Cost Effective Trend in Epistaxis Management
Roman Sereda*
Department of Medical Science, University of Lynchburg, Virginia, USA
- Corresponding Author:
- Roman Sereda,
Department of Medical Science,
University of Lynchburg, Virginia, USA
E-mail: rsereda@ut.edu
Received date: January 30, 2023, Manuscript No. IPMCRS-23-15718; Editor assigned date: February 01, 2023, PreQC No. IPMCRS-23-15718 (PQ); Reviewed date: February 10, 2023, QC No. IPMCRS-23-15718; Revised date: February 21, 2023; Manuscript No. IPMCRS-23-15718 (R); Published date: February 28, 2023, DOI: 10.36648/2471-8041.9.1.261
Citation: Sereda R (2023) Cost Effective Trend in Epistaxis Management. Med Case Rep Vol.9 No.1:261.
Abstract
Epistaxis affects much of the population and is a common medical complaint seen across a variety of medical settings. Current standard of care treatment includes a range of options ranging from topical therapy to invasive intranasal device insertion in the absence of specialist involvement. This case report highlights a superior noninvasive treatment approach to uncomplicated epistaxis with tranexamic acid. This cost-effective medication not only reduces rates of recurrence, it increases patient satisfaction while minimizing overall healthcare costs.
Keywords
Tranexamic acid; TXA; Epistaxis
Case Report
A 64-year-old nonsmoker female presented to emergency department with 3-day history of spontaneous, intermittent non-traumatic left sided epistaxis. At the time of presentation, the epistaxis had been on-going for the past two hours and was not resolved with pressure and leaning forward like the previous incidents that patient experienced. She denied use of blood thinners or history of blood diatheses. She denied fever, recent upper respiratory complaints or headache. Physical examination revealed copious hemorrhage from left nare without sinus tenderness on exam. At presentation, her vitals were blood pressure 92/55 mmHg, heart rate 103/min, respiration rate 16/min, temperature 36.7°C, and oxygen saturation 98% on room air. A complete blood count and comprehensive metabolic panel were ordered to evaluate for pathology and showed no gross abnormalities-hemoglobin 11.6 g/dL, hematocrit 34.7 L/L, platelets 266 mcL.
Patient initially treated with 2 sprays of oxymetazoline, and with lack of improvement an anterior/posterior nasal packing Rapid Rhino® was placed. Patient was re-examined 30 mins later. Her epistaxis was controlled and she was discharged with a 10-day supply of cephalexin and an outpatient otolaryngology follow-up. Vitals at discharge: Blood pressure 122/70 mmHg, heart rate 89/min, respiration rate 17/min, temperature 36.7°C, oxygen saturation 100% on room air.
Three hours later patient returned to emergency department with complaints of recurrent epistaxis despite Rapid Rhino® insertion. She complained of difficulty swallowing that she attributed to anxiety from Rapid Rhino® and being unable to breathe through either nare. She denied swallowing blood, nausea, vomiting or headache. All vitals remained stable. At this point, the Rapid Rhino® was removed. Physical re-examination revealed minimal bleeding without clear source and absence of septal hematoma. Patient was then treated with 2,000 mg of nebulized Tranexamic Acid (TXA) that led to prompt resolution of symptoms without need for repacking. Patient also reported resolution of anxiety. She was discharged home and instructed to proceed with otolaryngology outpatient follow-up scheduled from initial visit.
Results and Discussion
Epistaxis affects much of the population and accounts for 1 in 200 emergency room visits, with children and elderly being the most affected populations [1]. Currently, primary treatment includes standard measures such as silver nitrate cauterization, topical medication application with agents such as oxymetazoline, nasal packing, evaluation and management by otolaryngology specialist, and/or a combination of above therapies [2,3].
The use of TXA is an emerging adjunct treatment for epistaxis, usually used to soak the packing material. However, the nebulized form of TXA, as demonstrated in this case, is a leading alternative for definitive treatment of epistaxis which can also provide the patient with a more comfortable and less invasive option.
Tranexamic Acid (TXA) belongs to the class of medications called antifibrinolytics. It prevents excess blood loss by preventing blood clots from breaking down and achieves this by inhibiting the conversion of plasminogen into plasmin the activated form of plasminogen that is responsible for the degradation of fibrin clots [4]. The drug is approved by the Federal Drug Administration for the treatment of heavy menstrual bleeding and short-term prevention for patients with hemophilia prior to dental procedures [5].
It also has many widely accepted off-label uses. Intravenously, it is used off-label in elective cesarean sections, non-traumatic subarachnoid hemorrhages, or orthognathic surgeries to reduce blood loss to name a few. Oral TXA is used off-label for hereditary angioedema, or tooth extractions in patients who are orally anticoagulated. Topically, it is used for treatment of traumatic hyphemas and epistaxis. It can also be used in the nebulized form to manage hemoptysis, post-tonsillectomy hemorrhages and epistaxis.
Recent studies indicate that topical or inhaled TXA is more effective than other treatment options in stopping the hemorrhage and decreasing rates of re-bleeding [2,3,6-8]. From the adverse risk standpoint, the most common side effects reported are gastrointestinal (nausea, diarrhea) and bronchospasm, but are mild and uncommon [6,9].
Other studies have shown no evidence that use of TXA increased one's risk for thromboembolic events or had any adverse events associated with TXA inhalation [10,11]. Although nebulized TXA is an emerging management trend for epistaxis, it has been routinely used to treat hemoptysis and post-tonsillectomy hemorrhages.
A double-blind, randomized control trial by Wand, et al. compared nebulized TXA to normal saline placebo for treatment of hemoptysis [12]. Study concluded that TXA treatment significantly reduced the amount of time to resolution of symptoms (n=47, 96% vs. 50% within 5 days, p=0.0005), shortened length of hospital stay (n=47, 5.7 vs. 7.8 days, p=0.046), decreased the number of patients needing invasive procedures (n=47, 0% vs. 18.2%, p=0.041) and decreased rate of recurrence at the 1-year mark.
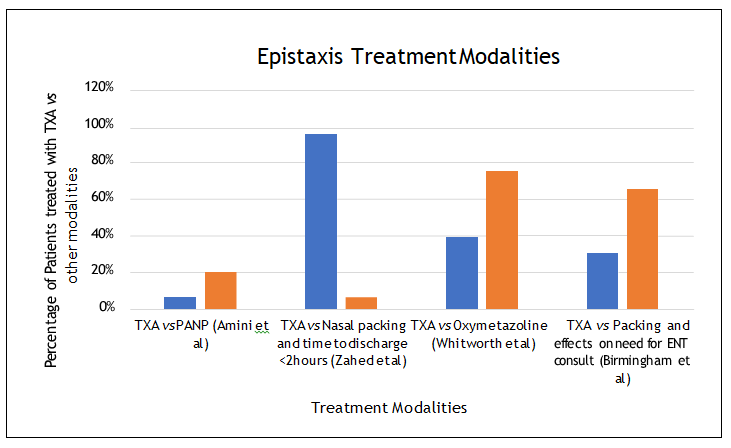
Numerous studies have looked at the benefit of using TXA off label for epistaxis (Figure 1). A metanalysis by Janapala, et al. compared the management of epistaxis by various modalities and concluded that not only patients that received TXA had significantly lower (3.5 times) rates of epistaxis recurrence (n=1299, 95% CI: 1.3-9.7), the TXA patients also were 63% less likely to return with recurrent epistaxis within 24-72 hrs (n=613, p=0.001) [2].
A retrospective multiyear review by Birmingham, et al. examined the benefits of TXA in patients with epistaxis and concluded that use of TXA decreased the need for otolaryngology consults (n=122, 30% vs. 65.2%, p=0.002) and need for nasal packing (n=122, 16.7% vs. 23.9%, p=0.003 respectively) when compared to other standard of care therapies [13].
Considering adverse risk profile, nasal packing is not only extremely uncomfortable for the patient, it can also cause nasal trauma if repeated. Furthermore, oxymetazoline is contraindicated in patients with hypertension and other common cardiovascular disease risk factors [3].
Figure 1: The rate of recurrence in epistaxis is compared between Tranexamic Acid (TXA), Phenylephrine-Lidocaine Nasal Packing (PANP), nasal packing and time to discharge (<2 hrs), oxymetazoline and requirement for otolaryngology consultation. The figure demonstrates that treatment with TXA leads to less rebleeding in patients and carries much shorter length of stay.
While oxymetazoline combined with nasal packing insertion is the most commonly used therapy in the emergent setting to control epistaxis, use of TXA is a growing trend. A prospective study by Whitworth, et al. concluded that 39% of TXA patients and 75% of oxymetazoline patients experienced recurrent hemorrhage (n=38, 95% CI) [14]. Furthermore, a randomized control trial by Zahed, et al. concluded that use of topical TXA instead of anterior nasal packing showed more efficacy in stopping the hemorrhage within 10 mins (n=216, 71% vs. 31.2%, p<0.001), lowered rates of recurrence (n=216, 4.7% vs. 11%, p=0.128), provided a quicker time to discharge (less than 2 hrs) (n=216, 95.3% vs. 6.4%, p<0.001), while increasing patient satisfaction (n=216, 8.5% vs. 4.4%, p<0.001) [8]. A similar prospective, double-blind, parallel-group, randomized clinical trial examined use of TXA versus Phenylephrine-Lidocaine Nasal Packing (PANP) where 6% of patients treated with TXA had recurrent bleeding, compared to 20% of patients treated with PANP (n=100, p=0.003) [15]. Numerous other studies evaluated effectiveness of TXA and variety of packing products came to similar statistical conclusions as seen in this trial [16,17].
Considering the increasing medical care costs, TXA is a reasonable option when compared to other modalities (Table 1). Relative costs for each modality were calculated based off average market prices and Relative Value Units (RVU) per Current Procedural Terminology (CPT) code for each option. While the TXA treatment option is the cheapest, when combined with significantly lower rates of recurrence compared to standard modalities including cost saving from reduced re-visits to emergency department and specialist involvement as well as improved patient satisfaction, the TXA should be the primary option for a clinician managing patients with epistaxis. Nebulized TXA should also be heavily considered in patients that have a financial or social limitation of follow-up with otolaryngology since TXA has a higher overall success rate when compared to other modalities.
Table 1: The approximate cost of different treatment modalities for epistaxis.
| Direct Cost of Epistaxis Treatment Modalities | ||
|---|---|---|
| Treatment modality | Breakdown of cost (Medicare) | Approximate cost |
| Nebulized tranexamic acid (100 mg/mL) 100 ml | Tranexamic acid [18]+CPT code 94640 [19] | $54.88 |
| Oxymetazoline 0.05% | Oxymetazoline [20]+CPT code 30901 [19] | $116.94 |
| Rapid Rhino® with saline | Rapid Rhino® [21]+CPT code 30903 [19] | $186.69 |
| Rapid Rhino® soaked with phenylephrine-lidocaine | Phenylephrine-lidocaine [22]+Rapid Rhino® [21]+CPT code 30903 [19] | $197.14 |
| Otolaryngologist evaluation | Office visit (99203) [19]+CPT code 31238 [19] | $246.29 |
Conclusions
- Tranexamic acid is the cheapest non-invasive option to control uncomplicated epistaxis.
- Use of nebulized TXA leads to lowest recurrence of hemorrhage when compared to standard treatment modalities.
- Tranexamic acid use in patients with epistaxis reduces overall healthcare costs and carries higher patient satisfaction.
References
- Newton E, Lasso A, Petrcich W, Kilty SJ (2016) An outcomes analysis of anterior epistaxis management in the emergency department. J Otolaryngol Head Neck Surg 45: 24.
[Crossref], [Google Scholar], [Indexed]
- Janapala RN, Tran QK, Patel J, Mehta E, Pourmand A (2022) Efficacy of topical tranexamic acid in epistaxis: A systematic review and meta-analysis. Am J Emerg Med 51: 169-175.
[Crossref], [Google Scholar], [Indexed]
- Hamlett KEL, Yaneza MMC, Grimmond N (2021) Epistaxis. Surgery 39: 577-590.
[Crossref], [Google Scholar]
- Hunt BJ (2015) The current place of tranexamic acid in the management of bleeding. Anaesthesia 70: 50-53.
[Crossref], [Google Scholar], [Indexed]
- Chauncey JM, Wieters JS (2022) Tranexamic Acid. In: StatPearls. Treasure Island (FL): StatPearls Publishing, USA.
- Joseph J, Martinez-Devesa P, Bellorini J, Burton MJ (2018) Tranexamic acid for patients with nasal haemorrhage (epistaxis). Cochrane Database Syst Rev 12: CD004328.
[Crossref], [Google Scholar], [Indexed]
- Gottlieb M, Koyfman A, Long B (2019) Tranexamic Acid for the Treatment of epistaxis. Acad Emerg Med 26: 1292-1293.
[Crossref], [Google Scholar], [Indexed]
- Zahed R, Moharamzadeh P, Alizadeharasi S, Ghasemi A, Saeedi M (2013) A new and rapid method for epistaxis treatment using injectable form of tranexamic acid topically: A randomized controlled trial. Am J Emerg Med 31: 1389-1392. [Crossref],
[Google Scholar], [Indexed]
- O'Neil ER, Schmees LR, Resendiz K, Justino H, Anders MM (2020) Inhaled tranexamic acid as a novel treatment for pulmonary hemorrhage in critically ill pediatric patients: An observational study. Crit Care Explor 2: e0075.
[Crossref], [Google Scholar], [Indexed]
- McCormack PL (2012) Tranexamic acid: A review of its use in the treatment of hyperfibrinolysis. Drugs 72: 585-617.
[Crossref], [Google Scholar], [Indexed]
- Erwin DZ, Heichel PD, Wright LM BS, Goldstein NA, McEvoy TP, et al. (2021) Post-tonsillectomy hemorrhage control with nebulized tranexamic acid: A retrospective cohort study. Int J Pediatr Otorhinolaryngol 147: 110802.
[Crossref], [Google Scholar], [Indexed]
- Wand O, Guber E, Guber A, Epstein Shochet G, Israeli-Shani L, et al. (2018) Inhaled tranexamic acid for hemoptysis treatment: A randomized controlled trial. Chest 154: 1379-1384.
[Crossref], [Google Scholar], [Indexed]
- Birmingham AR, Mah ND, Ran R, Hansen M (2018) Topical tranexamic acid for the treatment of acute epistaxis in the emergency department. Am J Emerg Med 36:1242-1245.
[Crossref], [Google Scholar], [Indexed]
- Whitworth K, Johnson J, Wisniewski S, Schrader M (2020) Comparative effectiveness of topically administered tranexamic acid versus topical oxymetazoline spray for achieving hemostasis in epistaxis. J Emerg Med 58: 211-216.
[Crossref], [Google Scholar], [Indexed]
- Amini K, Arabzadeh A, Jahed S, Amini P (2020) Topical tranexamic acid versus phenylephrine-lidocaine for the treatment of anterior epistaxis in patients taking aspirin or clopidogrel: A randomized clinical trial. Arch Acad Emerg Med 9: e6.
[Crossref], [Google Scholar], [Indexed]
- Akkan S, Çorbacioglu SK, Aytar H, Emektar E, Dagar S, et al. (2019) Evaluating effectiveness of nasal compression with tranexamic acid compared with simple nasal compression and merocel packing: A randomized controlled trial. Ann Emerg Med 74: 72-78.
[Crossref], [Google Scholar], [Indexed]
- Zahed R, Mousavi Jazayeri MH, Naderi A, Naderpour Z, Saeedi M (2018) Topical tranexamic acid compared with anterior nasal packing for treatment of epistaxis in patients taking antiplatelet drugs: Randomized controlled trial. Acad Emerg Med 25: 261-266.
[Crossref], [Google Scholar], [Indexed]
- https://www.drugs.com/price-guide/tranexamic-acid
- https://www.manninghammedicalcentre.com.au/w-medical/wv-medical-assistance-fee-schedule.html
- https://www.drugs.com/price-guide/oxymetazoline-nasal
- http://www.shopsps.com/shop/rr750-code-rr-750-smith-nephew-rapid-rhino-epistaxis-nasal-pac-7-5cm-ant-posterior-box-of-10-3230
- https://estore.healthfirst.com/product/lidocaine-hci-1-and-epinephrine-1-100-000-injection-usp-20ml-vial

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences