Epiphora: Successful Response to Systemic Steroids vs Topical Steroids
Ali Arif* and Humara Gull
DOI10.36648/2471-8041.21.7.197
1Department of Internal Medicine, 2nd year Northeast Ohio Medical University Student, USA
2Department of Internal Medicine and Primary Care, IMD Healthcare and Imaging, Kingwood, USA
- *Corresponding Author:
Received: August 30, 2021; Accepted: August 13, 2021; Published: September 20, 2021
Citation: Arif A and Gull H (2021) Epiphora: Successful Response to Systemic Steroids vs Topical Steroids. Med Case Rep Vol.7 No.8.197
Abstract
Purpose: Topical steroids are considered to be the first line of treatment for some forms of idiopathic punctal stenosis causing epiphora. We present a case of epiphora, which was unresponsive to the traditional management, but responded to one week of systemic steroids.
Observations: 48 year old male with no significant past medical history was referred for excessive tearing. Earlier, an ophthalmologist had prescribed Pataday and Zylet eye drops for both eyes after the patient complained about eye redness unilaterally. After a week without much improvement, Alrex and Azasite eye drops replaced them. Eye redness disappeared within a week, the patient then complained of excessive tearing. He was referred to a reconstructive ophthalmologist for treatment of possible punctal stenosis. On examination, the height of tear meniscus was increased, and diagnostic lacrimal probing of the lacrimal drainage system demonstrated both lacrimal drainage systems patent. Punctal stenosis was diagnosed. Over the next few weeks, patient underwent multiple syringing of the lacrimal duct system with temporary relief of symptoms. Tobradex was also prescribed for a month. Eye drops helped for the duration of treatment, but symptoms returned within a few days of discontinuation. However, intra ocular pressure began rising with Tobradex eye drops, so they were discontinued immediately. After three months of treatment and continuation of debilitating symptoms of epiphora, patient considered surgical intervention and consulted an ENT for second opinion. The ENT surgeon suggested Medrol Pack (Prednisolone) for a week as the patient had responded to the topical steroids, which increased his intra-ocular pressure. After four days of treatment, patient’s symptoms disappeared. By the seventh day, his eyes were back to normal with complete disappearance of epiphora symptoms.
Conclusions and Importance: Systemic steroids can be beneficial in patients suffering from idiopathic/iatrogenic punctal stenosis unresponsive to topical steroids and conventional treatments.
Keywords
Epiphora; Punctal stenosis; Steroids; Nasolacrimal duct
Introduction
Severe epiphora can be a debilitating condition because it not only causes patient discomfort but also visual disturbance. The lacrimal system consists of the main lacrimal gland, the accessory lacrimal glands and the conjunctival epithelium, responsible for producing tears. Tears are spread over the surface of the eye by blinking to establish the precorneal tear film. Tears are then drained through nasolacrimal ducts, a canicular connection between conjunctiva and nasal cavity. About 90 percent of tears are reabsorbed through nasolacrimal duct mucosa and 10 percent drain into the floor of nasal cavity. Any imbalance between tear production and loss can result in epiphora. Most imbalances fall into the categories of punctal obstruction, canicular obstruction, nasolacrimal duct obstruction, poor pump function, lid malposition, and ocular surface disorders. Punctal stenosis is considered one of the most common causes of epiphora but the incidence is still unknown, ranging from 8% to 54.3% [1]. Old age is identified as the most common cause of punctal stenosis with a mean age at diagnosis of 69.4 [2]. Multiple causes of punctal stenosis and canicular obstruction have been reported including, inflammation, infection, topical and systemic medications, neoplastic conditions, systemic diseases, trauma, and idiopathic [1].
Case Report
A 48 year old male with no significant past medical history, was seen by his ophthalmologist for redness in one of his eyes, who prescribed Pataday (Olopatadine) eye drops and Zylet (Tobramycin, lotepriol) eye drops for both eyes. The patient returned after a week of treatment without much improvement. His treatment was changed to Alrex (loteprednol) and Azasite (Azithromycin) eye drops. The redness of the eye disappeared in a week but patient noticed excessive tearing of his eyes. He was referred to reconstructive ophthalmologist for further treatment of possible punctal stenosis. On examination patient’s VA was 20/20 in both eyes. IOP were within normal limits in both eyes. The height of tear meniscus was increased and diagnostic lacrimal probing and syringing of the lacrimal drainage system demonstrated that both sides were patent and draining. Mild form of MGD was considered and punctal stenosis was diagnosed. Over the next couple of weeks, patient underwent multiple syringing, but the symptoms kept returning after a couple of days of treatment. He was also prescribed Tobradex eye drops to be used for a month. Eye drops helped relieve the symptoms only for the duration of treatment and the symptoms came back after a couple of days of discontinuing eye drops. Patient also received ductal probing and punctal dilation in the office with temporary relief. Mini perforated plugs were placed in both puncta resulting again, in temporary relief. At the same time patient’s intra ocular pressure started to rise with c/o sensitivity to light. Tobradex eye drops were discontinued immediately. After almost three months of treatment and continuation of debilitating symptoms of epiphora, patient decided to consider DCR and consulted an ENT surgeon for second opinion. Since he was responding to topical steroids, which in turn were causing an increase in his intra ocular pressure, the ENT surgeon prescribed Medrol Pack (Prednisolone) to be taken for a week. Patient was symptom free after 4 days of treatment and by 7th day, his eyes were back to normal without any signs of epiphora.
Discussion
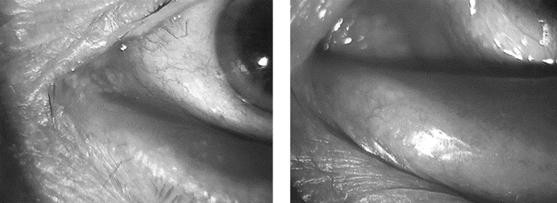
Punctal stenosis is considered one of the most common causes of epiphora but the incidence is still unknown, ranging from 8% to 54.3% [1]. Old age is identified as the most common cause of punctal stenosis with a mean age at diagnosis of 69.4 [2] Multiple other causes of punctal stenosis have been reported including, inflammation (Ch. Blepharitis, Ocular cicatricial pemphigoid, Graft vs host disease, Dry eye syndrome, Eye lid malposition), infection (Chlamydia trachomatis, Actinomyces, Herpes virus, Human papilloma virus), topical medications (Timolol, Latanoprost, Betaxolol, Dipivefrine hydrochloride, Echothiopate iodide, Pilocarpine, Prednisolone acetate-phenylephrine hydrochloride, Adrenaline, Chloramphenicol, Tobramycin, Indomethacin, Dexamethasone, Tropicamide, Naphazoline, Artificial tears, Mitomycin-C) systemic medications (5-Fluorouracil, Docetaxel, Piclitaxel, Idoxuridine, Trastuzumab emtansine) neoplastic (peripunctal tumors) systemic diseases (Acrodermatitis enteropathica, Porphyria cutanea tarda) other (local irradiation, photodynamic therapy for macular disease) trauma, and idiopathic [1]. The etiology in this case appears to be the reaction to one of the anti-allergy drops or topical antibiotics. As mentioned earlier, many medications including artificial tears can lead to this condition. This reaction was causing inflammation of the epithelial lining of the nasolacrimal drainage system, leading to obstruction. There were no signs of infection or any obstructive etiology. Instillation of topical steroid (combination of tobramycin and dexamethasone) was effective in providing symptomatic relief and quantitative decrease in of tear meniscus in this case. In literature, a study reported a 64% efficacy with topical steroids in nasolacrimal drainage obstruction [3]. Inflammation and edema of lacrimal drainage are the main pathological findings in the early phase of lacrimal drainage system stenosis [4], which can be reversed by anti-inflammatory treatment such as topical steroids. In addition, perforated punctal plugs have been used for punctal stenosis with good results [5]. Other options including mini-monoka stents and punctal snip procedures have also been reported for the treatment of refractory epiphora [6,7]. All these options were discussed with this patient (Figure 1). The appearance of symptoms in this patient was immediately after the use of topical medication (anti-allergy, antibiotic). It is possible that epiphora and lacrimal drainage stenosis in this case were coincidental findings induced by other etiologies such as blepharitis. However, no other possible etiologies such as infection, endogenous or exogenous inflammation, internal or external mechanical problems or trauma were detected in patient’s history or physical examination. In this case the diagnosis and subsequent treatment with topical steroids not only proved to be therapeutic but also diagnostic. Given the increase in IOP in this case and considering the long-term side effects of topical steroids including early cataract and glaucoma [8,9] it was prudent to give a trial of systemic steroids [10].
Laboratory tests showed a rise in cardiac enzymes, leukocyte count (16000 mm3), ESR, and CRP (135.5 mg/dl). Kidney and liver function with lipid profile and coagulation profile were normal. Results for syphilis (RPR and TPHA) were negative. Immunological markers, ANA and APLA were negative with low C3 levels.
Conclusion
Steroids have a long record of effective anti-inflammatory agent in many conditions. We believe that all the possible conservative management of lacrimal drainage stenosis including topical and systemic steroids (Medrol pack) should be exhausted before considering any surgical intervention.
Patient Consent
Consent to publish this case report has been obtained from the patient in writing.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgement
Thank you to Dr. Humara Gull for providing the opportunity to construct a case report and to the patient for their consent patient.
Conflict of Interest
The authors have no financial disclosures.
References
- Soibelman U, Kakizaki H, Selva D, Leibovitch I (2012) Punctal stenosis: Definition, diagnosis, and treatment: Review. Clinical Ophthalmology 6: 1011-1018.
- Kashkouli MB, Beigi B, Murthy R, Atsbury N (2003) Acquired external punctal stenosis: Etiology and associated findings. Am J Ophthalmol 136(6):1079-1089.
- Dayal Y (1962) Corticosteroids and Fibrolysin in the prevention of lacrimal duct obstruction. Br J Ophthalmol 46 (1)27-30.
- Linberg JV, McCormick SA (1986) Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology 93(8):1055-63.
- Konuk O, Urgancioglu B, Unal M (2008) Long-term success rate of perforated punctal plugs in the management of acquired punctal stenosis. Ophthal Plast Reconstr Surg 24(5):399-402.
- Kristan R, Branch L (1988) Treatment of lacrimal punctal stenosis with a one-snip canaliculotomy and temporal puntal plug. Arch Ophthalmol 106(7):878-879.
- Hussain RN, Kanani H, McMullan T (2012) Use of mini-monoka stents for punctal/canalicular stenosis. Br J Ophthalmol 96(5):671-673.
- Greiner JV, Chylack Jr LT (1979) Posterior subcapsular cataracts: histopathologic study of steroid-associated cataracts. Arch Ophthalmol 97(1):135-44.
- Razeghinejad MR, Katz LJ (2012) Steroid-induced iatrogenic glaucoma. Ophthalmic Res 47(2):66-80.
- P J Barnes (1998) Anti-inflammatory actions of glucocorticoids: Molecular mechanisms. Clin Sci (Lond) 94(6):557-72.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences