Hemoglobinosis D-Punjab in a Moroccan Family
Hanaa Bencharef*, Aya Rachidi and Bouchra Oukkache
Department of Medicine and Pharmacy of Casablanca Centre for Clinical & Diagnostic Oral Sciences, IBN Rochd University Hospital Center, Casablanca, Morocco
- *Corresponding Author:
- Hanaa Bencharef
Department of Medicine and Pharmacy of Casablanca Centre for Clinical & Diagnostic Oral Sciences ,IBN Rochd University Hospital Center, Casablanca, Morocco
Tel: 2126607650 00
E-mail: hanaa.bencharef@gmail.com
Received Date: December 27, 2021; Accepted Date: January 10, 2022; Published Date: January 17, 2022
Citation: Bencharef H, Rachidi A, Oukkache B (2022) Hemoglobinosis D-Punjab in a Moroccan Family. Med Case Rep Vol.8 No.2
Abstract
Background: Hemoglobinosis D, also called Hemoglobinosis Los Angeles or Punjab, is a structural variant derived from a point mutation of the beta-globin (HBB) gene in the first base of codon 121 (GAA → CAA) with the substitution of glutamine for glutamic acid (Glu> Gln) in the beta globin chain. It’s transmitted in autosomal recessive mode and occurs in different forms including heterozygous hbD trait.
Hemoglobinosis D is widespread worldwide, with dominance in the Punjab region of the northwest of India, unlike Morocco where it’s still very rare and poorly studied.
Case Report
We describe the first case of heterozygous HbD-Punjab in a Moroccan family, discovered following microcytic hypochromic anemia in a 6 years old child.
Conclusion
This case highlights the possibility of the appearance of rare phenotypes within our multiethnic population, and emphasizes the importance of precise genetic studies to plan genetic counseling and allow effective patient management before the onset of any complications.
Keywords
Heterozygous hemoglobinopathy; Hemoglobinosis D-Punjab; Moroccan family
Introduction
Mutations in genes encoding globin chains affect approximately 7% of the population around the world [1]. There are several variants of hemoglobin over 1000 variants, according to the globin gene server database [2]. Most of these variants are asymptomatic, but in some cases, they can have considerable clinical disorders [3].
Hemoglobinosis D-Punjab, also called hemoglobinosis D-Los Angeles, is one of those variants. It’s a structural variant of hemoglobin, caused by a point mutation, at the codon 121 of the beta-globin gene (HBB), which causes a substitution of glutamic acid by glutamine at position 121 of the hemoglobin chain [3,4].
This hemoglobinopathy is transmitted in autosomal recessive mode [3,5].
Hemoglobinosis D occurs in different forms including heterozygous hbD trait, hemoglobin D-B thalassemia association, and hemoglobin SD, and more rarely homozygous hbD disease [6,7].
The heterozygous form is clinically silent, on the other hand, the homozygous form, can be associated with a mild hemolytic anemia, and a mild or moderate splenomegaly [8,9].
Hemoglobinosis D is widespread worldwide, with dominance in the northwest of India, especially in Punjab and in Gujarat, with a prevalence of 1% to 3% [10,11].
In the Maghreb and especially in Morocco, the most frequent hemoglobin variants are hemoglobin S and C, contrary to hemoglobin D which is rarer [12,13].
We describe the first case of heterozygous HbD-Punjab in a Moroccan family, discovered following microcytic hypochromic anemia in a 6 years old child, and diagnosed in our laboratory of hematology laboratory. This case highlights the possibility of the appearance of rare phenotypes within our multiethnic population, and emphasizes the importance of precise genetic studies to plan genetic counseling and allow effective patient management before the onset of any complications.
Case Report
It is about a child of Moroccan origin, aged 6 years, without concept of consanguinity in the parents, who was referred to us for the exploration of a microcytic hypochromic anemia with normal ferritinemia, the clinical signs were cutaneo-mucous pallor associated with chronic asthenia.
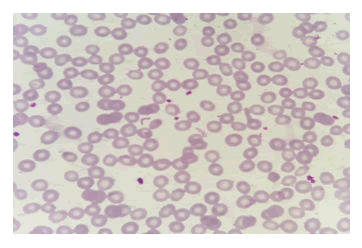
Red cell indices at the hospital revealed the following: Hb 9 g/dL, RBC 2.98 X106/uL, MCV 73fL, andMCHC30.9g/dL.Bloodsmearshowedmarkedanisopoikilocytosiswithmicrocytichypochromic red cells, without any sickle and boat shaped cells (Figure 1).
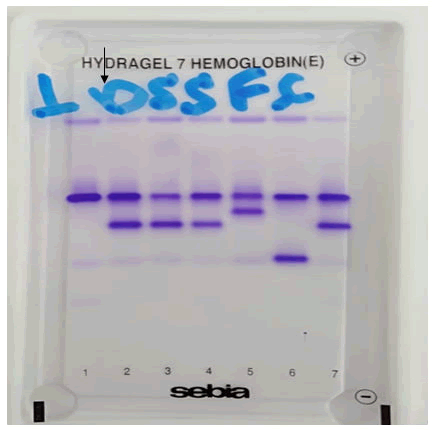
The Hemoglobin (Hb) electrophoresis done at pH 8.5 showed a variant band at hemoglobin S position (Figure 2).
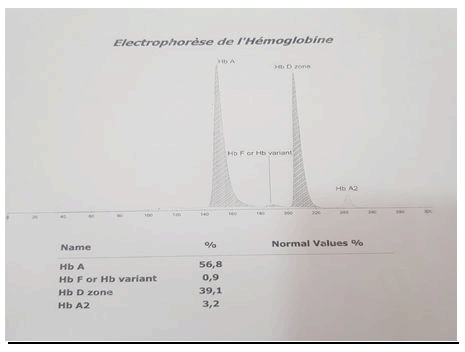
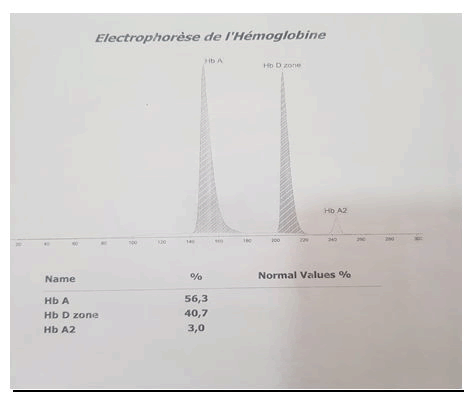
Further analysis on High Performance Liquid Chromatography (HPLC) showed presence of Hb D variant at 39,1% also checked by capillary electrophoresis (Figure 3). Based on this result, the diagnosis of heterozygous hemoglobin D-Punjab was made, and a family survey was carried out. The parent’s blood samples were sent to our institute for testing, objectifying a normal profile of hemoglobin electrophoresis in the mother and the presence of 40.7% of HbD in the father of the child; therefore we were able to fully determine the pattern of inheritance (Figure 4).
Discussion
Hb D Punjab is prevalent in the northwest of India, especially in Punjab and in Gujarat regions, due to consanguineous marriages, with an estimated frequency of 1% to 3% [7,10]. Its homozygous form is very rare and only few cases are described [9]. On the other hand, the Hb D trait is more frequent, and usually asymptomatic, but a slight anemia can be seen as well as morphologic abnormalities in the blood smear; including anisopoikilocytosis [13], which corresponds to the data of our study, therefore, the resultants of the blood count must be taken into account. Hemoglobin D may also be associated with hemoglobin S or thalassemia [2,4].
The study of hemoglobin in the laboratory, use several phenotypic and possibly genotypic techniques. Phenotypic diagnosis is based on electrophoretic and chromatographic techniques; mainly gel electrophoresis, high performance liquid chromatography and capillary electrophoresis [13,14].
In hemoglobin electrophoresis, Hb S and Hb D migrate at the same level at alkaline ph 8.5. However, they can be separated by electrophoresis on agar gel at acidic pH 6.2 [6,14,15]. High Performance Liquid Chromatography (HPLC) methods have highly sensitivity and specificity. It consists of the separation of the different hemoglobin fractions and the identification of their relative percentage. It allows provisional identification of many other variants types of hemoglobins that cannot be distinguished, by conventional gel electrophoresis [1].
In capillary electrophoresis, different hemoglobin’s are separated in different areas. The most common hemoglobin variants, including Hb D-Punjab, migrate separately from hemoglobin A2, giving a peak in zone 6 and therefore do not interfere in its quantification [14].
In the homozygous Hb D disease, the Hb D is about 80% to 90%, in the heterozygous Hb D trait, the Hb D is about 30% to 40% [16]. This was the case with our patient with a percentage of Hb D at 39.1%.
Hereditary character is proven in our study, since the father of the child also presents a heterozygous form of Hb D. However, for lack of resources, the genetic study was not done in our case.
The present case, underlines the rarity of this type of hemoglobinopathy and especially the difficulty of it’s diagnosis, which calls for several techniques allowing a phenotypic exploration, to which a genotypic analysis must necessarily be associated for better patient care.
It is necessary to make the nursing staff aware of the possibility of the existence of this type of hemoglobinopathy in our context, and to institute genetic counseling before marriage in order to make an early diagnosis of some hemoglobinopathies, the complications of which are serious especially in their homozygous form.
Conclusion
Due to migration, the Hb D-Punjab is relatively widespread in the world, However, it’s remains extremely rare in Moroccan family and not documented in the literature. The diagnosis of this hemoglobinopathy, can be difficult, especially in asymptomatic cases, and it uses a variety of tests, including a phenotypic exploration with electrophoretic techniques and chromatography as well as a genetic study.
Acknowledgements
We have no acknowledgements.
Conflict of Interests
The authors declare that they have no competing interests.
References
- Torres LD, Okumura JV, Silva DG, Bonini-Domingos CR (2015) Hemoglobin D-Punjab: origin, distribution and laboratory diagnosis. Revista brasileira de hematologia e hemoterapia 37:120-126
- Aslan D (2020) Is Hemoglobin D Trait Hematologically Silent: Comparison With Healthy Controls and β-thalassemia Carriers. JOPHON 42:698-701
- Dasgupta A, Wahed A (2014) Hemoglobinopathy. Clinical Chemistry, Immunology and Laboratory Quality Control
- Mukherjee MB, Surve RR, Gangakhedkar RR, Mohanty D, Colah RB. Case Report-Hemoglobin sickle D Punjab—a case report.
- Kohne E (2011) Hemoglobinopathies:Clinical Manifestations, Diagnosis, and Treatment. Dtsch Arztebl Int 108: 532–540
- Gupta S, Kapoor AK (2016) Detection of Hemoglobin D in Tharu Community of Banke, Nepal. JNGMC 14:24-26
- Biswas TK, Pillai A (2019) Hemoglobin-D Punjab—rare hemolytic anemia in the elderly: a case report. MGMJMS 6:148
- Pandey S, Mishra RM, Pandey S, Shah V, Saxena R (2012) Molecular characterization of hemoglobin D Punjab traits and clinical-hematological profile of the patients. Sao Paulo Med J 130:248-251
- Pandey S, Ranjan R, Seth T, Saha V, Mishra RM, et al. (2012) Clinical-hematological profile of Indian hemoglobin sickle cell D Punjab patients. Sao Paulo Med J 130:248-251
- Dolai TK, Bera R, Maji SK, Mandal PK (2014) Profile of hemoglobin D trait in West Bengal, India. Thalassemia Reports 4
- [11] Patel KD (2019) Variants of Hemoglobin D Punjab - A Retrospective Study. Saudi J Pathol Microbiol 4: 507-511
- Saoud MZ, Biaz A, Rachid A (2019) Hémoglobinose D-Punjab chez une famille de Zaër, Poster· JIRR BIO010
- Saoud MZ, Biaz A, Rachid A, El Amin G, Dami A, et al. (2020) Association d’hémoglobinose D-Punjab et de β-thalassémie dans une famille marocaine. InAnnales de Biologie Clinique 78:61-69
- Baudin B (2016) Les hemoglobines normales et pathologiques. Revue Francophone des laboratoires 481
- Ahmad R, Omar SL, Arif SH, Hamid FS, Aziz NA, et al. (2014) Mustapha NH, Zakaria Z. Haemoglobin sickle d punjab:-a case report. Med J Malaysia 69
- Srinivas U, Pati HP, Saxena R (2010) Hemoglobin D-Punjab syndromes in India: a single center experience on cation-exchange high performance liquid chromatography. Hematology15:178-181

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences