Does Topical Antifungal Treatment Plus Conventional Treatment Modality Improve Prognosis in Rhinoorbitocerebral Mucormycosis?
Tuba Bayindir1*, Sukru Aydin1, Mehmet Fatih Erbay2, Canan Ates Gurso3, Yuksel Toplu3 and Yasar Bayindir4
1Department of Otorhinolaryngology, Inonu University, Malatya, Turkey
2Department of Radiology, Inonu University, Malatya, Turkey
3Department of Medical Microbiology, Inonu University, Malatya, Turkey
4Department of Infectious Diseases and Clinical Microbiology, Inonu University, Malatya, Turkey
- *Corresponding Author:
- Tuba Bayindir
Department of Otorhinolaryngology Head and Neck Surgery,
Inonu University, Malatya,
Turkey,
Tel: 0090 532 6680111;
Email: tuba.bayindir@inonu.edu.tr
Received date: August 23, 2019, Manuscript No. IPMCRS-19-1600; Editor assigned date: August 28, 2019, PreQC No. IPMCRS-19-1600 (PQ); Reviewed date: September 11, 2019, QC No. IPMCRS-19-1600; Revised date: August 22, 2022,QI No:IPMCRS-19-1600;Manuscript No.IPMCRS-19-1600(R); Published date: September 19, 2022, DOI: 10.36648/2471-8041.8.8.242
Citation: Bayindir T, Aydin S, Erbay MF, Gusro CA, Toplu Y, et al (2022) Does Topical Antifungal Treatment plus Conventional Treatment to Modality Improve Prognosis in Rhinoorbitocerebral Mucormycosis? Med Case Rep Vol.8 No.8: 242.
Abstract
Mucormycosis is an aggressive fungal infection with high mortality rates, caused by the members of the mucarales order belonging to rhizopus, mucor and rhizomucor; less commonly cunninghamella, absidia, saksenaea and apophysomyces. The fungal sporangiospores are present in nature and found worldwide in soil, contaminated foods or decaying organic substances. Infection occurs either inhalation of these sporangiospores or direct inoculation of the fungi into the eroded skin and mucosa. They are angioinvasive organisms and cause thrombosis of the vessels with consequent infarction and tissue necrosis. There are different clinical types including; rhinocerebral, pulmonary, cutaneous, gastrointestinal and disseminated forms. The most common type is rhinocerebral form and the most isolated pathogen is rhizopus spp (90%).
Keywords
Cunninghamella ; Rhinoorbitocerebral mucormycosis ; Rhizomucor; Myelocytic leukemia
Introduction
Mucormycosis classically characterized as an opportunistic fungal infection, preferably effecting patients with uncontrolled Diabetes Mellitus (DM), patients receiving long-term chemotherapy due to haematological malignancies and in longterm neutropenic patients, solid organ or hematopoietic stem cell transplantation patients, patients using long-term corticosteroids, hemodialysis patients receiving desferoxamine, patients with Acquired Immune Deficiency Syndrome (AIDS) and pregnancies, it can also rarely cause illness in immuncompetant hosts. The treatment is comprising of early diagnosis, aggressive surgical debridement of the necrotic tissues, proper dose of systemic antifungal therapy and management of concomittant predisposing factors [1]. Despite the conventional treatment modality mortality rates of mucormycosis remains high with ranging from 40%-80% depending on underlying conditions, sites and spread of infection [2]. In localized sinus infection, earlier tissue based diagnosis and surgical treatment may provide cure and lower mortality rates can be seen. But disseminated disease especially cerebral involvement is often associated with high mortality rates. In the present study we aimed to evaluate the efficiency of the topical antifungal treatment plus conventional therapy on improved survival, by presenting the clinical course of the six patients whom were treated with both systemic and topical Liposomal Amphotericin B (LAMB) after surgical debridement [3].
Case study
Patients
In this study we evaluate the effectiveness of the added topical LAMB in six cases who were diagnosed as mucormycosis according to meticulous history, clinical signs and symptoms and radiological evaluation, retrospectively. Also confirmation of diagnosis by histopathology, culture, DNA isolation from the tissue and ITS1/ITS4 gene sequence analysis were done. The cases were evaluated in terms of demographic characteristics, presentation, signs and symptoms, predisposing factors, radiological findings, clinical and therapeutic outcomes (Tables 1 and 2).
| Case | Age | Gender | Predisposing factors | Signs/symptoms |
|---|---|---|---|---|
| 1 | 51 | F | Uncontrolled type II DM | Facial edema and pain on the right maxillary region after tooth extraction |
| Renal transplantation | Proptosis | |||
| 2 | 65 | M | Uncontrolled type II DM | Necrotic lesion on the hard palate |
| Ischemic cerebrovascular disease | Fever | |||
| 3 | 70 | M | No known chronic disease other than chronic obstructive pulmonary disease and hypertension | Skin necrosis at the left maxillo-zygomatic area |
| 4 | 65 | F | Acute myelocytic leukemia | Epistaxis |
| Facial edema and pain | ||||
| Fever | ||||
| 5 | 4 | F | Acute lymphoblastic leukemia | Epistaxis |
| Fever |
Table 1: Demographic characteristics, predisposing factors and signs/symptoms of the patients.
| Case | Diagnostic methods | Treatment modality | Follow-up | ||
|---|---|---|---|---|---|
| Pathologic diagnosis | Microbiologic diagnosis | Surgical therapy | Medical therapy | 6 years | |
| 1 | Mucormycosis | Mucor spp. | 1.ESC (Total sphenoethmoidectomy) 2.Middle+Inferior turbinate subtotal resection 3.Left Orbital exenteration |
Systemic LAMB (7.5 mg/kg/day IV) Topical (Diluated) LAMB |
|
| 2 | Mucormycosis | Mucor spp. | 1.ESC (Bilateral sphenoethmoidectomy) 2.Partial hard palate+subtotal septum+inferior turbinate resection |
Systemic LAMB (7.5 mg/kg/day IV) Topical (Diluated) LAMB |
2 years |
| 3 | Mucormycosis | Mucor spp. | 1. ESC (total sphenoethmoidectomy) 2.Skin resection (Nasal dorsum+left forehead+maxillo-zygomatic region) 3. Left Orbital exenteration 4. Subtotal septum+Middle turbinate resection |
Systemic LAMB (7.5 mg/kg/day IV) Topical (Diluated) LAMB |
- |
| 4 | Mucormycosis | Mucor spp. | 1.ESC (Bilateral sphenoethmoidectomy) 2. Lateral rhinotomy incision (partial resection on the skull base+partial maxillectomy) 3.Subtotal septum+Inferior+Middle turbinate resection |
Systemic LAMB (7.5-10 mg/kg/day IV) Topical (Diluated) LAMB |
- |
| 5 | Mucormycosis | Mucor spp. | 1.Subtotal septum+left inferior concha resection 2.Partial endoscopic left medial maxillectomy+total ethmoidectomy+middle mea antrostomy 3.Partial middle turbinate resection |
Systemic LAMB (3 mg/kg/day IV) Topical (Diluated) LAMB |
1 year |
| 6 | Mucormycosis | Rhizopus oryzae | 1.ESC (total sphenoethmoidectomy) 2.Left middle+inferior turbinate subtotal resection 3.Left Orbital exenteration |
Systemic LAMB (7.5-10 mg/kg/day IV) Topical (Diluated) LAMB |
- |
Table 2: Diagnostic methods, treatment modality and outcomes of the patients.
Predisposing factors
Five of 6 patients were immunocompromised and one patient had no known chronic disease other than chronic obstructive pulmonary disease and hypertension. Three patients were suffering from DM and had uncontrolled type II DM, two of these patients were using intensive immunosuppressive therapy due to renal transplantation and one had ischemic cerebrovascular disease history. One patient had Acute Myelocytic Leukemia (AML) and one patient had Acute Lymphoblastic Leukemia (ALL). Age ranged from 4 to 70 years (mean age 51.17 years).
Clinical signs and symptoms
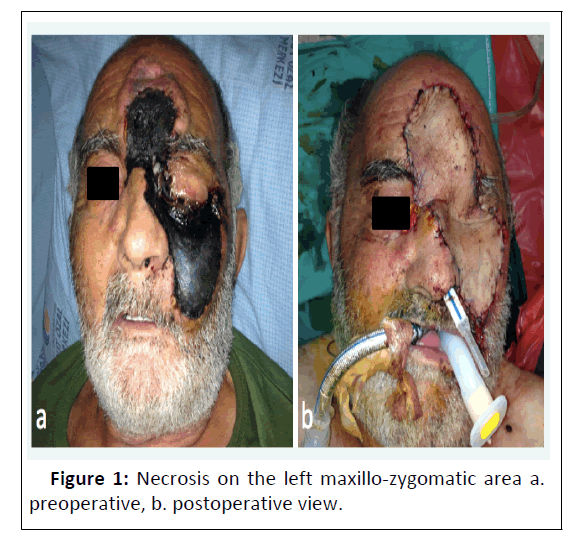
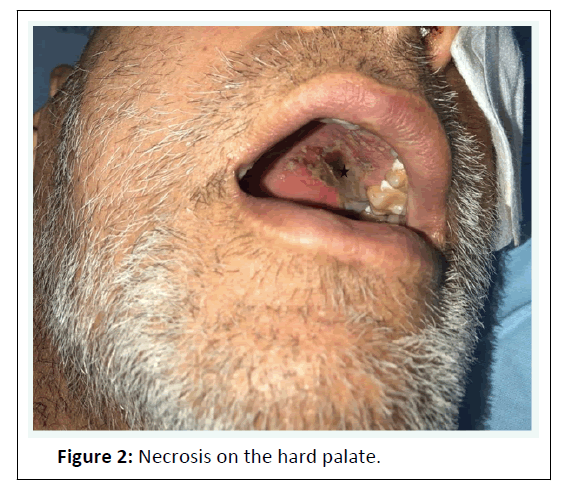
Chief complaint was facial edema and pain, fever and epistaxis. There were infraorbital anesthesia on involved check. Necrosis on the left maxillo-zygomatic area in one patient (Figure 1) and necrotic lesion on the hard palate in one patient (Figure 2) was present. On endoscopic examination all patients had black blood stained debris with necrosis in region of nasal septum, lateral wall of nasal cavity, inferior and/or middle turbinate or nasal floor (Figure 3). Two patient had periorbital edema, proptosis and altered vision in initial examination.
Radiological findings
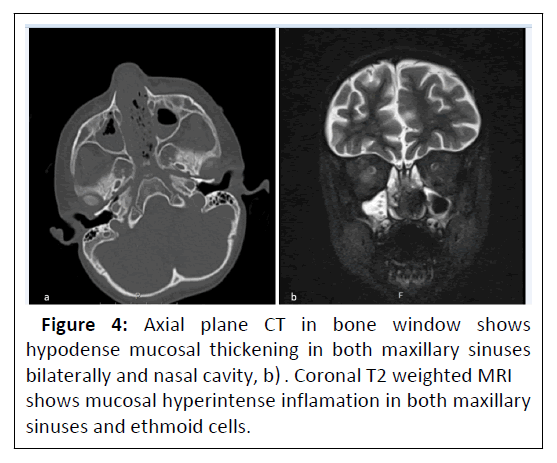
Except pulmonary mucormycosis, imaging studies have no specific or sensitive sign for sinonasal mucormycosis [4]. The most common radiographic finding will be sinusitis, which cannot be differentiate from bacterial/viral infection. Nonspecific inflammatory soft tissue changes can be detected in Computed Tomography (CT) as indicators for mucormycosis correlated with nasal endoscopy. Bone destruction and osseous erosion are rare, but obvious signs of the disease that could be seen in late stages [5]. However, CT and Magnetic Resonance Imaging (MRI) scan of Paranasal Sinuses (PNS) and brain were obtained to define the extention of disease. Mucosal hypodense thickening both nose and PNS was seen in all six patients and bone destruction was present in 3 patients on CT scan (Figure 4). Also, inflammatory mucosal thickening and heterogenous soft tissue hyperintensities in PNS was present on MRI. Heterogenous signal and contrast enhancement in intraconal space and intraconal fatty tissues consistent with orbital sellulitis were seen in three patients [6,7].
Diagnostic method
Biopsies from involved tissues were taken from all patients at the time of suspicion and were diagnosed as “angioinvasive mucormycosis” based on histopathological examination [8]. Also, microbiological examination for fungal identification from the biopsy samples, Matrix Assisted Laser Desorption Ionization- Time of Flight-Mass Spectrometry (MALDI-TOF MS) based VITEK MS (database v 3.0) system and/or Sanger DNA sequencing was used. Before processing for VITEK MS identification, specimens were cultured on Sabouraud dextrose agar and incubated at 25° C for up to two weeks. Fungal proteins were extracted from the culture using the VITEK MS Mould Kit. To confirm the identification, sequencing of Internal Transcribed Spacer (ITS) region using ITS1/ITS4 primer pair was carried out [9]. 12 PCR amplicons were purified from the agarose gel using QIAquick Gel Extraction Kit and were sequenced using the same primers and ABI Prism Big Dye Terminator v3.1 kit (Applied Biosystems, USA) in both directions. Sequence products were uploaded to ABI Prism 310 Genetic Analyser and nucleotid sequences were blasted against the NCBI database with a similarity cut-off of ≥ 99%. If two or more species fulfilled these criteria, the mould was reported at the genus level. In our patients, direct DNA isolation from the tissue and ITS1/ITS4 gene sequence analysis were done in five patients and five of them identified as Mucor spp. Only in one patient tissue culture was done and fungal colonies were isolated, therefore MALDI-TOF MS and DNA isolation from the tissue and ITS1/ITS4 gene sequence analysis were done and identified as Rhizopus oryzae [10].
Treatment modality
Surgical debridement, systemic and topical administration of Liposomal Amphotericin B were done to all patients. Treatment with systemic LAMB (7.5 mg/kg/day) via Intravenous Route (IV) was commenced since the suspicion of mucormycosis and the dose was increased up to 10 mg/kg/day if necessary, in addition to management of predisposing factors. Only in one case (pediatric patient) the systemic LAMB was used 3 mg/kg/day/IV. Also, surgical debridements were performed both by endoscopic and open approach surgery. Orbital exenteration was done in three of 6 patients [11]. Hard palate resection in one patient and nasal dorsum skin, skin of the left forehead, skin on the maxillozygomatic region resections in one patient were done in addition to endoscopic surgery. Either in endoscopic or open approach surgery, necrotic tissues were debrided until healty tissue was seen macroscopically. Only in one patient because of skull base invasion minimal mucor burden was left. After the completion of the surgery, lavage of the surgical field and placement of cottonoid pledgets soaked with diluated LAMB were done in all patients. Patients were examined daily and surgical field was irrigated four times in a day with diluated LAMB, with concentration of 1 mg/20 ml and volume 1 ml to 15 ml, postoperatively. Three patients received either parenteral or topical diluated LAMB until they died (10th, 19th and 37th days). Three survived patients were received parenteral and topical diluated LAMB 103, 77 and 37th day, respectively. The home treatment with oral posaconazole in two patients and voriconazole in pediatric patient was continued up to the resolution of clinical signs and symptoms, normalization or stabilization of radiological abnormalities and resolution of underlying immunosuppressive condition [12].
Treatment outcomes
Despite aggressive surgical debridement, systemic and topical LAMB therapy, three of six patients had progressive disease and were died during treatment (10th, 19th and 37th days). And three patients were recovered with no evidence for recurrence or fungal infection. Follow-up period for the survived patients were 1 to 6 years (mean 35 months). Moreover, the routine control of 3 survived patients still continues [13].
Results
Mucormycosis is an opportunistic fungal infection. Fungal sporangiospore forms that are widespread in nature reach the respiratory tract and the oral cavity through inhalation, but the immunological system does not constitute a serious human disease except in rare cases who have risk factors. The spores taken by inhalation are phagocytosed by the mononuclear and polymorphonuclear system and then eliminated. In situations that cause phagocytosis dysfunction such as diabetic ketoacidosis, spores escape from the phagocytosis system and invade the vascular endothelium. As the vascular invasion occurs, acidosis in the microcirculation increases and the acidic environment allows the rapid growth of the fungal hyphae. Furthermore, in diabetic patients, the iron binding capacity of transferrin is reduced and the increased iron content facilitates the proliferation of fungi [14]. This situation predispose the development of mucormycosis in patients with hemochromatosis and hemodialysis patients with overloaded iron. Diabetes mellitus and consequently diabetic ketoacidosis are predominant (60%-80%) predisposing factor, especially in sinus mucormycosis (approximately two-thirds of cases). Hematologic malignancies and solid organ malignancies with chemotherapy, solid organ transplantations with continuous immunosuppressive therapy and bone marrow transplantations are other predisposing conditions. Especially in patients with these predisposing factors, spores initiate the disease by invading the mucosa of the mouth or nasal cavity and sinuses. Fungal hyphaes enlarge the necrotic area by angioinvasion and perineural involvement by the way destroy the surrounding tissues [15]. Fungal emboli in small veins are also important for spreading. If not intervened, orbital and brain invasion develops in a short time. The predisposing factors in our cases were intensive immunosuppressive therapy due to renal transplantation, uncontrolled type II DM, AML, ALL. Only in one case there were no known chronic diseases other than chronic obstructive pulmonary disease and hypertension [16].
Rhinoorbitocerebral mucormycosis is a rare disease, but the increasing prevalence of DM, increased organ transplantation and associated immunosuppressive therapies are indicators of increased the incidence of the disease. In the literature, it is stated that mucormycosis has an increasing trend worldwide. Particularly in patients with predisposing conditions, complaints of acute developed headache, nasal obstruction and nasal discharge, unexplained fever, loss of vision, edema in the periorbital region and focal neurological deficits, rhinocerebral mucormycosis should be considered in the differential diagnosis [17]. Although the pathways of spread in rhinoorbitocerebral mucormycosis are not clearly known, generally course of the disease known as; initially involvement of the nasal mucosa, spreading to the paranasal sinuses (especially the ethmoid and maxillary sinuses), orbit and finally the intracranial fossa. Different clinical manifestations or clinical signs and symptoms of the disaese lead to think about the pathway that responsible of spread. Pterygopalatine fossa via pterygopalatine foramen considered as the potential conduit for the extensive disease (involvement of orbita, retrobulbar space, intracranial fossa and facial soft tissues) and might be percieved as the main reservoir for the mucormycosis [18].
Discussion
For diagnosis, complaints of patients with a predisposing factor should assessed carefully and a complete otolaryngologic examination should performed [19]. Deep biopsies should be performed rapidly in the presence of suspected lesions (black crusted, necrotic or ulcerative lesions) of the oral and/or nasal cavity, histopathological and microbiological examination of the samples should be conducted. Diagnosis can be confirmed by radiologically and pathologically, if the culture based diagnosis is impossible or not succeeded. Besides, the diagnosis is unfortunately postmortem in some cases [20].
In microbiological examination randomly segregated hyphae without septum seen by microscope and mucormycosis colonies on Sabouraud Dextrose Agar (SDA) medium should be seen for diagnosis. But conventional methods have low sensitivity and specifity in the diagnosis of mucorales family members [21]. Some investigational studies demonstrated that using Polymerase Chain Reaction (PCR)-based techniques on specimens can enhace diagnosis. The gold standard for the diagnosis of mucormycosis is the isolation of the agent in culture. Unfortunately, undelivered samples to microbiology laboratory is still an important problem. This may lead to delay in diagnosis and cause further increase in mortality and morbidity [22]. In cases whom zygomycosis is suspected, the importance of mycological culture should be kept in mind by clinicans who perform surgical procedures for diagnosis and treatment. Along with the advances in molecular biological methods, techniques have been developed which can give rapid, sensitive and accurate results in the diagnosis of the pathogen. The vast majority of molecular methods are based on the ITS region that was selected as pan-fungal barcode by International Subcommission on Fungal Barcoding and ITS sequencing was found sufficient to identify the genus and species level of the Mucormycetes members [23].
Since early diagnosis and treatment are crurical in this disease, all microbiological, pathological and radiological methods should be used to confirm the diagnosis without delaying. The gold standard imaging method is contrast enhanced CT scan to show bone destruction, swelling of the soft tissue and extraocular muscles or opacification of paranasal sinuses and edematous mucosa. Also MRI can be used to assess involvement of soft tissues, demonstrate intracerebral infection and by enhanced images early vascular invasion may detect [24].
The most important management modality of mucormycosis is immediate and radical surgical debridement along with appropriate systematic antifungal therapy [25]. If total debridement is not feasible, minimal mucor burden could be released. But, former data supports that radical surgical debridement can optimize cure rates and local control of the disease dramatically impacts survival rates in rhinoorbitocerebral mucormycosis. Amphotericin B must be initiated immediately since suspicion of mucormycosis. The studied first-line treatment for mucormycosis is amphotericin B and its lipid formulations and recently isavuconazole. Posaconasole is an other option sepecially studied for salvage therapy. During antifungal therapy the underlying predisposing condition should be tried to adjust, especially in the presence of uncontrolled DM [26]. The dose for classical amphotericin B is 1-1.5 mg/kg/day. However, nephrotoxicity risk of classical amphotericin B, the lipid form can be preferable to reduce the risk, also the dosage can be increased up to 10 mg/kg/day. In our cases, five of six were treated with LAMB mg/kg/day/IV and the dosage was increased up to 10 mg/kg/day/IV when needed, whereas one pediatric patient was treated with 3 mg/kg/day/IV [27].
Also, there is no consensus in the literature about the duration of antifungal therapy. General suggestion for the recommended duration is to sustain the treatment until the time of response, which lasts at least 6-10 weeks. European Society for Clinical Microbiology and Infectious Diseases (ESCMID) and European Confederation of Medical Mycology (ECMM) Joints recommended to continue antifungal treatment until a complete resolution seen on radiological imaging. The effect mechanism of amphotericin B is related to its ability to form permeable channels in the cellular membrane of the pathogen, which leads to cell death. Its accepted that, delayed diagnosis and delayed treatment, in-complete surgical removal, disseminated infection especially involvement of central nervous system and pulmonary system infection are associated with higher risk of mortality [28]. Delaying systemic amphotericin B treatment also reported as an independent predictor for mortality in patients with hematologic malignancies. In localized sinus infection, earlier tissue based diagnosis and complete surgical debridement may provide cure and lower mortality rates. To increase the local effect of antifungal drugs topical application can be an option to decrease mortality rates. Topical application provides major tissue accumulation on the site of application. Therefore, to decrease the systemic absorption and toxicity, local irrigation can be delivered at a lower dose or can be delivered by diluation. The local irrigation with LAMB by surgical packing of orbit, nasal cavity and/or sinuses and chest wound for invasive fungal infections caused by the Mucoraceae family of fungi, was reported in the literature but dose, concentration, volume and duration of topical LAMB did not defined well and clearly [29]. A larger study with 30 patients who diagnosed as mucormycosis and whom infection was limitted to nose and sinuses was presented in literature. All patients underwent endoscopic surgery and were treated with 1 mg/kg/day/IV amphotericin B. Also after surgical resection, amphotericin B solution was applied to nasal cavity by cottonoid pledgets for 15 minutes and topical treatment was lasted for five consecutive days, once daily. The overall survival rate was found 60% and the authors point out that this survival rate showed improvement with less morbidity in comparision with the conventional treatment at their centre. In our six cases, all patients treated with topical diluated LAMB in addition to conventional treatment modality. In contrast to that study, five of six cases had mucormycosis not limitted to nose and sinuses. Neverthless three of them were survived. Even though we used topical antifungal therapy plus conventional therapy on a small number of cases, the mortality rate can be accepted lower for these patients with more extended disease. Due to the rarity of the disease there is no published datas with large series that compares conventional treatment with topical LAMB enhanced novel treatment modality. So that, well-designed controlled studies are needed to evaluate the response, define the effect on survival rates, to demonstrate the optimal dose and duration for the topical antifungal therapy [30].
Conclusion
In conclusion; early diagnosis, reversal of predisposing factors, aggressive surgical debridement and prompt administration of systemic antifungal therapy are critical steps for good outcomes in mucormycosis. Because of the aggressive nature of the disease, every possible effective treatment modality such as topical administration of LAMB may be considered. It is difficult to compare the benefit of this approach with conventional treatment modality by randomized-controlled trials, because of the rarity of the disease, presentation variety and patient comorbidities. In literature the improved outcomes of extensive invasive mucormycosis were reported in some case reports, in which combining topical and systemic antifungal therapy with aggressive surgical treatment. Finally, multicenter studies are needed to provide sufficient evidence for recommendation of additional topical antifungal therapy in the related guidelines.
References
- Kontoyiannis DP, Levis RE (2015) Agents of mucormycosis and entomophthoramycosis. in: Bennett je, dolin r, blaser mj editors. mandell, douglas, and bennett’s principles and practice of infectious diseases. Elsevier 1: 2909-2919.
- Kursun E, Turunc T, Demiroglu YZ, AlıÅ?kan HE, Arslan AH, et al. (2015) Evaluation of 28 cases of mucormycosis. Mycoses 58: 82-87.
- Guinea J, Escribano P, Vena A (2017) Increasing incidence of mucormycosis in a large Spanish hospital from 2007 to 2015: Epidemiology and microbiological characterization of the isolates. PLoS One 12: e0179136.
- Danion F, Aguilar C, Catherinot E (2015) Mucormycosis: New developments into a persistently devastating infection. Semin Respir Crit Care Med 36: 692-705.
- Kömür S, Ä°nal AS, Kurtaran B (2016) Mucormycosis: A 10-year experience at a tertiary care center in Turkey. Turk J Med Sci 46:58-62.
- Marty FM, Ostrosky-Zeichner L, Cornely OA (2016) Isavuconazole treatment for mucormycosis: A single-arm open-label trial and case-control analysis. Lancet Infect Dis 16: 828-837.
- Mallis A, Mastronikolis SN, Naxakis SS (2010) Rhinocerebral mucormycosis: An update. Eur Rev Med Pharmacol Sci 14: 987-992.
- Spellberg B, Kontoyiannis DP, Fredricks D (2012) Risk factors for mortality in patients with mucormycosis. Med Mycol 50: 611-618.
- Palejwala SK, Zangeneh TT, Goldstein SA (2016) An aggressive multidisciplinary approach reduces mortality in rhinocerebral mucormycosis. Surg Neurol Int 7: 61.
- Walsh TJ, Skiada A, Cornely O (2014) Development of new strategies for early diagnosis of mucormycosis from bench to bedside. Mycoses 57: 2-7.
- Herrera DA, Dublin AB, Ormsby EL (2009) Imaging findings of rhinocerebral mucormycosis. Skull Base 19: 117-125.
- White TJ, Bruns T, Lee S (1990) Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics. In: Innis MA, Gelfand DH, Sninsky JJ, White TJ, editors. PCR protocols: A guide to methods and applications. New York: NY Academic Press 315-22.
- Bitar D, Van Cauteren D, Lanternier F (2005) Increasing incidence of zygomcosis (mucormycosis), France, 1997-2006. Emerg Infect Dis 41:634-53.
- Bouza E, Munoz P, Guinea J (2006) Mucormycosis: An emerging disease? Clin Microbiol Infect 12: 7-23.
[Crossref][Google Scholar][Pubmed]
- Gamaletsou MN, Sipsas NV, Roilides E (2012) Rhino-orbital-cerebralmucormycosis. Curr Infect Dis Rep 14: 423-34.
- Hilal AA, Taj-Aldeen SJ, Mirghani AH (2004) Rhinoorbital mucormycosis secondary to Rhizopus oryzae: A case report and literature review. Ear Nose Throat J 83: 556-62.
- Hosseini SM, Borghei P (2005) Rhinocerebral mucormycosis: Pathways of spread. Eur Arch Otorhinolaryngol 262: 932-938.
- Hammond SP, Bialek R, Milner DA (2011) Molecular Methods to improve diagnosis and identification of mucormycosis. J Clin Microbiol 49: 2151-2153.
- Badotti F, Fonseca PLC, Tomé LMR (2018) ITS and secondary biomarkers in fungi: Review on the evolution of their use based on scientific publications. Rev Bras Bot 41: 471-479.
- Prasad K, Lalitha RM, Reddy EK (2012) Role of early diagnosis and multimodal treatment in rhinocerebral mucormycosis: experience of 4 cases. J Oral Maxillofac Surg 70: 354-362.
- Turner JH, Soudry E, Nayak JV (2013) Survival outcomes in acute invasive fungal sinusitis: A systematic review and quantitative synthesis of published evidence. Laryngoscope. 123: 1112-1118.
- Vironneau P, Kania R, Morizot G (2014) Local control of rhino-orbito-cerebral mucormycosis dramatically impacts survival. Clin Microbiol Infect 20: 336-339.
- Cornely OA, Arikan-Akdagli S, Dannaoui E (2013) ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect 20: 5-26.
- Sipsas NV, Gamaletsou MN, Anastasopoulou A (2018) Therapy of Mucormycosis. J Fungi (Basel) 4: E90.
- Vaezi A, Moazeni M, Rahimi MT (2016) Mucormycosis in Iran: A systematic review. Mycoses 59: 402-415.
- Saedi B, Sadeghi M, Seilani P (2011) Endoscopic management of rhinocerebral mucormycosis with topical and intravenous amphotericin B. J Laryngol Otol 125: 807-810.
- Frankenburg S, Glick D, Klaus S (1998) Efficacious topical treatment for murine cutaneous leishmaniasis with ethanolic formulations of amphotericin B. Antimicrob Agents Chemother 42: 3092-3096.
- Kahana A, Lucarelli MJ (2007) Use of radiopaque intraorbital catheter in the treatment of sino-orbito-cranial mucormycosis. Arch Ophthalmol 125: 1714-1715.
- Pelton RW, Peterson EA, Patel BC (2001) Successful treatment of rhino-orbital mucormycosis without exenteration: the use of multiple treatment modalities. Ophthal Plast Reconstr Surg 17: 62-66.
- Di Pentima MC, Chan S, Powell J (2014) Topical amphotericin B in combination with standard therapy for severe necrotizing skin and soft-tissue mucormycosis in an infant with bilineal leukemia: Case report and review. J Pediatr Hematol Oncol 36: 468-70.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences