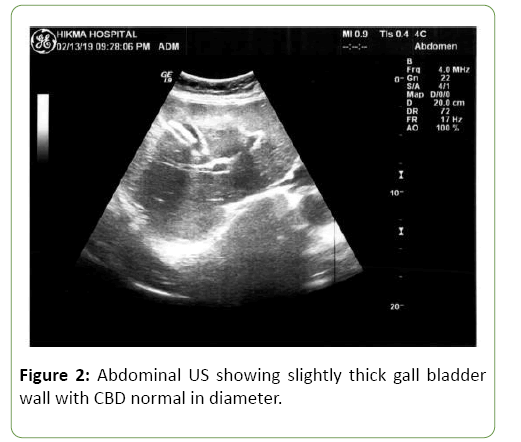
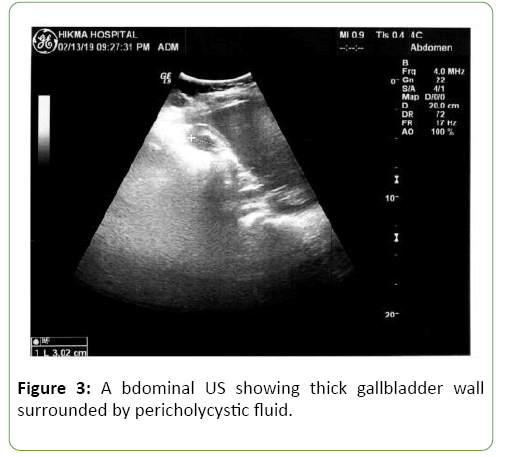
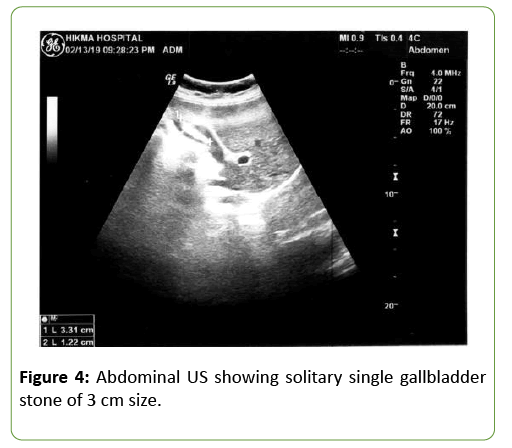
Abdominal Ultrasonography showed homogenous fatty liver, the gall bladder wall is slightly thick surrounded by pericholycystic fluid, solitary single gall bladder stone of 3 cm size, Common Bile Duct is normal in diameter, spleen and otherwise are normal (Figures 1-4).
Laparoscopic cholecystectomy
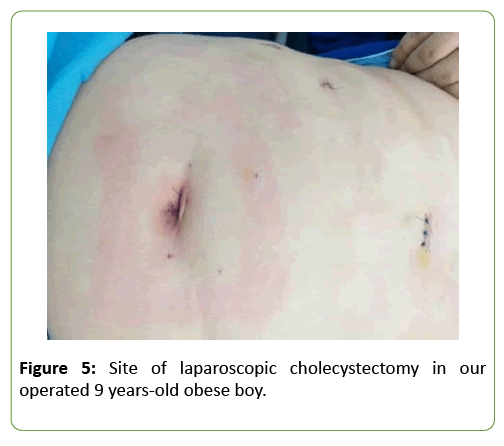
The positive murphy sign and the deep tenderness of the right hypochondria area regardless the afebrile status and normal level of WBC, let our thinking and decision are very clear and the patient was candidate for elective laparoscopic cholecystectomy. After appropriate preoperative investigations and discussion with anesthesia team, critical view Laparoscopic cholecystectomy was done under general anesthesia, the time of operation was one hour and twenty minutes, standard four laparoscopic ports inserted, after pneumoperitoneum achieved at 12 mmhg and camera 300 inserted, the view was difficult due to fatty omentum, the gall bladder was empyemic and large in size with significant adhesions and edematous wall, release of adhesions performed and critical view applied, The Calot’s triangle has been skeletonized, was found normal. Cystic duct and cystic artery were identified, clipped and ligated, no gall bladder bed oozing is noted and finally cholecystectomy done (Figure 5).
Recovery of the patient was smoothly without any complications, patient kept in the ward nil per mouth with iv fluid maintainace, Antibiotics IV, perfelgan IV and ranitidine IV. 12 hours post-operative, the general condition was normal, patient mobilized, his vital signs were within normal, afebrile, the bowel sound early regain to function, diet initiation with no vomiting and nausea. He has been discharged DAY 2 post operation with well general condition; no complain with only few cc serousangouinus discharge in the drain. Stitches has been removed one week after operation. Regular follow up applied at 2 months, 6 months and 1 year. The patient was symptomatic free with no GIT or Cholecystectomy related complications.
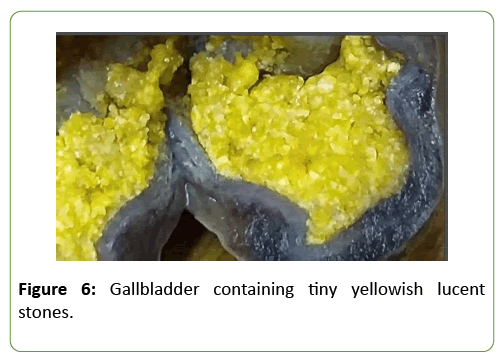
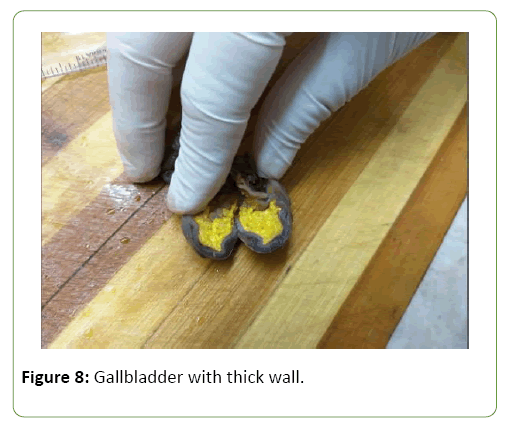
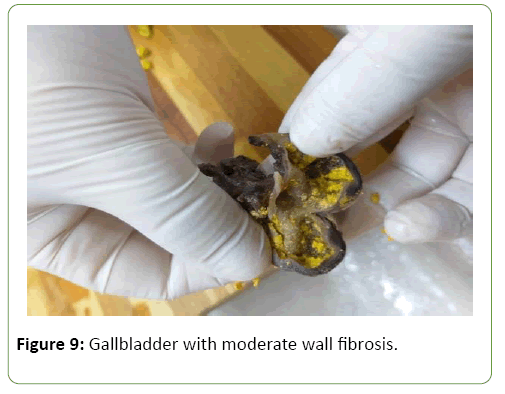
Histopathological findings
After cholecystectomy, the biopsy was sent to histopathology. The result showed that lumen contains tiny yellowish lucent stones, ulcerated mucosa, moderate wall fibrosis and transmural infiltrations of lymphocyte and eosinophil cells (Figures 6-9).
Discussion
Little information is known about the epidemiology of gallbladder stones in children. The exact prevalence of gallstones in children is not known but some studies have shown an overall prevalence of gallstone disease of 0.13% to 0.2% in children [11,12]. Cholelithiasis in children have been increasing due to increased use of total parenteral nutrition, frusemide and phototherapy in the infants [11].
Our patient is a 9 years-old boy with central obesity with skin folds more than 3.5 cm and waist circumference more than 90 cm, this overweight was helpful to us in diagnosis. He has History of high cholesterol and fatty diet and fast food habit. This is supported by other studied in which the prevalence of gallstones among obese children was shown to be quite high (2%) [13].
Although both genders are equally aected in early childhood, most previous studies have demonstrated a female predominance in pediatric gallbladder disease, starting from puberty. In fact,most cases of cholelithias is at young age are diagnosed in the second decade of life [14-16].
The relation of cholesterol gall bladder stones in obese child could be related to cholesterol metabolism or related to the compression effect of fatty omentum and intestine on the stasis of biliary radicles (lithogenic effect). hypersaturation of bile caused by either increased hepatic cholesterol uptake or increased cholesterol synthesis. Second, dysmotility and impaired contraction of the gallbladder is caused by the direct influence of cholesterol at the cellular level onto the plasma membrane of smooth muscle cells in the gallbladder wall [8].
Tsai performed prospective study of abdominal adiposity and gallstone disease in US men, the conclusion was, the collected data for abdominal obesity in relation to the incidence of symptomatic gallstone disease suggested presence of a significant association between abdominal adiposity and the incidence of symptomatic gallstone disease. As measures of abdominal adiposity, abdominal circumference and waist-to-hip ratio predict the risk of developing gallstones independently of body mass index [17].
Several risk factors for gallstones in adults are wellestablished, including age, female sex, Hispanic ethnicity, obesity, use of female sex hormones, pregnancy, sedentary lifestyle, and a family history of gallstones. However, scant information is available regarding risk factors for gallstones in the pediatric population [18].
In our patient, there was positive family history and history of long duration of vitamin D intake. While, many other risk factors were absent as no hemolytic diseases, no diabetic, no history of biliary atresia or choledochal cyst.
Generally, the incidence and prevalence of cholelithiasis are influenced by age, gender, genetics, and race. Epidemiological studies have indicated the involvement of genetic factors in the formation of cholelithiasis. The e ect of a gene on incontinentia pigmenti chromosome has been confirmed in the formation of cholelithiasis. In fact, patients with ABCB11 mutations are at a higher risk of cholelithiasis [19].
While, Onal and his collages in their study revealed that vitamin D deficiency is suggested to be associated with gallbladder stasis, and a role for vitamin D supplementation is thought to have potential to prevent gallstones in this special population [20]. This may explain the occurrence of gallbladder stones in our patient as a result of vitamin D deficiency in early childhood, and that was not due to increased intake of vitamin D as it seems to be. Our patient takes vitamin D to replace its deficiency and the deficiency of vitamin D itself is responsible for gall bladder stasis with development of stones in our case. In other studies, long-term use and high dose use of ceftriaxone was founded to be associated with increase the probability of occurrence of gallstones [21].
Our patient was complaining of attacks of colicky epigastric pain associated with recurrent vomiting. On abdominal palpation, there is positive sign of deep tenderness at hypochondrium area and positive murphy sign. The results of laboratory investigation was mostly normal in our case, even WBCs was of normal level despite the presence of empyema and that may be explained as a result of the previous empirical antibiotic course administrated in other clinics before the case attended our outpatient clinic. Abdominal ultrasound was the method of choice in diagnosis of the reported case. While, radiological investigations other than ultrasound (i.e., MRCP) was not indicated, so it was not performed. Cholelithiasis in children have been increasingly diagnosed in recent years due to better medical imaging (especially ultrasonography) and its usage in investigating children with unexplained abdominal pain [11]. So, we should consider the Cholecystolithiasis as from the differential diagnosis of unexplained abdominal pain associated with vomiting in children and we have to confirm that by conducting abdominal US, to avoid the complications of GBS as acute cholecystitis, empyema, biliary pancreatitis and sepsis. In addition, empyema of gallbladder should be considered once murphy sign is positive in such child patients even with absence of leukocytosis.
Because The youngest age of the patient, making the final decision of laparoscopic cholecystectomy (L.C.) is delayed from other clinics, to considerations of exclusion of some risk factors as hemolytic diseases. For this reason, he was operated lately. The patient was treated with laparoscopic cholecystectomy with prolonged time but with clear anatomy. This is in agreement with the recommendations of other studies, which stated that the laparoscopic cholecystectomy is safe and preferable in pediatric patients. L.C. have better results, short post-operative hospital stays and with low complication rates in particular, zero bile duct injuries were noted [22,23].
Post-operative histopathological examination revealed thick wall gallbladder with multiple tiny stones of cholesterol type. Our findings were compatible with that of Agostino Di Ciaula who investigated several pathogenic mechanisms in literature review article, the Major pathogenetic factors for cholesterol gallstones include a genetic background, hepatic hypersecretion of cholesterol and supersaturated bile which give life to precipitating cholesterol crystals that accumulate and grow in a sluggish gallbladder [24]. While, our study is in contrary to our other studies stated that pigment stones containing bilirubin salts are more common in the pediatric population. Nevertheless, our explanation is that these types of bilirubin stones are associated with hemolytic disorders, most commonly sickle cell anemia, which no of them were identified in our patient.
Conclusion
Despite cholelithiasis is rare in children, pediatric surgeon should consider the cholecystolithiasis as from differential diagnosis of abdominal pain associated with vomiting in the youngest age group even with absence of positive laboratory investigations, to avoid the complications of GBS as acute cholecystitis, empyema, biliary pancreatitis and sepsis. In addition, empyema of gallbladder should be considered once murphy sign is positive in such child patients even with absence of leukocytosis. Ultrasonography is the mainstay of diagnosis and it is very useful in detecting these cases. Child obesity, fatty diet, and family history were the most frequent risk factors in our patient. Vitamin D deficiency is suggested to be associated with gallbladder stasis and may increase the risk of cholelithiasis. Laparoscopic cholecystectomy is the appropriate management for symptomatic cholelithiasis in children, as it can be performed safely using technique of single-incision. We emphasize the importance of further researches to explore the epidemiology of gallbladder disease in children for better diagnosis and management of such cases.
Informed Consent
An informed consent was obtained from our patient's parents for publication of this case report and the accompanying images.
Competing Interests
The authors declare they have no competing interests.
References
- Stinton LM, Myers RP, Shafer EA (2010) Epidemiology of gallstones. Gastroenterol Clin N Am 39:157-169.
- Bogue CO, Murphy AJ, Gerstle JT, Moineddin R, Daneman P (2010) Risk factors, complications, and outcomes of gallstones in children: A single center review. J Pediatr Gastroenterol Nutr 50:303-308.
- Serdaroglu F, Koca YS, Saltik F, Koca T, Dereci S, et al. (2016) Gallstones in childhood: Etiology, clinical features, and prognosis. Eur J Gastroenterol Hepatol 28: 1468-1472.
- Currò G, Meo A, Ippolito D, Pusiol A, Cucinotta E (2007) Asymptomatic cholelithiasis in children with sickle cell disease: Early or delayed cholecystectomy?. Ann Surg 245:126-129.
- Chhabra SK, Ahmed Z, Massey A, Agarwal S, Vij V, et al. (2016) Laparoscopic cholecystectomy in a 2 year old male child with choleilithiasis and recurrent right hypochondrial pain: A case report and review of literature. Int J Surg Case Rep 26:142-145.
- Barthel ER, Pierce JR, Zmora O, Harlan SR, Russell S, et al. (2012) Calcified gallstone in a 3 year-old boy: A case report. BMC Res Notes 5:433.
- Koebnick C, Smith N, Black MH, Porter AH, Richie BA, et al. (2012) Pediatric obesity and gallstone disease: results from a cross- sectional study of over 510,000 youth. Pediatr Gastroenterol Nutr 55: 328.
- Frybova B, Drabek J, Lochmannova J, Douda L, Hlava S, et al. (2018) Cholelithiasis and choledocholithiasis in children: Risk factors for development. PloS One. 13(5).
- Karami H, Kianifar HR, Karami S (2017) Cholelithiasis in children: A diagnostic and therapeutic approach. J Pediat Rev 5: e9114.
- Vegunta RK, Raso M, Pollock J, Misra S, Wallace LJ, et al. (2005) Biliary dyskinesia: The most common indication for cholecystectomy in children. Surgery 138:726-731.
- Poddar U (2010) Gallstone Disease in Children. Indian Pediatrics 47:945-953.
- Wesdorp I, Bosman D, De Graaff A, Aronson D, Van der Blij F, et al. (2000) Clinical presentations and predisposing factors of cholelithiasis and sludge in children. J Pediatr Gastroenterol Nutr 31: 411-417.
- Kaechele V, Wabitsch M, Thiere D, Kessler AL, Haenle MM, et al. (2008) Prevalence of gallbladder stone disease in obese children and adolescents: influence of the degree of obesity, sex and pubertal development. J Pediatr Gastroenterol Nutr 42: 66-70.
- Wesdorp I, Bosman D, De Graaff A, Aronson D, VanderBlij F, et al. (2000) Clinical presentations and predisposing factors of cholelithiasis and sludge in children. J Pediatr Gastroenterol Nutr 31:411-417.
- Mehta S, Lopez ME, Chumpitazi BP, Mazziotti MV, Brandt ML, et al. (2012) Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics 129:82–88.
- Punia RP, Garg S, Bisht B, Dalal U, Mohan H (2010) Clinico-pathological spectrum of gallbladder disease in children. Acta Paediatr 99:1561-1564.
- Tsai CJ, Leitzmann MF, Willett WC, Giovannucci EL (2004) Prospective study of abdominal adiposity and gallstone disease in US men. Am J Clin Nutr 80:38-44.
- Bãlãnescu RN, Bãlãnescu L, Drãgan G, Moga A, Caragaåã R (2015) Biliary lithiasis with choledocolithiasis in children. Chirurgia (Bucur) 110:559-561.
- Wyllie R, Hyams JS, Kay M (2016) Pediatric gastrointestinal and liver disease. (5th edn). Philadelphia, PA: Elsevier, USA.
- Onal E, Berker D, Guler S (2016) Vitamin D deficiency and gallbladder stasis. Dig Dis Sci 60:3823-3824.
- Bor O, Dinleyici EC, Kebapci M, Aydogdu SD (2004) Ceftriaxone-associated biliary sludge and pseudocholelithiasis during childhood: a prospective study. Pediatr Int 2004; 46:322–324.
- Zeidan MM (2014) Laparoscopic cholecystectomy in the pediatric population: A single-center experience. Surg Laparosc Endosc Percutan Tech 24:248-250.
- Langballe KO, Bardram L (2014) Cholecystectomy in Danish children-A nationwide study. J Pediatr Surg 49:626-630.
- Di Ciaula D, David QH, Wang H, Portincasa P (2018) An update on the pathogenesis of cholesterol gallstone disease. Curr Opin Gastroenterol 34:71-80.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences