Central Pontine Myelinolysis, Osmotic Demyelination Syndrome Due to Rapidly Decreased Fluid Intake in a Schizophrenic Patient with Psychogenic Polydipsia: A Case report and Review of The Literature
Hamza M Alsaid and Anis M Naser
Hamza M Alsaid1* and Anis M Naser2
1Al-Quds College of Medicine, Jerusalem, Palestine, Israel
2Department of Neurology, Al-Makassed Islamic Charitable Hospital, Jerusalem, Palestine, Israel
- *Corresponding Author:
- Hamza Mohammad Alsaid
Al-Quds College of Medicine
P.O Box. 17233, Jerusalem, Israel
Tel: +972599042495
E-mail: hamza.m.alsaid@gmail.com
Received Date: December 02, 2018; Accepted Date: January 18, 2019; Published Date: January 22, 2019
Citation: Alsaid HM, Naser AM (2019) Central Pontine Myelinolysis, Osmotic Demyelination Syndrome Due to Rapidly Decreased Fluid Intake in a Schizophrenic Patient with Psychogenic Polydipsia: A Case report and Review of The Literature. Med Case Rep Vol.5 No.1:89.
Abstract
Central pontine myelinolysis is a rare entity of osmotic demyelinating disease that mostly affects the basis pontis in brainstem. The clinical picture of central pontine myelinolysis can be variable and mixed, manifestations such as pseudobulbar palsy, various degrees of spastic paraparesis and tetraparesis, ataxia and diminished deep tendon reflexes can all occur. Etiology of central pontine myelinolysis has been reported to be mostly attributed by rapid changes in serum osmolality. Magnetic Resonance Imaging is the only way to confirm the diagnosis of central pontine myelinolysis. In this report, we describe an unusual case of central pontine myelinolysis in a 39 years old male patient who had a long-standing history of psychogenic polydipsia, compulsive water intake associated with schizophrenia that was referred to our hospital for deteriorating level of consciousness and generalized weakness after a sudden decrease in his oral water intake and sudden withdrawal of lithium treatment. We review this uncommon etiology of central pontine myelinolysis in the patient as well as pathophysiological mechanisms involved.
Keywords
Central Pontine Myelinolysis (CPM); Osmotic demyelination syndrome; Hyponatremia; Hypernatremia; Psychogenic polydipsia
Introduction
Central pontine myelinolysis (CPM) is a non-inflammatory demyelinating disease that affects the central portion of the base of pons. Sometimes, demyelination of other areas of the Central Nervous System can be also associated; this is referred to as Extrapontine Myelinolysis (EPM). The term; ‘Osmotic Demyelination syndrome (ODS)’ can include both extrapontine and pontine demyelination and reflects to serum osmolality as an etiological factor for the disease [1].
The first clinical description of Central Pontine Myelinolysis dates back to 1949 when Victor and Adams described an Alcoholic 38 years old patient that had developed quadriplegia, pseudobulbar palsy and dysphagia. The patient’s post-mortem showed a demyelinating lesion in the basis pontis. In 1959 the concept of Central Pontine Myelinolysis (CPM) was introduced, when Adams further described three more patients with symmetrical butterfly-like lesions located in basis pontis [2].
The exact incidence of CPM is unknown; a review by Singh on liver transplant patients’ neurological complications showed that CPM was found in 11% of liver transplant recipients, two thirds of them had disturbances in Sodium levels [3]. In a study among ICU patients, it was also reported that Isolated CPM was in 41% of patients and combined pontine, and extra-pontine lesions were found in 23% of cases [4]. In a report of 58 cases, 27 cases had an isolated CPM, 13 had exclusively EPM and 18 had combined CPM and EPM [5].
Etiology of CPM can be variable, it includes many etiological factors; Alcoholism and malnutrition have been reported in literature as common associations with CPM. Psychogenic Polydipsia (especially if chronic), burns, prolonged diuretic use, post liver transplant and to a lesser extent; post pituitary surgery, all have been reported [6]. Tomlinson in 1976 was credited with the suggestion that the rapidity of correction of Sodium was the main etiological factor [7]. In regard to the clinical picture associated with CPM, patients can present with different manifestations, such as; spastic tetraparesis, the locked-in syndrome, pseudobulbar paralysis and coma [8].
We report the case of a 39-year-old male patient who exhibited Central Pontine Myelinolysis and has long standing history of schizophrenia associated with psychogenic polydipsia and compulsive water drinking, for which the patient was maintained on Lithium treatment for 8 years. We discuss the role of psychogenic polydipsia, hyponatremia correction and lithium in the onset of CPM in this case, as well as the pathophysiological mechanisms involved.
Case Report
A 39-year-old male single patient was Referred to our Internal Medicine and Neurology Department at Al-Makassed Hospital, Jerusalem for generalized weakness, decreased level of consciousness with progressive deterioration, the patient is known to have schizophrenia for the last 8 year that was associated with psychogenic polydipsia associated with a daily water intake of approx. 12 liters per day, for which he was maintained on; lithium 600 mg/day, Valproic Acid 500 mg/day and Risperdal 3 mg/day. It is worthy of noting that the patient had base line hyponatremia, sodium level before the onset of any events was 126 mEq/L.
The patient was in his usual state of health, with unlimited exercise intolerance and able to do daily life activities, until six days days Before the admission when the patient developed fever of 38°C that lasted for two days, the patient was evaluated in a peripheral medical center and was treated for Community acquired Pneumonia that resolved with IV Antibiotics. Lithium, Valproic acid and Risperdal where stopped due to suspicion of Neuroleptic Malignant Syndrome. During this period, the patient decreased daily oral fluid intake to approx. 3 Liters of water, one day before the admission to our hospital; the patient started to have generalized weakness, with progressive deterioration in his level of consciousness, for which the patient was referred to our hospital.
On Admission, the patient had decreased level of consciousness, emerging dysphagia and flaccid tetraplegia, there was no history of ataxia, urinary or fecal incontinence. There was no history of chest pain or palpitations or respiratory distress. On physical exam, the patient was stuporous, unresponsive to verbal stimuli with mild response to painful stimuli in the form of grimacing, Pupils were reactive to direct and indirect light. Vestibulo–ocular reflex was intact on both left and right. Deep Tendon Reflexes where absent with flaccid muscle tone. We observed no involuntary movements, a full Cranial Nerve Examination was not assessable. Lungs and thorax; normal shape and contour No wheezes or added sounds, No mass or organomegaly on abdominal examination.
The patient’s vital signs were of the following values on admission: Temperature 36.2°C, Pulse Rate 80 BPM, Blood Pressure 150/80, Oxygen Saturation 88%. The patient was evaluated by the following lab work; Complete Blood Count was of normal values. Serum Electrolytes testing revealed Hypernatremia with a Serum Sodium level of 157 mEq/L and normal other electrolytes. Arterial Blood Gases testing was of normal values; PH 7.41, Bicarbonate 24 mEq/L, PaCO2 39 mmHg. Lumbar Puncture was done and had normal values. The patient was admitted to the Intensive Care Unit due to Desaturation and was intubated.
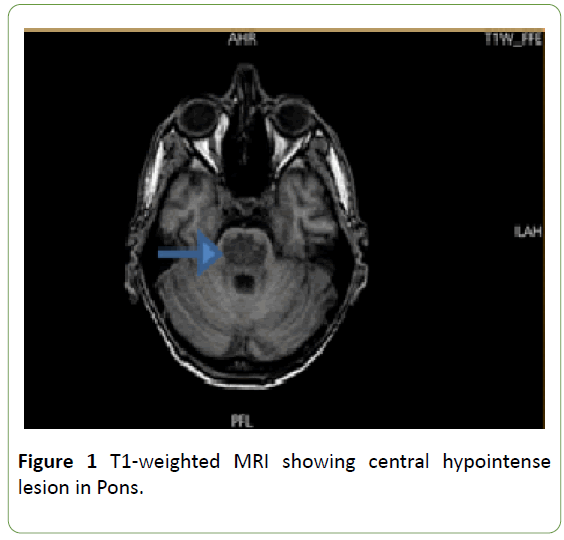
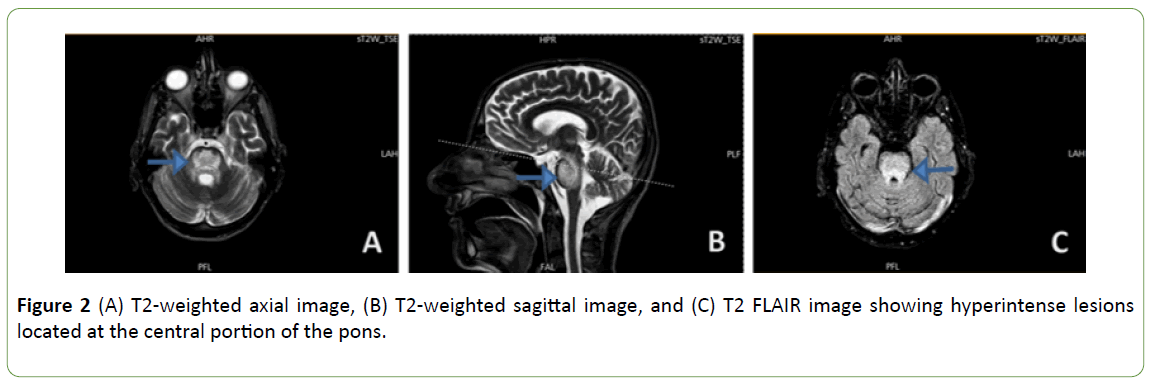
Magnetic resonance imaging (MRI) examination was done and revealed a Central hypointense lesion on Axial T1- weighted imaging (Figure 1), Sagittal and coronal T2-weighted Imaging along with FLAIR showed hyperintense lesions in the central pons (Figures 2A, 2B and 2C). Findings were consistent with Central Pontine Myelinolysis.
Management for this patient’s Central Pontine Myelinolysis focused on the correction of Hypernatremia that went up to 168 mEq/L during the first day of admission. Over the patient’s ten-day admission to the Intensive Care Unit, hypernatremia was corrected to 136 mEq/L, the patient was then transferred to the Internal Medicine Ward and admitted for two weeks during which the patient had a close follow up, but unfortunately the patient remained in persistent vegetative state without improvement in his physical exam. The patient was then discharged to a Rehabilitation Center and will continue his lifelong follow up with a neurologist.
Discussion
Central Pontine Myelinolysis is a rare entity of disease that is characterized by a non-inflammatory demyelination of oligodendrocytes of the basis pontis [6] Mostly, Central Pontine Myelinolysis lesions are usually symmetrical and bilateral [2]. Demyelination can also affect other parts of the brain, in Extrapontine Myelinolysis (EPM); Hippocampus, Putamen, cerebral cortex, thalamus, cerebellum, lateral geniculate body, external capsule lesions can also be included [6]. The term ‘Osmotic demyelination syndrome’ is used to describe CPM and EPM since both carry similar pathophysiology, time course and associations [1].
Several Etiologies and factors have been reported to contribute in causing central pontine myelinolysis, rapid correction of hyponatremia seems to be a major factor, the rate of hyponatremia correction is essential as a cause of CPM, as it was noted that slow correction of Hyponatremia did not trigger CPM [9].
From our point of view, the most interesting aspect in this case is the unusual etiology of CPM. Our patient has had psychogenic polydipsia and Schizophrenia for 8 years with a compulsive daily water intake of approx. 12 Liters, and it has been reported that patients with compulsive water drinking can develop hyponatremia [10]. Reviewing the patient’s medical record, the patient sustained a history low sodium levels of 126 mEq/L before his hypernatremic state on admission.
The exact mechanism of hyponatremia in psychiatric patients with excessive compulsive drinking in not fully understood, some studies revealed that it could be due to defective sensitivity to the actions of Vasopressin, And a reduced osmotic threshold for vasopressin secretion in psychiatric patients with polydipsia and hyponatremia [11].
We believe that the cause of this patient’s rapid rise in sodium levels was due to the sudden decrease in water intake after the previous admission, and since the patient had a history of hyponatremia, the rapid decrease in water intake thus produced an osmotic demyelination syndrome of CPM as observed in our patient. From a pathophysiological point of view, when serum sodium levels drop and serum osmolality decreases, water will enter brain cells causing their edema. However, cells have a protective mechanism against edema especially in the setting of chronic hyponatremia, by releasing organic osmoles; cells can adjust their cellular osmolality. This is a form of slow adaption that can only help balance a decrease in serum osmolality. Thus, if the serum plasma sodium osmolality is rapidly corrected causing a quick rise in serum osmolality, this will lead to failure of this protective mechanism. As the rate of rise in tonicity exceeds the rate of release of organic osmoles, brain cells, especially oligodendrocytes will shrink and be at the risk of myelinolysis [6].
We also considered another etiological aspect for our patient’s hypernatremia and CPM, and that is Lithium treatment. The effect of Lithium treatment on CPM is still controversial. While it has been reported that CPM and EPM were caused by lithium toxicity in a pregnant woman [12]. CPM was reported by Swartz in the setting of rapid drop in serum lithium levels after a gradual increase in its levels, as such rapid change is associated with neuronal injury. From a physiological point of view, lithium moves sodium into the cells, and high lithium levels can cause intra-neuronal sodium depletion, thus rapid discontinuation of Lithium might cause intra-cellular hyponatremia which could be rapidly corrected in a similar picture of a rapid correction of hyponatremia, thereby causing demyelinating brain lesions such as CPM [13-15]. Unfortunately, our limitation was that we did not have any measurements of serum lithium levels in this patient.
Since there might be involvement of ascending and descending tracts in brainstem [16], the clinical picture of CPM can be very variable, the main symptoms are usually, disturbed consciousness, pseudobulbar palsy, psychiatric manifestations, dysarthria and dysphagia, various degrees of spastic paraparesis and tetraparesis, ataxia and seizures. Physical signs might include; diminished or absent deep tendon reflexes, lethargy and hypotension. In extreme cases, a ‘locked-in syndrome’ can also be seen [8]. Our patient had decreased level of consciousness, emerging dysphagia and flaccid tetraplegia as well as absent deep tendon reflexes on physical exam. This correlates well with the clinical signs and symptoms of CPM.
Along with the clinical picture this disease, CPM diagnosis is confirmed via Magnetic Resonance Imaging (MRI), MRI can reveal the extent and number of the pontine demyelinating lesions, the classical MRI findings are hypointense demyelinating lesions on T1-weighted imaging acutely, and hyperintense demyelinating lesions on T2-weighted imaging subacutely [17]. Our patient had hyperintense lesions on T2- weighted imaging and hypointense lesions on T1-weighted imaging as well as.
In regards to management of CPM, there is no treatment of choice, general therapeutic measures and supportive treatments focus on correction of any electrolyte imbalance, prevention of pneumonia and thrombotic events, as well as ensuring adequate caloric intake [1]. Concerning hyponatremia correction, the rate of correction in acute symptomatic hyponatremia is recommended to be 1±2 mmol/l/h. As for hypernatremia correction, if the hypernatremia is acute and symptomatic, sodium levels could be lowered as fast as 1 mmol/l/h, if the hypernatremia has a chronic course, the rate of sodium correction should be not more than 0.5 mmol/l/h [17]. Our patient’s acute symptomatic hypernatremic state was corrected according to guidelines at the rate of 0.5 mmol/l/h.
The prognosis in Central pontine myelinolysis can be variable and mixed. In a series of 34 cases, death was reported in 2 patients, 10 survived but were left dependent, 11 had deficits but were independent and 11 had a complete recovery [18]. In another retrospective observational study in French Intensive Care Units and after a 1 year follow up. It was reported that among 36 patients of CPM and EPM, 11 (31%) had died [19]. Hence, outcomes of CPM may vary from death and disability to recovery to a relatively normal level of function.
Conclusion
In conclusion, Central pontine myelinolysis is a rare complication of rapid correction of serum osmolality, identifying and predicting which patients might be at the risk of central pontine myelinolysis is a cornerstone in preventing any neurological injury that might ensue. We believe that Specific care should be considered for psychiatric patients with longstanding psychogenic polydipsia and impulsive water intake, as these patients may develop a chronic state of hyponatremia which makes them vulnerable to osmotic demyelinating disease. There is lacking evidence on the effect of lithium on CPM, but we think that the rapid decrease in water intake as well as the rapid removal of high lithium levels from the serum after a gradual increase might have caused a quick rise in serum sodium and thus, an osmotic demyelinating disease in this observation.
Since CPM could be avoided by good monitoring and control of serum osmolality and electrolytes, clinicians should always be aware of this complication, especially in patients with multiple risk factors. Fortunately, a better understanding of the pathophysiology of osmotic demyelination has allowed for more rational intervention and improved prognosis.
Acknowledgements
We would like to express our sincere thanks for Dr. Muayad Salman, M.D., Pediatric Radiologist at Al-Makassed Islamic Charitable Hospital, Jerusalem. For his help in reporting the MRI findings in our case report. This case report was selected for presentation and discussion at the Medical scientific symposium of 2019 at Al-Quds University, Jerusalem.
References
- Lampl C, Yazdi K (2002) Central pontine myelinolysis. Euro Neurol 47: 3-10.
- Adams RD, Victor M, Mancall EL (1959) Central pontine myelinolysis: a hitherto undescribed disease occurring in alcoholic and malnourished patients. AMA Arch NeurPsych 81: 154-172.
- Singh N, Yu VL, Gayowski T (1994) Central nervous system lesions in adult liver transplant recipients: A clinical review with implications for management. Med 73: 110-110.
- Rao PB, Azim A, Singh N, Baronia AK, Kumar A, et al. (2015) Osmotic demyelination syndrome in Intensive Care Unit. Indian J Crit Care Med 19: 163-166.
- Gocht A, Colmant HJ (1987) Central pontine and extrapontine myelinolysis: a report of 58 cases. Clin Neuropathol 6: 262-270.
- Martin RJ (2004) Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry 75: 22-28.
- Tomlinson BE, Pierides AM, Bradley WG (1976). Central pontine myelinolysis: Two cases with associated electrolyte disturbance. Q J Med 45: 373-386.
- Pirzada NA, Ali II (2001) Central pontine myelinolysis. In Mayo Clinic Proceedings 76: 559-562.
- Laureno R (1983) Central pontine myelinolysis following rapid correction of hyponatremia. Ann Neurol 13: 232-242.
- Cronin RE (1987) Psychogenic polydipsia with hyponatremia: report of eleven cases. Am J Kidney Dis 9: 410-416.
- Goldman MB, Luchins DJ, Robertson GL (1988) Mechanisms of altered water metabolism in psychotic patients with polydipsia and hyponatremia. N Engl J Med 318: 397-403.
- Bejot Y, Depierre P, Osseby GV, Troisgros O, Moreau T, et al. (2008). Central pontine and extra-pontine myelinolysis: A complication of lithium toxicity in a pregnant woman. Clin Neurol Neurosurg 110: 852-854.
- Swartz CM (1996) Encephalopathy Associated with Rapid Decrease of High Levels of Lithium. Ann Clinical Psychiatry 8:111-112.
- Swartz CM (2003) Central pontine myelinolysis and lithium toxicity. Ann Clin Psychiatry 15: 133-133.
- Swartz CM, Dolinar LJ (1995) Encephalopathy associated with rapid decrease of high levels of lithium. Ann Clin Psychiatry 7: 207-209.
- Messert B, Orrison WW, Hawkins MJ, Quaglieri CE (1979) Central pontine myelinolysis Considerations on etiology, diagnosis, and treatment. Neurology 29: 147-160.
- Brown WD (2000) Osmotic demyelination disorders: central pontine and extrapontine myelinolysis. Curr Opin Neurol 13: 691-697.
- Menger H, Jörg J (1999) Outcome of central pontine and extrapontine myelinolysis. J Neurol 246: 700-705.
- Louis G, Megarbane B, Lavoué S, Lassalle V, Argaud L, et al. (2012) Long-term outcome of patients hospitalized in intensive care units with central or extrapontine myelinolysis. Crit Care Med 40: 970-972.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences