Huriez a Squamous Cell Carcinoma Prone Syndrome: A Case Report
Hala Halbony1*, Mehmet Bekerecioglu1 and Sezen Kocarslan2
1Department of Plastic Reconstructive and Aesthetic Surgery, Kahramanmaras Sutcu Imam University, Kahramanmaras, Turkey.
2Department of Clinical Pathology, Kahramanmaras Sutcu Imam University, Kahramanmaras, Turkey.
- *Corresponding Author:
- Hala HalbonyDepartment of Plastic Reconstructive and Aesthetic Surgery, Kahramanmaras Sutcu Imam University, Kahramanmaras, Turkey, E-mail: hala.halbouni@yahoo.com
Received date: May 2, 2022, Manuscript No. IPMCRS-22-13585; Editor Assigned date: May 3, 2022, PreQC No. IPMCRS-22-13585 (PQ); Reviewed date: May 18, 2022, QC No. IPMCRS-22-13585; Revised date: May 24, 2022, Manuscript No. IPMCRS-22-13585 (R); Published date: June 1, 2022, DOI: 10.36648/2471-8041.8.6.229
Citation: Halbony H, Bekerecioglu M, Kocarslan S (2022) Huriez a Squamous Cell Carcinoma Prone Syndrome: A Case Report. Med Case Rep Vol.8 No.6: 229.
Abstract
This report is to describe a case of a rare autosomal dominant genodermatosis known as Huriez syndrome in a 41 year-old female patient presenting with recurrent skin lesions. Following investigations, the patient was diagnosed to have Huriez syndrome. She was planned for excision and follow up in the plastic surgery, dermatology and oncology departments.
Huriez syndrome, also known as ‘sclerotylosis’ a rare autosomal dominant genodermatosis which has been first reported in France by Huriez et al. later it has been reported in India, Japan, Tunisia Germany, Ä°taly and Turkey.
Introduction
Huriez syndrome, also known as ‘sclerotylosis’ a rare autosomal dominant genodermatosis which has been first reported in France by Huriez et al. later it has been reported in India, Japan, Tunisia Germany, İtaly and Turkey [1-5].
The syndrome manifests as scleroatrophy of distal extremities, hypoplastic nails palmoplantar keratoderma and an increased risk of the development of Squamous Cell Carcinoma (SCC) [4]. In the case of the development of SCC it is featured by an early onset mostly in 3rd to 4th decades of life, and a more aggressive behavior [5].
Case Presentation
The patients history dates first to 13 years prior to her last visit, when she first presented to the dermatology clinic of Kahramanmaraş Sutcu Imam University Hospital, Kahramanmaras-Turkey, complaining of brown discolored macular lesions as well as hyperkeratotic squamous erosions in the face and on the plantar aspect of the foot, the patient was prescribed PREDNOL-A cream as well as sunblock. Two months later the patient visited the dermatology clinic for the same complaint where she was prescribed salisilic acid, vaseline, flurokortolone caproate, balmandol oil and a urea based lotion. 11 years later the patent was referred from a Private clinic to KSÜ Dermatology clinic with a 3*4 cm lesion in the medial aspect of the right foot suspicious of Bowen disease on punch biopsy. Cardiology consultation was requested and no cardiologic pathology was found. The patient got referred to the department of plastic Surgery in KSÜ hospital for potential excision and tissue defect closure.
The lesion was excised with a 1 cm margin and the defect was closed by a split thickness skin graft from the anteriolateral aspect of the right things.
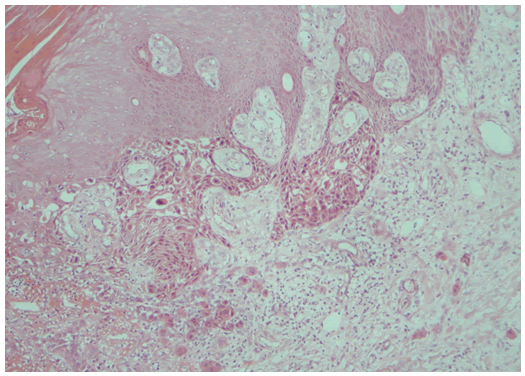
The pathological diagnosis of the lesion was squamous cell carcinoma with lesions of squamous cell in situ the margin were tumor free, perineural and intraneural invasion was present, however lymphovascular invasion was absent as shown in Figure 3, following the epithelialization of the wound the patient was referred to oncology department for follow-up.
2 years later the patient visited the dermatology clinic with chief complaint of fissures in her right hand, the patient was referred to the plastic surgery department for diagnostic excision.
The lesion was excised with a 1 cm margin and the defect was closed by a full thickness skin graft from the left arm.
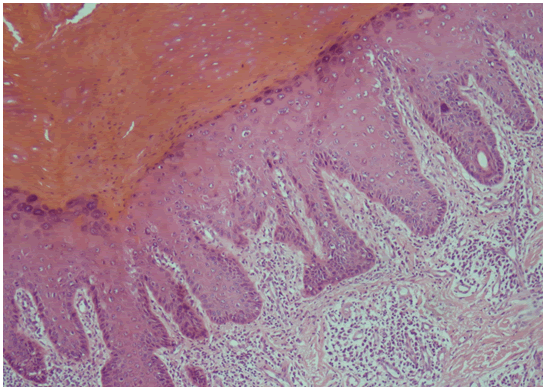
The pathological report revealed focal regions of mild-moderate degrees of dysplasia in the squamous epithelium with severe, chronic inflammation in the dermis as shown in Figure 3. Surgical margins were negative, there was no invasion detected for the diagnosis of carcinoma P53 was sparse positive, Kİ 67 was positive in the basal layer.
Following the epithelialization of the wound the patient was referred to on oncology department for follow up.
Cantella asiatica cream, salisilic acid based cream, olive oil, hyaluronic acid based cream, vaseline and urea based cream were prescribed by the dermatology clinic.
The patient is a result of a second degree consanguinal marriage and her Sister suffers from similar but milder symptoms.
Laboratory investigations revealed vitamin D deficiency, iron deficiency, hypothyroidism, Anti DS DNA, ANA, Anti-scl70, and Anti ssDNA were negative (Figures 1-4).
Results and Discussion
Huriez syndrome is a rare autosomal dominant genodermatosis characterized by a triad of congenital scleroatrophy of distal extremities, Palmoplantar Keratoderma (PPK) and hypoplastic nails [2,3]. Chromosomal locus of Huriez syndrome has been found to be on the 10.5-Mbregion on chromosome 4q [4]. Haploinsufficiency of the Skin specific SMARCAD 1 isoform accounts for this syndrome. SMARCAD1 has two isoforms; the long isoform has been shown to have a role in the 5’-3’ resection of DNA ends which initiate the high-fidelity homologous recombination repair of DNA double stranded breaks. The short isoform has two CUE1 domains which are absent in Huriez syndrome, these domains take part in the recruitment of DNA repair factors.
The histopathology of the skin in Huriez syndrome is nonspecific and includes epidermal atrophy demal hypervascularity, sparse lymphocytic infiltrate as well as pigment laden macrophages [2]. Patients with Huriez syndrome have a more than 100 fold increased risk for the development of SCC, where SCC arises in alound 15% of patients with Huriez syndrome. Moreover SCC in Huriez syndrome is characterized by its early onset and aggressive behavior [3].
Pathological P53 staining of atypical keratinocytes suggest a positive correlation of P53 mutation and the development of SCC in Hureiz syndrome.
The differential diagnosis includes scleroderma and dyskeratosis congenita. Topical emollients, keratolytics as well as oral and topical retinoids can be used in the treatment.
Conclusion
Huriez syndrome must be always considered in the differential diagnosis of patients presenting with scleroatrophy of the distal extremities. High level of suspicion of SCC is essential for proper and early treatment to prevent devastating consequences of the aggressive disease. Therefore a multidisciplinary team of Plastic Surgeons, dermatologists, geneticists and oncologists is vital in the treatment.
No genetic studies were performed in our case and this was the limitation in our study.
Clinical phenotype, tumor risk in patients can be modified by environmental exposures, ethnic differences or modifier gene [4,6].
References
- Surana T, Padhiar B, Karia U, Pandya P (2016) Huriez syndrome with superadded dermatophyte infection. Indian Dermatol Online J 7: 288-9.
[Crossref], [Google Scholar], [Indexed]
- Kharge P, Fernendes C, Jairath V, Mohan M, Chandra S (2015) Poikiloderma a varied presentation-Huriez syndrome. Indian Dermatol Online J 6: 27-30.
[Crossref], [Google Scholar], [Indexed]
- Çelik NS, Yaşar Ş, Aytekin S, Güneş P (2018) A rare syndrome resembling scleroderma: Huriez syndrome. Skin Appendage Disord 4: 82-85.
[Crossref], [Google Scholar], [Indexed]
- Günther C, Lee-Kirsch MA, Eckhard J, Matanovic A, Kerscher T, et al. (2018) SMARCAD1 haploinsufficiency underlies huriez syndrome and associated skin cancer susceptibility. J Invest Dermatol 138:1428-1431.
[Crossref], [Google Scholar], [Indexed]
- Cohen PR, Jiang SB (2017) Finger pad squamous cell carcinoma: Report of squamous cell carcinoma of the distal palmar digit and review of associated risk factors, mimickers, and treatment of squamous cell carcinoma of ventral hand digits. J Clin Aesth Dermatol 10: 42-48.
[Crossref], [Google Scholar], [Indexed]
- Tadlaoui I, Qasmi S, Belgnaoui F, Bouhllab J, Afifi Y, et al. (2008) Syndrome d'Huriez compliqué d'un carcinome épidermoïde
(Squamous cell carcinoma in Huriez syndrome). Ann Dermatol Venereol 135: 249-50.[Crossref], [Google Scholar]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences