Hyperhomocysteinemia and Pregnancy: About a Case and Literature Review
Bouchaib Allae Eddine*, Mamadou Alpha Balde, Abdellah Babahabib, Moulay El Mehdi Elhassani and Jaouad Kouach
Department of Gynecology-Obstetrics, Mohamed V Military Training Hospital, Rabat, Morocco
Corresponding Author:
Bouchaib Allae Eddine
Department of Gynecology-Obstetrics, Mohamed V Military Training Hospital,
Rabat, Morocco,
E-mail: alae.eddine.crislax@gmail.com
Received date: January 31, 2023, Manuscript No. IPMCRS-23-15731; Editor assigned date: February 02, 2023, PreQC No.IPMCRS-23-15731 (PQ); Reviewed date: February 13, 2023, QC No. IPMCRS-23-15731; Revised date: February 23, 2023, Manuscript No. IPMCRS-23-15731 (R); Published date:March 02, 2023, DOI: 10.36648/2471-8041.9.1.262
Citation: Eddine BA, Balde MA, Babahabib A, Elhassani MEM, Kouach J (2023) Hyperhomocysteinemia and Pregnancy: About a Case and Literature Review. Med Case Rep Vol.9 No.1:262.
Abstract
Homocysteine (Hct) is a substance produced in the metabolism of methionine that can be found in our daily diet. Mutation of the methylenetetrahydrofolate reductase gene, especially for women with low folate intake. Hyperhomocysteinemia (HHct) can be caused by several factors, such as lack of folic acid, vitamin B6 and B12 deficiency, hypothyroidism, medications, genetic abnormalities, aging and kidney dysfunction. Increased homocysteine in peripheral blood can lead to vascular disease, coronary artery dysfunction, atherosclerotic changes and embolic disease. Hence, increased thrombogenic activity in pregnant women upstream of the trophoblast plug resulting in clot formation and either early or late abortion. Recent studies have reported that hyperhomocysteinemia is associated with numerous pregnancy complications, including abortion disease, preeclampsia, preterm birth, hematoma placentae, fetal growth restriction and gestational diabetes. Thus, to avoid thrombosis, treatment is based on anticoagulants, sometimes combined with low-dose aspirin, especially for its anticoagulant effect. In this article, we report the case of a patient with a history of abortive disease on hyperhomocysteinemia who carried a pregnancy to term, while recalling the metabolism of homocysteine, its impact on pregnancy and the interest of prescribing the folic acid to avoid complications related to hyperhomocysteinemia.
Keywords
Hyperhomocysteinemia; Pregnancy; Abortion disease; Thrombophilia
Introduction
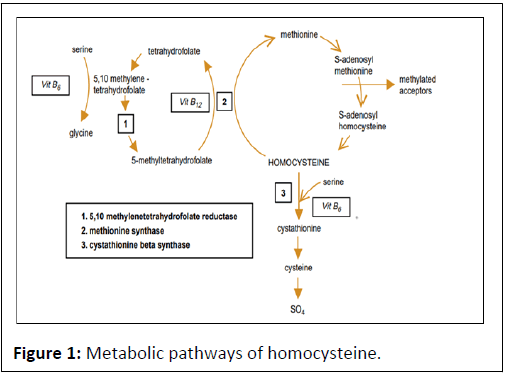
Homocysteine is a sulfur amino acid which is an intermediate step in the cellular metabolism of the essential amino acid methionine. However, most homocysteines are remethylated to methionine. It is by an enzymatic route of synthesis of SAdenosylmethionine, a major methyl donor involved in numerous biochemical reactions (DNA, protein, neurotransmitter, hormone, synthesis of phospholipids, etc.) (Figure 1). Mutation of the MTHFR gene is linked to elevated expressions of total homocysteine, especially in women with folic acid deficiency [1]. Polymorphism of the MTHFR gene is a major cause of hyperhomocysteinemia [2]. Folic acid along with vitamins B12 and B6 have a strong impact on the functionality of Hct [3]. Many factors cause hyperhomocysteinemia, including genetic abnormalities, folic acid deficiency, vitamin B6 and B12 deficiency, hypothyroidism, medications, aging and kidney dysfunction [4]. Increased peripheral blood homocysteine can lead to vascular disease [5], coronary artery dysfunction, atherosclerotic changes [5] and embolic disease [6]. The Hct level is lower during pregnancy compared to its normal values [7]. The Hct dosage tends to drop in the first trimester; it reaches its lowest value during the second trimester; thereafter, it increases steadily at the end of pregnancy until it reaches the level at the beginning of pregnancy [8]. Hyperhomocysteinemia reduces the nitric oxide released by the vascular endothelium, which will cause the formation of thrombosis, which in turn will affect placental perfusion, consequently it can have an impact on pregnancy; and may be responsible for an abortive disease, preeclampsia, threat of premature delivery, retroplacental hematoma, intrauterine growth restriction [9]. The aim of this review is to address the importance of the search for hyperhomocysteinemia and its complications in pregnant women by reporting the case of a patient with a history of abortive disease that carried a pregnancy to term after folic acid supplementation and put on anticoagulant.
Observation and Clinical Case
36-year-old female patient, group a positive, with a history of abortive disease with 7 spontaneous unaspirated and uncuretted fossae in the first trimester and a delivery by high route at 7 months for retroplacental hematoma in a context of preeclampsia of a newborn died on day 2 of life for respiratory distress. During the follow-up of her abortive disease, the patient benefited from a complete assessment having objectified a hyperhomocysteinemia without other biological anomaly; she consulted in our training with a ninth pregnancy estimated at 12 weeks of amenorrhea where an ultrasound was performed showing an evolving monofetal pregnancy corresponding to the gestational age without trophoblastic detachment. The patient was seen in prenatal consultation on a monthly basis and was placed throughout the pregnancy on a progestogen associated with an antiplatelet agent with heparin therapy based on lovenox 0.4 per day associated with vitamin supplementation.A prenatal check-up was requested having objectified gestational diabetes on OGTT at 75 g, hence his diet alone with correct glycemic cycles. Knowing that the patient kept correct tendon figures throughout the pregnancy without significant uterine bleeding a prophylactic cesarean section was scheduled at 39 weeks of amenorrhea. The clinical examination on the day of the upper route objectified a patient in good condition general normotensive afebrile correct uterine height at 32 cm speculum examination showed a healthy-looking cervix with no noticeable bleeding. The high prophylactic way allowed the cephalic extraction of a newborn male with an apgar score of 10 births weight 3200 grams received by the pediatrician. The suites are simple for the mother and the newborn.
Results and Discussion
Although the mechanisms of the vascular changes associated with hypermocysteinemia are not yet fully understood, animal studies have allowed us to provide specific details [10]. In the case of endothelial changes, the effects occur mainly at the level of the vessel wall [11]. The lesions observed consist of vascular fibrosis and endothelial cell dysfunction. Vascular endothelia are prone to vacuolation and desquamation, exposing subendothelial tissue and activating thrombus formation. Homocysteine decreases in the first trimester of pregnancy, reaches a minimum in the second trimester and increases somewhat to baseline levels during term [12]. Therefore, finding homocysteine during pregnancy is difficult. On the other hand, it is possible to look for mutations in the CBS or MTHFR genes during pregnancy.
Hereditary thrombophilias and hyperhomocysteinemia, or a combination of the two, may be responsible for recurrent fossa, with a genetic susceptibility to venous thrombosis [13]. A third of abortive diseases are due to hyperhomocysteinemia, as is the case in our patient. A deficiency in vitamin D and folate could raise the level of homocysteine by reducing the enzyme involved in its metabolism. The MTHFR genotype can double or triple the morbidity of fetal loss [14]. Maternal genetic mutations cause embolic kidney disease or heart disease. However, it may not have the same adverse effects on placental circulation in early pregnancy [9]. Quere reports the case of a patient who had 2 fetal losses at 28 and 26 weeks of amenorrhea and three early miscarriages, the only abnormalities of the etiological assessment were hyperhomocysteinemia and the mutation of the MTHFR gene [15]. A prescription of folic acid and vitamin B6 during subsequent pregnancies allowed this patient to have a living child and this is almost the case with our patient who was able to carry a pregnancy to term after having had seven fetal loss.
Recent studies have reported that homocysteine expression levels in women with preeclampsia are increased compared to normotensive pregnant patients [16]. However, a significant difference in its levels between patients with PE and nonpregnant women was not found, implying hyperhomocysteinemia in PE is the change in blood volume rather than at a mutation of the MTHFR gene [17]. Several studies aim to determine whether hyperhomocysteinemia can be used to predict the risk of preeclampsia [18]. Elevated homocysteine levels have been detected during the first or second trimester of pregnancy without being directly implicated in preeclampsia. The reason for the high level of homocysteine in early pregnancy could be due to the alteration of vascular endothelial cells in early pregnancy. As this lesion worsens thus causing placental ischemia, eventually leading to preeclampsia [19]. On the other hand, the level of expression of homocysteine during the second trimester does not help to predict the risk of preeclampsia in pregnant women with chronic hypertension [20]. Homocysteine levels in patients with retroplacental hematoma were significantly higher than in patients with normal pregnancies [21]. A comparative retrospective case-control study of patients with retro-placental hematoma compared to other patients who had normal pregnancies without signs or symptoms of metrorrhagia showed an increase in homocysteine levels in patients with retroplacental hematoma [22]. However, in other studies, the authors revealed that hyperhomocysteinemia was not necessarily associated with retroplacental hematoma [23]. In our patient, the intentional figures were correct throughout the pregnancy with no signs of detectable abnormal bleeding.
Among the actions of homocysteine on endothelial cells is vascular obstruction, which can be the cause of premature labor. However, the prevalence of decidual angiopathy is not significantly related to preterm delivery [24]. An association between neurological malformations and hyperhomocysteinemia has been described in the literature [25]. In fact, AFTN is not due to a direct effect of homocysteine, but to a dysfunction of Methionine Synthase (MS), a key enzyme in remethylation and also involved in the synthesis of the basic protein of the myelin.
Hyperhomocysteinemia can impact the transfer of amino acids into the placenta, which could cause intrauterine growth restriction [26]. Some authors reveal that compared to normal pregnancies, homocysteine levels are higher in patients who have had pregnancies with intrauterine growth restriction [27], this could be due to damage to endothelial cells which can cause impaired uterine and placental blood circulation. In our patient who carried a pregnancy to term, the birth weight was eutrophic; it seems premature to retain a direct impact of hyperhomocysteinemia on fetal growth.
Hyperhomocysteinemia is a congenital thrombophilia, just like antithrombin, protein C, or protein S deficiency, resistance to activated protein C (due to Leiden mutations of the V gene) and factor II mutations [28]. Pregnancy itself is a risk factor for thrombosis. Therefore, the association between hyperhomocys teinemia and pregnancy represents a high thromboembolic risk situation. The prescription of anticoagulants in addition to vitamin therapy to patients is even advised once congenital thrombotic tendencies have been identified. This prophylaxis consisted in our case of treatment with calciparin at the start of pregnancy, low molecular weight heparin at the end of pregnancy, then resumption of calciparin at the end of pregnancy, during delivery and 1 month after delivery.
Conclusion
Homocysteine activity during normal pregnancies and its impact is a widely debated topic. According to the literature, homocysteine levels are not constant during pregnancy. Genetic polymorphisms associated with hyperhomocysteinemia and their metabolisms are clearly associated with complications during pregnancy. However, clinical trials aiming to show this require a lot of resources. High-dose folic acid supplementation during pregnancy may help women with complications from hyperhomocysteinemia.
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Yamada K, Chen Z, Rozen R, Matthews RG (2001) Effects of common polymorphisms on the properties of recombinant human methylenetetrahydrofolate reductase. Proc Natl Acad Sci USA 98: 14853-14858.
[Crossref], [Google Scholar], [Indexed]
- Long S, Goldblatt J (2016) MTHFR genetic testing: Controversy and clinical significance. Aust Fam Physician 45: 237-240.
[Google Scholar], [Indexed]
- Refsum H (2001) Folate, vitamin B12 and homocysteine in relation to birth defects and pregnancy outcome. Br J Nutr 85: S109-S113.
[Google Scholar], [Indexed]
- Alvares Delfino VD, De Andrade Vianna AC, Mocelin AJ, Barbosa DS, Mise RA, et al. (2007) Folic acid therapy reduces plasma homocysteine levels and improves plasma antioxidant capacity in hemodialysis patients. Nutrition 23: 242-247.
[Crossref], [Google Scholar], [Indexed]
- Graham IM, Daly LE, Refsum HM, Robinson K, Brattstrom LE, et al. (1997) Plasma homocysteine as a risk factor for vascular disease: The european cooperative action project. JAMA 277: 1775-1781.
[Crossref], [Google Scholar], [Indexed]
- Den Heijer M, Koster T, Blom HJ, Bos GM, Briet E, et al. (1996) Hyperhomocysteinemia as a risk factor for deep vein thrombosis. N Engl J Med 334: 759–762.
[Crossref], [Google Scholar], [Indexed]
- Cicott RJLM, Stegers-Theunissen RP, Thomas CM, De Boo TM, Mercus HM, et al. (2001) Longitudinal vitamin and homocysteine levels in normal pregnancy. Br J Nutr 85: 49-58.
[Crossref], [Google Scholar], [Indexed]
- Walker MC, Smith GN, Perkins SL, Keeley EJ, Garner PR (1999) Changes in homocysteine levels during normal pregnancy. Am J Obstet Gynecol 180: 660-664.
[Crossref], [Google Scholar], [Indexed]
- Zammiti W, Mtiraoui N, Mahjoub T (2008) Lack of consistent association between endothelial nitric oxide synthase gene polymorphisms, homocysteine levels and recurrent miscarriages in Tunisian women. Am J Reprod Immunol 59: 139-145.
[Crossref], [Google Scholar], [Indexed]
- Wilken DEL, Dudman NPB (1989) Mechanisms of thrombus formation and accelerated atherogenesis in homocysteinemia. Hemostasis 19: 14-23.
[Crossref], [Google Scholar], [Indexed]
- Woo KS, Chook P, Lolin YI, Cheung ASP, Chan LT, et al. (1997) Hyperhomocystinemia is a risk factor for arterial endothelial dysfunction in humans. Circulation 96: 2542-2544.
[Crossref], [Google Scholar], [Indexed]
- Walker MC, Smith GN, Perkins SL, Keely EJ, Garner PR (1999) Changes in homocysteine levels during normal pregnancy. Am J Obstet Gynecol 180: 660-664.
[Crossref], [Google Scholar], [Indexed]
- Raziel A, Friedler S, Schachter M, Ron-El R, Kornberg Y, et al. (2003) Hypercoagulable thrombophilic defects and hyperhomocysteinemia in patients with recurrent pregnancy loss. Am J Reprod Immunol 45: 65-71.
- Nellen WL, Stegers EA, Eskes TK, Blom HJ (1997) Genetic risk factors for recurrent early miscarriage of unknown cause. Lancet 350: 861.
[Crossref], [Google Scholar], [Indexed]
- Quere I, Bellet H, Hoffet M, Janbon C, Mares P, et al. (1998) Women with five consecutive fetal deaths: Case report and retrospective analysis of the prevalence of hyperhomocysteinemia in her 100 consecutive women with repeated miscarriages. Fertil Steril 69: 152-154.
- Sanlikan F, Tufan F, Göçmen A, Kabadayi C, Sengül E (2015) The evaluation of homocysteine level in patients with preeclampsia. Ginekol Pol 86: 287-291.
- Ligemakers MT, Zusterzeel PL, Steegers EA, Peters WH (2001) Hyperhomocysteinemia: A risk factor for pre-eclampsia? Eur J Obstet Gynecol Reprod Biol 95: 226-228.
[Crossref], [Google Scholar], [Indexed]
- Hogg BB, Tamura T, Johnston KE, Dubard MB, Goldenberg RL (2000) Second-trimester plasma homocysteine levels and pregnancy-induced hypertension, preeclampsia and intrauterine growth restriction in the second trimester. Am J Obstet Gynecol 183: 805–809.
[Crossref], [Google Scholar], [Indexed]
- Sun F, Qian W, Zhang C, Fan JX, Huang HF (2017) Correlation between maternal serum homocysteine in early pregnancy and development of gestational hypertension and preeclampsia. Med Sci Monit 23: 5396-5401.
[Crossref], [Google Scholar], [Indexed]
- Zeeman GG, Alexander JM, McIntire DD, Devaraj S, Leveno KJ (2003) Homocysteine plasma concentration levels for the prediction of preeclampsia in women with chronic hypertension. Am J Obstet Gynecol 189: 574-576.
- Godin Wessel TA, Wouters MG, Molen EFVD, Spuijbroek MDEH, Theunissen RPMS, et al. (1996) Hyperhomocysteinemia: Placental abruption or heart attack risk factors. Eur J Obstet Gynecol Reprod Biol 66: 23-29.
[Crossref], [Google Scholar], [Indexed]
- Budde MP, De Lange TE, Dekker GA, Chan A, Nguyen AM (2007) Risk factors for placental abruption in socioeconomically disadvantaged region. J Matern Fetal Neonatal Med 20: 687-93.
[Crossref], [Google Scholar], [Indexed]
- Chaudhry SH, Taljaard M, MacFarlane AJ, Gaudet LM, Smith GN, et al. (2019) The role of maternal homocysteine concentration in placenta-mediated complications: Findings from the Ottawa and Kingston birth cohort. BMC Pregnancy Childbirth 19: 75.
- Kramer MS, Kahn SR, Rozen R, Evans R, Platt RW, et al. (2009) Vasculopathic and thrombophilic risk factors for spontaneous preterm birth. Int J Epidemiol 38:715-723.
- D'Anna R, Baviera G, Corrado F, Ientile R, Granese D, et al. (2004) Plasma homocysteine in early and late pregnancy with preeclampsia and isolated intrauterine growth restriction. Acta Obstet Gynecol Scand 83:155–158.
[Crossref], [Google Scholar], [Indexed]
- Tsitsiou E, Sibley CP, D'Souza SW, Catanescu O, Jacobsen D (2009) Homocysteine transport by systems L, A and y+L across the microvillous plasma membrane of human placenta. J Physiol 587: 4001-4013.
[Crossref]
- Furness D, Fenech M, Dekker G, Khong TY, Roberts C, et al. (2013) Folate, vitamin B12, vitamin B6 and homocysteine: Impact on pregnancy outcome. Matern Child Nutr 9: 155-166.
- Rao AK, Kaplan R, Sheth S (1998) Inherited thrombotic conditions. Semin Thromb Hemost 24: 3-12.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences