Isolated Glycosuria in a Child in Sri Lanka
Mihira Manamperi*, Iresha Jasinghe, Tharindi Suriyapperuma and Thilini Somaratne
DOI10.36648/2471-8041.21.7.192
Mihira Manamperi*, Iresha Jasinghe, Tharindi Suriyapperuma and Thilini Somaratne
Internal Medicine Department, District General Hospital, Gampaha, Sri Lanka
- *Corresponding Author:
- Mihira Manamperi Internal Medicine Department, District General Hospital, Gampaha, Sri Lanka, Tel: + 94775212760; E-mail: mihira123@gmail.com
Received date: July 02, 2021; Accepted date: July 16, 2021; Published date: July 23, 2021
Citation: Manamperi M, Jasinghe I, Suriyapperuma T, Somaratne T (2021) Isolated Glycosuria in a child in Sri Lanka. Med Case Rep Vol.7 No.7. 192
Abstract
Renal glycosuria or benign glycosuria is a rare autosomal recessive condition where glucose is excreted from the urine while having normal serum glucose levels, as a result of a defect in low affinity sodium glucose transporter (SGLT2) in the proximal convoluted tubule (PCT) of the nephron. Benign glycosuria or renal glycosuria has been described as an autosomal recessive disorder. It is usually benign and most of the time asymptomatic and considered as an incidental finding. However, childhood glycosuria is associated with many other tubular disorders such as an Fanconi’s syndrome, Cystinosis, Wilson’s disease, Lowe’s syndrome, Tyrosinaemia and the initial presentation of childhood diabetes mellitus
Introduction
Renal glycosuria or benign glycosuria is a rare autosomal recessive condition where glucose is excreted from the urine while having normal serum glucose levels, as a result of a defect in low affinity sodium glucose transporter (SGLT2) in the proximal convoluted tubule (PCT) of the nephron. This condition is asymptomatic and most of the time diagnosed as an incidental finding.
Case History
A 3 year 4 month old previously healthy Sri Lankan boy being investigated for a febrile illness was found to have persistent glycosuria. He was born to healthy non consanguineous parents at term with a birth weight of 2.52 kg. He hadn’t developed urinary tract infections and didn’t having polyuria, polydipsia or weight loss. His growth parameters were within normal range. He was developmentally normal with normal systems examination. There were multiple readings of random blood glucose levels with positive urine glucose.
His fasting blood sugar (FBS) was 4.2 mmol/L with a normal HbA1c. The urine Clinitest and Clinistix were strongly positive. Urine ketone bodies were negative. Urine full report showed +++ glucose on multiple occasions yet negative for rest of the components such as protein, nitrites, leucocytes, blood and organisms.
The boy’s renal functions were assessed with; protein to creatinine ratio 15 mg/mmol, (within the normal limit), serum osmolality and urine osmolality, 291 mOsmol/kgH2O and 642 mOsmol/kgH2O, respectively.
His renal functions, liver functions and electrolytes were normal. Phosphate to creatinine ratio, calcium to creatinine ratio, magnesium to creatinine ratio, sodium to creatinine ratio and potassium to creatinine ratio were performed and found to be within normal limits. The lipid profile was normal [1].
The mother’s Clinitest and Clinistix tests were negative. The father was employed overseas and unavailable for screening. A diagnosis of isolated glycosuria was made based on the above investigations (Figure 1).
Discussion
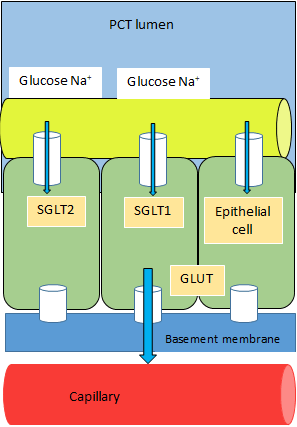
In a normal child with normal tubular function glucose will only appear in urine when the serum glucose level exceeds the renal threshold. The sodium coupled glucose transporters (SGLT) and glucose transporters (GLUT) are responsible for glucose transport in both kidney and the intestine. Both the intestine and kidney have high-affinity sodium glucose co transporters (SGLT1). However low affinity sodium glucose transporter (SGLT2) is specific to kidneys. SGLT transports glucose from brush border to epithelial cells and out of the epithelial cell via GLUT. In normal circumstances, 90% of the filtered glucose is reabsorbed by the first segment of the PCT via high affinity SGLT1. The remaining glucose is reabsorbed from the second and third part of the PCT via low affinity SGLT2. It has been hypothesized that a defect in SGLT2 leads to failure to reabsorb the remaining glucose and hence glucose appears in the urine. SGLT1 and SGLT2 are members of the SLC5A gene family (also known as the sodium substrate symporter gene family (SSSF)). Inherited form of this disorder is called familial renal glucosuria (FRG). FRG has recently been shown to result from mutations in SLC5A2, encoding the kidney-specific low-affinity/ high-capacity Na+/glucose cotransporter, SGLT2 [2].
Benign glycosuria or renal glycosuria has been described as an autosomal recessive disorder. It is usually benign and most of the time asymptomatic and considered as an incidental finding [3]. However, childhood glycosuria is associated with many other tubular disorders such as Fanconi’s syndrome, Cystinosis, Wilson’s disease, Lowe’s syndrome, Tyrosinaemia and the initial presentation of childhood diabetes mellitus. Almost all the above mentioned disorders will have other clinical features such as eye abnormalities (glaucoma, cataract, Keyser-Fleischer rings), growth retardation, liver failure, polyuria and polydipsia. Renal glycosuria is a benign condition [4, 5]. The authors’ approach to the immediate postdiagnosis management of these infants and toddlers is as follows. If admitted, children should remain in hospital only as long as their clinical condition demands (usually less than two to four days). If the child is not hospitalized, the family should return on a daily basis for two to four days to the diabetes day care facility: they arrive before breakfast and leave after dinner each day. During this time, parents and/or other primary caregivers are taught the ‘survival skills’ needed to care for an infant or toddler with diabetes, ie, insulin injection technique, blood glucose monitoring, appropriate infant feeding, and recognition and treatment of hypoglycemia. More complete diabetes education is carried out on an ambulatory basis as the family begins to deal with the diabetes at home; this is invariably accomplished within two to four weeks of diagnosis. Throughout this early phase, general medical care and psychosocial support are provided by a core diabetes team experienced in the care of young patients, including a paediatric endocrinologist, diabetes nurse, dietitian and social worker. It is often beneficial to have home care providers assist the family with the routines after their initial period in day care. However it is a diagnosis of exclusion of the other disorders which includes a thorough clinical evaluation and assessment of the other tubular functions to identify early stages of more serious conditions as above. Genetic counseling will be of benefit for affected individuals and their families case [6].
Conclusion
Renal glycosuria is a benign condition. However it is a diagnosis of exclusion of the other disorders which includes a thorough clinical evaluation and assessment of the other tubular functions to identify early stages of more serious conditions as above. Genetic counseling will be of benefit for affected individuals and their families.
References
- Magen D, Sprecher E, Zelikovic I, Skorecki K (2005) A novel missense mutation in SLC5A2 encoding SGLT2 underlies autosomal recessive renal glucosuria and aminoaciduria. Kidney Int 67: 34-41.
- Jhaveri KD, Meir LR, Chang BS, Parikh R, Wanchoo R, et al. (2020) Thrombotic microangiopathy in a patient with COVID-19. Kidney Int 98(2):509-512.
- Ferrario CM, Jessup J, Chappell MC, Averill DB, Brosnihan KB, et al. (2005) Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation 111(20):2605-10.
- Iregbu KC, Nwajiobi-Princewill PI (2013) Urinary tract infections in a tertiary hospital in Abuja, Nigeria. Afr J Clin Exper Microbiol. 14(3):169â??173.
- Miller M, Dalakos T (2017) Recognition of partial defects in antidiuretic hormone secretion. Ann Intern Med. 73:721-729
- Robertson GL (1995) Diabetes insipidus Endocrinol Metab Clin North Am 549-572.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences