Chronic-Vomiting Induced Recurrent Spontaneous Pneumomediastinum: Case Report
Youssef Halhoul1*, Salaheddine El Miskini4, Mouaad Amraoui2, Sara Koualla3, Saad Zidouh4, Lahcen Belyamani4
1Department of Anesthesia and Intensive Care Unit, Mohamed V Military Training Hospital, Rabat, Morocco
2Department of Thoracic surgery, Mohamed V Military Training Hospital, Rabat, Morocco
3Department of Oral and Maxillofacial Surgery, Mohamed V Military Training Hospital, Rabat, Morocco
4Department of Emergency, Mohamed V Military Training Hospital, Rabat, Morocco
- *Corresponding Author:
- Youssef Halhoul
Department of Anesthesia and Intensive Care Unit,
Mohamed V Military Training Hospital, Rabat,
Morocco,
E-mail: youssefhalhoul2@gmail.com
Received date: June 29, 2022, Manuscript No. IPMCRS-22-14159; Editor Assigned date: July 01, 2022, PreQC No. IPMCRS-22-14159 (PQ); Reviewed date: July 13, 2022, QC No. IPMCRS-22-14159; Revised date: July 22, 2022, Manuscript No. IPMCRS-22-14159 (R); Published date: August 01, 2022, DOI: 10.36648/2471-8041.8.7.236.
Citation: Halhoul Y, Miskini SE, Amraoui M, Koualla S, Zidouh S et al. (2022) Chronic-Vomiting Induced Recurrent Spontaneous Pneumomediastinum: Case Report. Med Case Rep Vol.8 No.7: 236.
Abstract
In contrast to secondary pneumomediastinum who has an identifiable cause, spontaneous pneumomediastinum is a rare clinical entity defined as the presence of free air in the mediastinal structures not associated with trauma. Its main causes are vomiting, exercise, drugs, asthma, difficult labour and valsalva maneuvers. Its classic clinical presentation is retrosternal chest pain, dyspnoea and subcutaneous emphysema. Chest X-ray or ideally a chest CT scan confirms the diagnosis. Before retaining the spontaneous character of the pneumomediastinum, several investigations should be carried out in order to detect an obvious cause such as iatrogenic or traumatic perforation of the oesophagus, trachea, or respiratory tract and intrathoracic infection. The prognosis is usually excellent without specific treatment and the recurrences are poorly described in the literature. We report the case of a 30-year-old female patient presenting dyspnoea, chest pain and facial swelling with a history of chronic vomiting over the past year and two previous episodes of similar symptomatology and who was diagnosed with recurrent spontaneous pneumomediastinum.
Keywords
Vomiting; Spontaneous; Pneumomediastinum; Recurrent
Introduction
Pneumomediastinum is defined as the presence of free air in the mediastinum. The diagnosis is confirmed by radiology. Pneumomediastinum can be divided into two groups of patients: Spontaneous pneumomediastinum, without any obvious primary source and secondary pneumomediastinum, with a specific responsible pathologic event, such as trauma, intrathoracic infections, or perforation of the aerodigestive track [1].
Firstly described by Louis Hamman in 1939 [2], spontaneous pneumomediastinum or Hamman’s syndrome is a benign condition, presenting in young male adults exposed to a sudden pressure change within the intrathoracic cavity [3]. Its incidence has been reported as occurring in 1 in 800 to 1 in 42,000 hospital admissions [4]. Vomiting-induced pneumomediastinum can be a result of barotrauma causing alveolar rupture or Boerhaave’s syndrome [5]. In Boerhaave’s syndrome, evidence of oesophageal perforation by extravasation of contrast after ingestion of gastrografin is essential. Unlike these diagnosis criteria, we report the case of a 30-year-old female patient presenting dyspnoea, chest pain and facial swelling during vomiting effort and who was diagnosed with spontaneous pneumomediastinum because of the absence of any source proving tracheal tor airway injury as well as oesophageal rupture. We would also like to point out the recurrent nature of this spontaneous pneumomediastinum, which is rarely described in the literature, as our patient had two previous episodes of identical symptoms.
Case Presentation
A 30-year-old female patient presented to the emergency department with sudden onset of dyspnoea associated with chest pain and cervico-facial swelling during an episode of vomiting.
Patient’s medical history shows recurrent vomiting with transit disorders due to chronic gastritis on omeprazole and antiemetic.
The patient presented two episodes of similar symptomatology during the previous 3 months and did not have any medical check-up with spontaneous improvement after a few days.
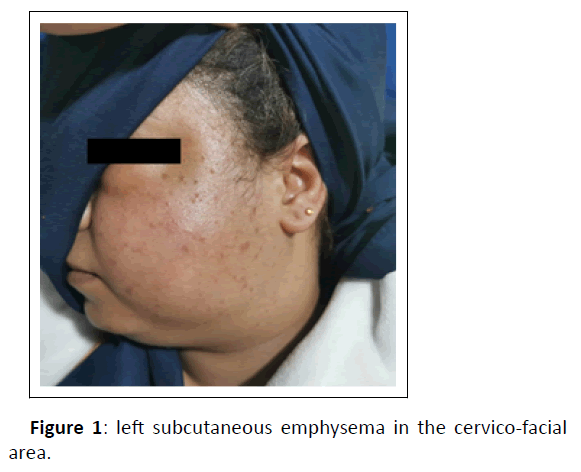
Vital signs were within the normal range. Physical examination showed mild tachypnoea with no stridor, left subcutaneous emphysema in the cervico-facial area (Figure 1) with soft tissue crepitus, normal bilateral ventilation and a soft abdomen. No visible injury to the thorax could be detected.
Blood tests revealed a haemoglobin level of 10.5 g/dL (normal range 12–15 g/dL) and white blood cell count of 12000/mm3 (normal range 4–10 × 109/L). Serum urea, creatinine and electrolytes were normal despite hypokalemia at 3.1 mmol/L (normal range 3.5–5.1 mmol/L) explained by prolonged vomiting.
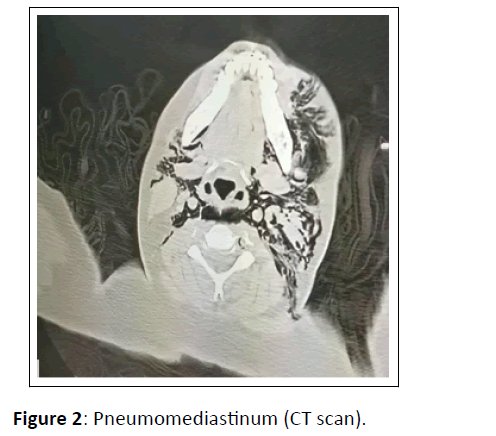
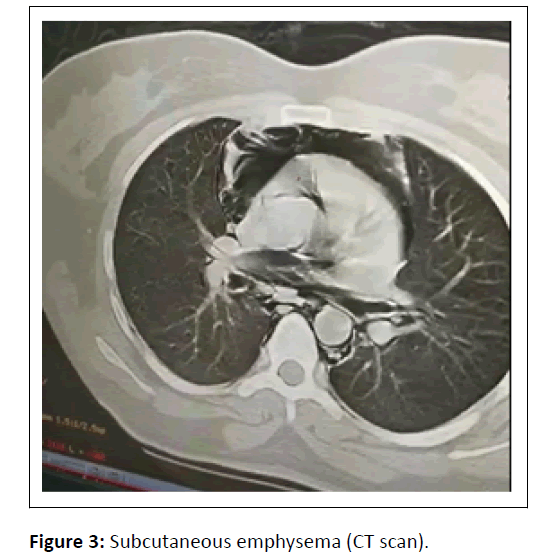
An enhanced Computed Tomography (CT) scan of the neck and chest was performed, revealing extensive pneumomediastinum (Figure 2) and subcutaneous emphysema (Figure 3). A gastrografin swallow showed no extravasation of contrast eliminating the diagnosis of Boerhaave’s syndrome. Imaging and bronchoscopy did not reveal a tracheal tear or airway injury
The patient was commenced on antibiotics, intravenous fluids and antiemetics and kept nil by mouth. Her condition improved quickly. She was discharged 8 days later. Ambulatory follow-up was planned with no recurrence.
Discussion
Spontaneous pneumomediastinum results from alveolar rupture rather than gastrointestinal leak, it occurs due to bronchial hyper-reactivity or barotrauma, the latter of which can be induced by coughing or vomiting. Alveolar rupture allows air to be drawn into the mediastinum down a pressure gradient [5].
However, the presence of a triggering factor, such as vomiting, points much more towards a diagnosis of Boerhaave’s syndrome, which is a transmural perforation of the oesophagus.
The distinction between the two diagnoses is not easy and is based primarily on post contrast CT imaging showing direct contrast leakage/tracks and oesophageal wall thickening in Boerhaave’s syndrome in contrast to spontaneous pneumomediastinum [6].
Several case reports suggest that vomiting-induced pneumomediastinum does not always indicate oesophageal rupture [7,8].
Another criterion that may point to Boerhave’s syndrome rather than spontaneous pneumomediastinum is the evolution of the symptomatology towards mediastinitis, which is usually a consequence of oesophageal perforation or iatrogenic causes. Mediastinitis can occur following secondary pneumomediastinum, but is not typically seen following spontaneous pneumomediastinum [9]. This is supported by Ebina et al. [10], who reviewed 34 cases of spontaneous pneumomediastinum and found that none developed mediastinitis.
Concerning our patient and the progression of the symptomatology, the diagnosis of spontaneous pneumodmediastinum is retained given the absence of any contrast leakage after gastrografin swallow and no evidence of mediastinis.
Our patient presented two episodes of similar symptomatology during the previous 3 months, and did not have any medical check-up with spontaneous improvement after a few days, which may suggest episodes of recurrent spontaneous pneumomediastinum.
Recurrent spontaneous pneumomediastinum is an exceptional event and little is known about it, in English literature only three cases of recurrent spontaneous pneumomediastinum are reported. It seems reasonable to think that recurrences of spontaneous pneumomediastinum are facilitated by the persistence of predisposing factor [11], such as vomiting for our case.
Therapeutic management consists of close monitoring combining rest, analgesics and oxygen therapy in case of dyspnoea. Antibiotic coverage, generally by third generation cephalosporin, is recommended [7]. Fasting is not systematic. The duration of hospitalisation varies between 3 and 7 days [12].
Our patient’s condition improved quickly. She was discharged 8 days later. Ambulatory follow-up was planned with no recurrence.
The management of the triggering factor seems to reduce or even avoid any recurrence. Our patient, after treatment of the gastritis responsible for vomiting, had a follow-up for 18 months without any recurrence.
Conclusion
Spontaneous pneumomediastinum is a rare and benign entity. Its management and prognosis are different from Boerhave’s syndrome. Before retaining the diagnosis of spontaneous pneumomediastinum, it is necessary to exclude the presence of a digestive or tracheal damage. Chest Computed Tomography (CT) is very used for the diagnosis and also for monitoring the progress of patients. The management of the triggering factor is a milestone to avoid recurrences.
Consent
Written informed consent was obtained from the patient’s family to publish this case report and any accompanying images. No institutional approval was required to publish the case report.
References
- Caceres M, Ali SZ, Braud R, Weiman D, Garrett HE (2008) Spontaneous pneumomediastinum: A comparative study and review of the literature. Ann Thorac Surg 86: 962‑966.
[Crossref], [GoogleScholar], [Indexed]
- Ito S, Takada Y, Tanaka A, Ozeki N, Yazaki Y (1989) A case of spontaneous pneumomediastinum in a trombonist. Kokyu To Junkan 37: 1359‑62.
[Crossref], [GoogleScholar], [Indexed]
- Gerazounis M, Athanassiadi K, Kalantzi N, Moustardas M (2003) Spontaneous pneumomediastinum: A rare benign entity. J Thorac Cardiovasc Surg 126: 774‑6.
[Crossref], [GoogleScholar], [Indexed]
- Newcomb AE, Clarke CP (2005) Spontaneous pneumomediastinum: A benign curiosity or a significant problem? Chest 128: 3298‑302.
[Crossref], [GoogleScholar], [Indexed]
- Kyriakides J, Stackhouse A (2020) Vomiting-induced pneumomediastinum as a result of recurrent Boerhaave’s syndrome. J Surg Case Rep 2020: rjaa102.
[Crossref], [GoogleScholar], [Indexed]
- Spontaneous pneumomediastinum: A comparative study and review of the literature
- Al-Mufarrej F, Badar J, Gharagozloo F, Tempesta B, Strother E, et al. (2008) Spontaneous pneumomediastinum: Diagnostic and therapeutic interventions. J Cardiothorac Surg 3: 59.
[Crossref], [GoogleScholar], [Indexed]
- Forshaw MJ, Khan AZ, Strauss DC, Botha AJ, Mason RC (2007) Vomiting-induced pneumomediastinum and subcutaneous emphysema does not always indicate Boerhaave’s syndrome: Report of six cases. Surg Today 37: 888‑92.
[Crossref], [GoogleScholar], [Indexed]
- Pierce TB, Razzuk MA, Razzuk LM, Luterman DL, Sutker WL (2000) Acute mediastinitis. Proc Bayl Univ Med Cent 13: 31‑3.
[Crossref], [GoogleScholar], [Indexed]
- Ebina M, Inoue A, Takaba A, Ariyoshi K (2017) Management of spontaneous pneumomediastinum: Are hospitalization and prophylactic antibiotics needed? Am J Emerg Med 35: 1150‑3.
[Crossref], [GoogleScholar], [Indexed]
- Fiorelli A, Messina G, Capaccio D, Santini M (2012) Recurrent spontaneous pneumomediastinum: A rare but possible event! J Thorac Dis 4: 431‑3.
[Crossref], [GoogleScholar], [Indexed]
- Takada K, Matsumoto S, Hiramatsu T, Kojima E, Shizu M, et al. (2009) Spontaneous pneumomediastinum: An algorithm for diagnosis and management. Ther Adv Respir Dis 3: 301‑7.
[Crossref], [GoogleScholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences