Covid-19 Associated Cerebral Infarction in an Elderly Patient: A Case Report
Jumin Xie, Changwu Feng, Zhu Wang* and Jie Chen
Jumin Xie1,2, Changwu Feng3 Zhu Wang3* and Jie Chen4
1Department of Respiratory Medicine, PhD, director of central lab of Medical college of Hubei Polytechnic University, Huangshi, Hubei, China, 435003.
2Department of Respiratory Medicine, Hubei key laboratory of renal disease occurrence and intervention, Hubei Polytechnic University, Huangshi, Hubei, China, 435003.
3Department of rehabilitation, Huangshi Central Hospital, Affiliated Hospital of Hubei Polytechnic University, Edong Healthcare Group, Huangshi, Hubei, China, 435000.
4Department of Respiratory Medicine, Huangshi Central Hospital, Affiliated Hospital of Hubei Polytechnic University, Edong Healthcare Group, Huangshi, Hubei, China, 435000.
- *Corresponding Author:
Received Date: September 01, 2021; Accepted Date: September 21, 2021; Published Date: September 30, 2021
Citation: Xie J, Feng C, Wang Z and Chen J (2021) Covid-19 Associated Cerebral Infarction in an Elderly Patient: A Case Report. Med Case Rep Vol.7 No.9.201
Abstract
Background: The 2019 severe acute respiratory syndrome coronavirus (SARS-Cov-2) was initially declared as a health emergency by the World Health Organization, which eventually progressed to a pandemic. To date, more than 213,752,662 people worldwide have been infected by SARS-Cov-2, resulting in 4,459,381 deaths. Various clinical characteristics and studies have been described regarding SARS-Cov-2.
Case presentation: There are very few reports about cases of patients with a COVID-19 infection accompanied by cerebral infarction. In this report, we present the case of a 74-yearold patient who was infected with SARS-Cov-2 in late January and later developed a cerebral infarction. Following appropriate treatment, the patient recovered and was discharged from hospital on April 3, 2020. Follow-up after 10 months revealed that the patient was living a normal life without any obvious sequelae.
Conclusions: This paper presents the management and treatment of an elderly patient who suffered from COVID-19 associated with a cerebral infarction. Following discharge from Huangshi Central Hospital, the patient lived a normal life without any clinical sequelae. We believe that the early introduction of traditional Chinese medicine played an important role in the treatment of COVID-19. We aim to spread awareness on COVID-19 and to suggest a therapy for COVID-19 patients with a concomitant cerebral infarction.
Keywords
SARS-Cov-2; COVID-19; cerebral infarction; elderly patient; case report
Introduction
The novel severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2), which causes severe pneumonia, has spread to 223 countries, areas, and territories worldwide. More than 213,752,662 people have been infected, resulting in 4,459,381 deaths, according to the World Health Organization. The coronavirus disease 2019 (COVID-19), which is caused by the SARS-Cov-2 virus, is now a pandemic that has had an enormously negative impact on the economy and threatens to the health and lives of people around the world. SARS-Cov-2 belongs to the betacoronavirus genus, which is associated with 229E, OC43, NL63, HKU1, severe acute respiratory syndrome coronavirus (SARS-Cov), and Middle East respiratory syndrome coronavirus (MERS-Cov) [1,2].
SARS-Cov-2 is an enveloped positive-sense RNA virus and is the seventh member of the human coronavirus family that causes infections in humans. Together with SARS-Cov and MERS-Cov, SARS-Cov-2 can cause fatal pneumonia in humans [2]. Studies have proven that the spike protein of SARS-Cov-2 is the molecular determinant of viral attachment, fusion, and entry into the host cells [3,4]. The SARS-Cov-2 spike protein combines withangiotensin-converting enzyme 2 (ACE2) and acts with transmembrane serine protease 2 (TMPRSS2) to promote cellular entry [5]. The structure of the spike protein receptorbinding domain (RBD) has been determined, and the essential residues in ACE2 binding have been revealed [6,7]. SARS-Cov-2 and RaTG13, which were isolated from a bat in 2013, show a high genetic similarity to to each other, having a 93.1% nucleotide identity [1]. Phylogenetic analysis of the SARS-Cov-2 genome elucidated the high probability of the virusoccurring naturally and originating from bats [1]. Analysis of the amino residues in the SARS-Cov-2 RBD showed highly conserved amino acids and side chain properties similar to those in the SARS-Cov RBD, which allows ACE2 binding [8].
A variety of characteristics related to COVID-19 have appeared in all ages during the recent months. Typical symptoms include fever, cough, headache, fatigue, gastrointestinal symptoms, chest tightness, and dyspnea [9]. In this paper, we present a 74-yearold man with a COVID-19 infection who developed cerebral infarction and encephalatrophy during the early stages of SARSCov- 2 pandemic in Huangshi, China. Real-time polymerase chain reaction (RT-PCR) of a throat swab taken from the patient confirmed the presence of SARS-Cov-2. After 1 month of treatment, viral nucleic acid testing was performed three times, all having negative results. He was classified as having recovered from COVID-19 and was discharged on April 3, 2020. Follow-up after 5 months showed that the patient had a healthy overall condition without any clinical and diagnostic sequelae.
Case Report
A 74-year-old man was sent to the Huangshi Hospital of Traditional Chinese Medicine on January 31, 2020 due to, fever, cough, headache, diarrhea, vomiting, fatigue and dyspnea for 2 days. Weakness in the right extremities, distortion of commissure, and lalopathy, which were present since the middle of January, were also noted. Blood tests revealed elevated monocyte count (0.64 g/L), mean platelet volume (12.00 fL), and percentage of monocytes (16.30%).
On February 3, blood tests were performed, which revealed that the eosinophil count (0.00 g/L), percentage of eosinophils (0.00%), platelet count (87 g/L), mean corpuscular hemoglobin concentration (315 g/L) and hemoglobin concentration (129 g/L) were all decreased on February 3, 2020.
The coagulation profiles were tested and are shown in (Table 1). The D-dimer and fibrinogen degradation products were markedly increased compared with the normal reference range, while the other parameters were normal. As the hospital was 80 kilometers away from Wuhan, which was the epicenter of the COVID-19 outbreak. SARS-Cov-2 RNA testing was unavailable in our institution in early February. However, we speculated that he was infected with SARS-Cov-2, hence, we performed a thoracic computed tomography (CT) scan to confirm our diagnosis.
| Items | Results | Unit | Ref range |
|---|---|---|---|
| Prothrombin time | 11.6 | S | 9.00-14.00 |
| International normalized ratio of prothrombin time | 0.91 | -- | 0.85-1.15 |
| Activated partial thromboplastin time | 27.3 | S | 20.0-41.0 |
| Thrombin time | 12.2 | S | 8.0-14.0 |
| Fibrinogen | 3.98 | g/L | 2.00-4.00 |
| D-dimer | 4.81 | μg/mL | 0-0.50 |
| Fibrinogen degradation products | 143.25 | μg/L | 0-5.00 |
Table 1. Coagulation profiles.
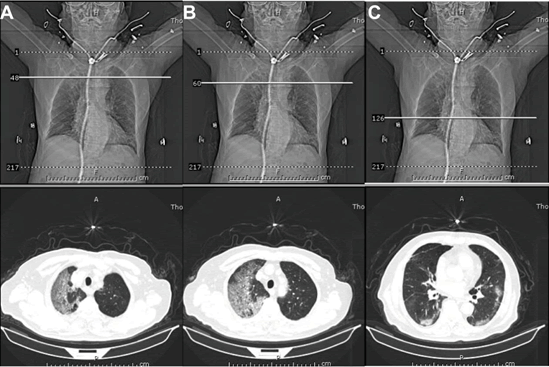
The thoracic CT scan images taken on February 5, 2020, these images showed ground-glass opacities in the right and left middle lobes of the lung, indicating the possibility of viral pneumonia (Figure 1). Based on his clinical features and the results of the CT scan, he was hospitalized for further investigation due to suspected COVID-19 infection, and he was given antiretroviral, antispasmodic, and anti-asthmatic expectorant therapies.
On February 7, the thoracic CT scan images showed progression of the ground-glass opacities in both the lobes as compared with the images on February 5. Blood tests on the same day showed elevation of the neutrophil granulocyte count and ratio, which indicated a pathogenic infection. On February 9, blood tests showed elevation of the WBC count, neutrophil granulocyte count and ratio, and monocyte count, while there was a decrease in the lymphocyte and eosinophil counts and eosinophil percentage. Since there was a lack of the SARS-Cov-2 RNA testing equipment at Huangshi in early February, no nucleic acid results could prove the presence of a COVID-19 infection.
On February 10, 14, 20, 24, 25 and March 1, 2, 5, 10, 14 and 20, the coagulation profiles were tested. Except on March 20, the level D-dimer (normal range, 0-0.50 μg/mL) on all dates was above the normal. Previous studies have demonstrated that the D-dimer level was an important indicator for predicting the presence of a COVID-19 infection and in-hospital mortality [10]. In the early stages of the patient’s disease, the D-dimer level was 4.81 μg/mL, which was markedly elevated compared with the normal range. We then investigated the prothrombin time (PT), thrombin time (TT) and fibrinogen (Fg), which were also significant indicators for confirming the presence of a COVID-19 infection. PT and Fg were elevated during the middle infection stage, while TT was elevated during the early stages.
In the middle of February, the patient experienced sudden onset of right limb weakness accompanied with a drooping mouth, difficulty in speaking, and other discomforts. The initial CT scan images of the brain revealed a cerebral infarction affecting the bilateral basal ganglia area, radial coronal area, bilateral frontal parietal lacunar, partial softening lesion formation, leukoencephalopathy, and brain atrophy. Anti-biotics, antiplatelets, and medications to improve the patient’s circulation were given.
An interview revealed that the patient had a history of hypertension and type 2 diabetes mellitus. His vital signs were as follows: blood pressure, 135/80 mmHg; pulse rate, 80 bpm; and body temperature, 37oC. On physical examination, it was revealed that there was no yellowing of the skin, no lymph node enlargement in the superficial layer, clear respiratory sound in the lungs, no rales and dryness. The heart rhythm was regular, heart, murmurs were absent, the abdomen was flat and soft, and swelling was absent in both lower extremities. Three-dimensional reconstruction of the lungs, mediastinum, heart, and ribs on February 22 showed a viral infection in both the lungs, calcification of the aorta and coronary artery wall, arteriosclerosis, enlarged lymph nodes in the mediastinum, and localized adhesion of the pleura of both the lungs, multiple circular light-transmitting areas that were localized in the lower lobes of both lungs, and emphysema with interstitial pneumonia. Compared with the chest CT images on February, the lesions in the upper lobe of the left lung and the lower lobe of the right lung increased in size, while those in the lower lobe of the left lung and the upper lobe of the right lung decreased in size.
SARS-Cov-2 antibodies were tested on March 1, 2020, which revealed the following results: IgG, 123.64 AU/mL; IgM 16.89 AU/ mL. Both indices exceeded the normal range (0-10.00 AU/mL). On March 3, the patient was transferred to Huangshi Central Hospital for systemic detection and treatment. On March 5, the levels of IgG and IgM were measured at 77.80 AU/mL and 5.72 AU/mL, respectively. The elevated IgG level together with the chest CT results confirmed the presence of SARS-Cov-2 pneumonia.
On admission, the patient had fever, cough, headache, and dyspnea. Antiviral therapy was initially administered to treat the patient. As his physical condition improved, our focus shifted on the additional detection. CT scans of the brain showed a cerebral infarction, and the patient developed symptoms of encephalopathy on March 10, which worsened on March 16. The pulmonary function test results revealed a favorable outcome, and the result of the PCR analysis on March 19 was negative for SARS-Cov-2. During this period, his vital signs were as follows: body temperature, 36.5oC; blood pressure, 120/75 mm Hg; respiratory rate, 19 breaths per minute; and heart rate, 75 beats per minute. He had no cough, dyspnea, shortness of breath, and chest pain, and, ventilator assistance was not needed. Oxyhemoglobin saturation reached 100%.
The recommended medications suggested by the guidelines were as follows: for antiplatelet aggregation, (clopidogrel hydrogen sulfate tablet 25 mg po qid); to lowerlipids and stabilize plaque, (rosuvastatin 5 mg po qid); to control the heart rate and protect the heart muscle, (metoprolol tartrate controlled-release tablet 25 mg po qid); to control blood pressure, (felodipine sustained release tablet 5 mg po qid); for mucolytics, (acetylcysteine effervescent tablets 0.6 g po bid); and for antivirals, (imipenemastatin 0.5 g IV). Aside from the medications, management of the patient included a rehabilitation training therapy (PT OT therapy).
On March 21, the patientexperienced a brief episode of palpitation, but his vital signs were stable. Regardless, cardiac enzymes such as troponin and B-natriuretic peptide were measured, which revealed normal levels 0.01 ng/mL and 50 pg/ mL, respectively. The result of the SARS-Cov-2 nucleic acid testing on March 31 was negative. The patient was physically stable and he was discharged from the hospital on April 3. In the following months, patient’s physical condition was regularly monitored, and no obvious sequelae were observed.
Discussion
WHO declared COVID-19 as a pandemic on March 11, 2020. The SARS-Cov-2 virus has caused an enormous impact on the public health and economy on a global scale, with the number of infections and deaths still rising. Several reports have proven that the SARS-Cov-2 virus affects the cerebral neurons, resulting in insomnia, headache, stroke, mild cognitive impairment, epilepsy, and encephalorrhagia [11,12]. Meanwhile, SARS-Cov has been shown to also affect the nervous system and induce polyneuropathy, encephalitis, and ischemic stroke. SARS-Cov-2 shares a 79.5% genetic similarity to SARS-Cov, and the main infection sites for both viruses is the lungs [1]. The RBDs of each virus have a similar structure that improves binding to ACE2, and the genome sequence strongly demonstrates a convergent evolution between SARS-CoV-2 and SARS-CoV, although SARSCoV- 2, which belongs to the beta-clade, is not clustered within SARS-Cov and SARS-related coronaviruses. People infected with SARS-Cov-2, have similar symptoms as those with a SARS-Cov infection.
We reported a case of an elderly patient who was infected with SARS-Cov-2 that was associated a with cerebral infarction. It is still unclear Whether SRAS-Cov-2 entries and damages the central nervous system, and additional research is needed to investigate this possibility. Recently, it was reported that SARS-Cov-2 can infect human neural progenitor cells and brain organoids. Although SARS-Cov-2 primarily infects the lungs and causes symptoms, such as fever, dry cough, and acute pneumonia, it can also infect epithelial cells that express the ACE2 receptor. SARS-Cov-2 binds to the ACE2 receptor, which is crucial for blood pressure regulation and viral entry into the cell. The ACE2 receptor, which is present in many organs, facilitates the spread of the virus in the human body and also increases the rate of viral transmission. Determining the crystal structure of the receptorbinding domain (RBD) of the spike protein of SARS-CoV-2 will elucidate the mechanism of viral combination and entry, which will guide intervention strategies that will target the ability of SARS-CoV-2 to recognize receptors [3].
After a systemic comprehensive evaluation that included the breathing rate, oxyhemoglobin saturation, ambulation, and limb coordination, the patient was discharged from the Huangshi Central Hospital on April 3, 2020.
After his discharge, we are still continuously monitored the patient. Physiological indicators have returned to normal except for the neurological sequelae after the cerebral infarction. During the follow-up period, blood tests were performed and the breathing rate and, oxyhemoglobin were monitored, which were all within the normal range. The results of SARS-Cov-2 testing has been negative since his discharge.
Conclusion
Previous reports have mentioned that COVID-19 could cause encephalitis, headache, stroke, arterial and venous thrombosis, hypercoagulability, mild cognitive impairment, epilepsy and encephalorrhagia. However, no evidence has been presented that has proven that SARS-Cov-2 infects brain and cause damage. Additional research is needed to establish the association between cerebral injury and a COVID-19 infection.
Case of cerebral infarction in patients with COVID-19 are limited. Early diagnosis of cerebral infarction in a COVID-19 infection can result in proper guidance and treatment. We reported a case of a 74-year-old patient who recovered from COVID-19 associated with a cerebral infarction. After his discharge from the hospital, the patient lived a normal life without any obvious sequelae. This case may provide information on the treatment and management of similar cases in the future. In addition, we believe that the addition of traditional Chinese medication in the early stages of treatment played a pivotal role in the treatment of COVID-19.
Ethics Approval and Consent to Participate
The Ethics Committee of Huangshi Central Hospital confers this case report submission and publication. The patient would love to share his medical experiences and consent for this case report submission.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editorin- Chief of this journal
Availability of Data and Materials
Availability of data and materials should address to Wangzhu912100@163.com
Competing Interest
The authors declare that they have no competing interests.
Funding
This study was supported by the Fund of Hubei Provincial Department of Education (Q20204508) and Talent Introduction Project of Hubei Polytechnic University (19XJK02R).
Authors’ Contribution
J.X wrote the manuscript. C. F helped with data analysis and shared the case report. Z.W participates in the patient’s treatment and rehabilitation, meanwhile he shared all the testing data of the patient. J. C gave critical suggestions in manuscript writing.
Acknowledgement
We thank the patient for his kind permission and willing to share the experiences.
References
- Zhou P, Yang XL, Wang XG (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579:270-273.
- Zhu N, Zhang D, Wang W, Li X (2020) A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 382:727-733.
- Yan R, Zhang Y, Li Y, Xia L (2020) Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science 367:1444-1448.
- Shang J, Ye G (2020) Structural basis of receptor recognition by SARS-CoV-2. Nature 581:221-224.
- Ziegler CGK, Allon SJ, Nyquist SK, Mbano IM (2020) SARS-CoV-2 Receptor ACE2 Is an Interferon-Stimulated Gene in Human Airway Epithelial Cells and Is Detected in Specific Cell Subsets across Tissues. Cell 181:1016-1035.e1019.
- Walls AC, Park YJ, Tortorici MA, Wall A (2020) Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell 181:281-292.e286.
- Wang Q, Zhang Y, Wu L (2020) Structural and Functional Basis of SARS-CoV-2 Entry by Using Human ACE2. Cell 181:894-904.e899.
- Lan J, Ge J, Yu J (2020) Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature 581:215-220.
- Wang D, Hu B (2020) Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. Jama 2020.
- Zhang L, Yan X, Fan Q, Liu H, Liu X (2020) D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J Thromb Haemost 18:1324-1329.
- Adan GH, Mitchell JW, Marson T (2020 ) Epilepsy care in the COVID-19 era. Clin Med (Lond) 20:e104-e106.
- Aghagoli G (2020) Neurological Involvement in COVID-19 and Potential Mechanisms: A Review. Neurocrit Care 1-10.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences