Blind Approach Posterior Tampon with Foley Catheter for Mallampati Class IVPatient during Covid19 Pandemic Era
Rusly*, Sy Bellia Kharisma
Rusly*, Sy Bellia Kharisma
Department of A&E, Murni Teguh Memorial Hospital, Medan, North Sumatera, Indonesia
*Corresponding author: Rusly, Department of A&E, Murni Teguh Memorial Hospital, Medan, North Sumatera, Indonesia, Tel No: 08126526065; E-mail: dr.rusly@gmail.com
Received date: December 06, 2020; Accepted date: January 18,2022; P u blished date: January 25, 2022
Citation: Rusly (2022) Blind Approach Posterior Tampon with Foley Catheter for Mallampati Class IV Patient during Covid19 Pandemic Era. Med Case Rep Vol: 8 No: 1.
Abstract
Epistaxis is one of the common emergencies with many risk factors and causes, one of the main cause is due to neoplasm. Forty-eight years old male admitted to ER with nassal bleeding for 30 minutes. Blood lost was estimated 1500-2000 cc. He has history of nasopharingeal carcinoma. In ER, patient’s airway was managed, fluid ressuscitation and bleeding was controlled by posterior tampon with a foley catheter. After the patient is stabilized, patient received further treatment. Posterior tampon is common procedure for treating posterior epistaxis in Emergency Room and foley catheter is used in most emergency room settings. Visual references require physician to see the tip of the foley catheter before inflating the catheher balloon. However, this step might be a challange in patient with mallampati class III-IV which visualization to hypopharynx is limitted or in Covid19 Pandemic Era which chance to receive patient with covid19 disease is possible and aerosolization procedure should be done in shorter time.
Keywords: Epistaxis; Posterior tampon; Foley catheter; Covid19 pandemic
Introduction
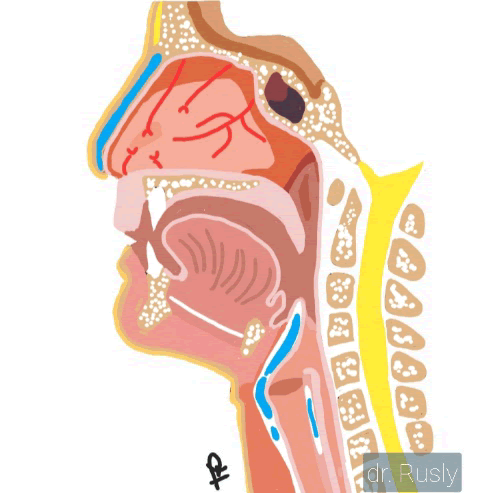
Epistaxis is an extremely common condition in ER with an incidence estimated at 60% and 10% could be serious and life threatening.1 Based on its characteristic, epistaxis posterior is common in older population. It may be the first sign of sin nasal problem. Woodruff plexus that supply most nasal mucosa posteriorly arises from internal maxillary artery, a branch of external carotid system.1 Due to its anatomical position, posterior epistaxis can also manifest as massive hemorrhage that is extremely difficult to control and cause dangerous.
condition such as aspiration of blood into the airways, anemia and leading to shock. Improper handling of epistaxis can worsen the patient’s condition.
Posterior epistaxis can arises from local factor like direct trauma, neoplasm or even more systemic disorder including medication.
Diagnosing massive posterior epistaxis might not be difficult but determining wether unilateral or bilateral nassal might be a challenge, especially in most emergency room setting. Laboratory findings such as haemoglobin, platelet and coagulation studies are always helpful if situation allows.1,2
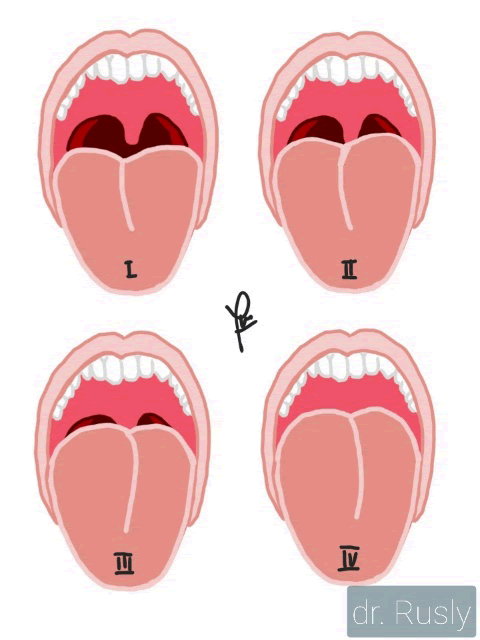
Mallampati classification by visualize hypopharynx may be helpful in diagnosing posterior epistaxis. As part of LEMON assessment for difficult airway, mallampati classification are classified into 4 classes.3
As dangerous conditions that commonly happend, life support must be prioritized in management of posterior epistaxis, including airway management and circulation status.
| Class I (15%) | Class II (15-30%) | Class III (30-40%) | Class IV (>40%) | |
|---|---|---|---|---|
| Blood Loss | -750 | 750- 1500 | 1500-2000 | >2000 |
| Systolic | normal | normal | ↑ | ↑ |
| Pulse Pressure | normal/↑ | ↓ | ↓ | ↓ |
| HR | <100 | 100-120 | 120-140 | >140 |
Table 1: Haemorrhage Classification (estimation for 70 kg male)3.
Basic bleeding management is aiming to stop the bleeding, epistaxis posterior could be managed by hemostatic agents, placing posterior tampon and interventional surgery. Infection must be considered after procedure. Eventhough posterior tampon’s failure rate approaching 40% but it can be done in most emergency room setting unlike surgical treatment or embolization.1 But close monitoring patient condition can also prevent unwanted condition.
Posterior tampon can be managed by inserting belloq tampon but it may be difficult and requires preparation. As alternative, a double balloon catheter is easier but they are expensive and might not be available in every Emergency Room. Expandable nassal sponge might be inexpensive and easy but it might be ineffective if used alone.2
Alternatively, folley catheter technique may be used to provide a posterior buttress. It is easy, simple and inexpensive.
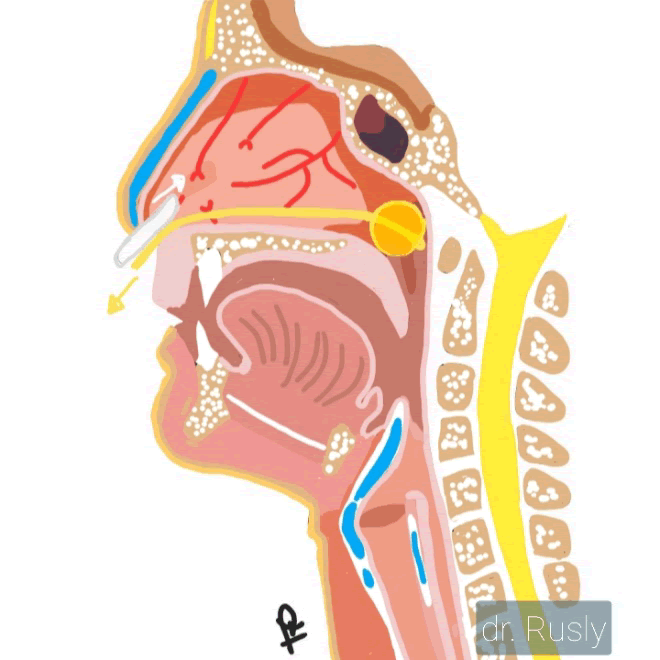
The procedure as following: 2
- Insert a foley catheter no.14 Fr that has been applied gel until visible in the nasopharynx
- Inflated it with 7-10 mL of air and avance it back to nasopharynx
- Add another 3 to 5 mL of air till it lodges against choanal arch
- Place anterior pack and secure the foley catheter
Other alternative of this technique is inflate the baloon with 5-15 mL of normal saline.4
Postnasal tampon requires hospitalization and should be retained for about 24-48 hours.4
COVID19 has been a pandemic in the world since early 2020. WHO declare this disease needs airborne precaution so performing aerosol generating procedure required appropriate PPE and negative pressure single room setting. Caring patient with suspected and confirmed Covid19 that have underlying noncommunicable diseases to continue or modify previous medical therapy according patient’s clinical conditions. A trained and experience provider using airborne precaution is recommended.5
Case
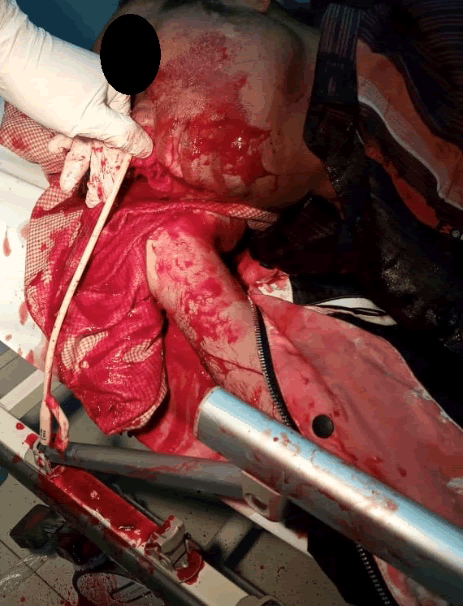
A 48 year old male patient admitted to the emergency room with active bleeding coming out from both sides of the nose for 30 minutes. The bleeding was massive as the patient's clothes and ER triage floor wet with blood. The patient looks very pale and apparently in shock. Patient was soon transferred to the closed resuscitation room. While resuscitation was made, the patient's wife told the other ER staff that he was nasopharynx malignant neoplasm and 6 months- post treatment. From the primary survey, he was conscious but very weak in response.
The patient's vital signs came out as blood pressure 83/67 mmHg, pulse 128x/i, respiratory rate 24x/i, temperature 36.7c oxygen saturation 89-94%. The extremities were cold and conjuntiva palpebra inferior was pale. No gargling or stridor in this patient but as massive blood kept coming out from his mouth, patient was positioned in left lateral decubitus to prevent blood aspirated into lung. He also received 2000cc fluid ressuscitation and oxygen supplementation as part of shock management while preparing tools for posterior tampon.
The procedure was successful in the first try within under 1 minute. Hemostatic agent and antibiotic were administrated after.
Procedure as follows;
- Preparation: Foley catheter 14 fr, Syringe 10 ml, Aquabidest 25 ml, Jelly, Water-resistant film Hyperskin TR, Propper PPE (N95 mask, goggle, steril mask, long sleeve gown, shoe cover).
- Quick direct view to posterior pharynx with tounge depressor, he has mallampati class IV
- The foley catheter is tested before insertion
- Plan for insertion foley catheter without direct view by measuring the length of nostril to the tragus from the tip of the ballon. Measurement is marked by a clamp
- After lubricate with jelly, foley catheter was inserted slowly to one side of the nostril till reaching the clamp, open the clamp and followed by inflating 10 mL of air
- Withdraw the catheter to lodge the balloon against choanal arc and add aditional 5 mL of water
- Secure the foley catheter with waterproof film
- Put the tape gauze anteriorly that is filled with epinefrin.
- Repeat the same procedure to the other nostril.
- Clean the patient and cover both nostril a water resistant film on the nostril.
Blood was withdrawn to assess the hemoglobin level and blood transfusions planning. Evaluate and close monitoring the patient’s vital sign in possibility of transient response ressusciation.
After the patient was stable, the patient was screened for covid19 before hospitalized and reffered to ENT specialist. His haemoglobin count was as low as 6.8 g/dL and received blood transfusion without signs of ongoing bleeding during hospitalization. CT Scan paranasal and confirmed by nassal endoscopy revealed that he has sphenoid errosion, sequaelae of post radiation treatment for his nasopharynx carcinoma. He was discharged after 4 days hospitalization.
Discussion
Based on demographic population, older population are common with posterior epistaxis than anterior apistaxis. This patient had a history of nasopharynx carcinoma that has finnished treatments with 6 months free of symtoms. Patient was admitted to ER in unstable condition so taking history from patient was not possible in such situation.
Advance life support is still considered as priority to manage his condition. Working as teamwork, the epistaxis is also needed to be managed at the same time considering that massive unwitnessed bleeding had occured and shock in this patient.
Even no stridor nor gargling found in this patient, risk of airway obstruction come into first. This patient’s airway was risky so simply positioning the patient in left lateral decubitus is wise option in consciouss patient. As covid19 pandemic awareness, screening may take long time and inappropriate to patient with unstable condition, so we opted to non invasive airway management and transferring patient into a closed room as soon as. Every patient admitted to hospital must be suspected covid19 untill proven otherwise.
Amount of fluid ressucitation was made quickly based on amount of blood on his clothes, triage floor and vital sign, he is in hypovolemict shock with class III haemorrhage.
At the same time, preparation is quick. Foley catheter technique is opted as the most effective and quick method that can be done in most emergency room setting. Considering covid19 may be any patient, aresolization procedure must be performed quickly to limit staff being exposed. After quick assessment to pharynx, posterior pharynx was visualize, blinded approach was made by measuring the length of nostril to tragus that is equal to the length from nostril to nasopharynx. If any blockage was found, plan to abbort this procedure. In other posterior epistaxis case of young male adolescent, we found the blockage of left nostril due to juvenile nassal angiofibroma. We plan to place posterior tampon from the free-of-blockage-right nostril but it come out to be failed.
Ballooning Foley catheter with water has risk of aspiration if ruptured. In our opinion, air only inside balloon has risk of leakage as density of air. So combining additional small amount of water will be less risky.
Re-evaluation and monitoring of the patient after this procedure is essential in managing the bleeding. Using a transparent water-resistant film can monitor bleeding from anterior tampon. Transient response of hypovolemict shock, serial haemoglobin and haema faeces test can be a clue for further investigation of leakage, unsuccessful posterior tampon.
Based on our experience, managing posterior bleeding using catheter folley may be beneficial to patient as admitted to Emergency Room, before time consuming covid19 screening or waiting the preparation of more invasive procedure.
Conclusion
Epistaxis is one of the emergency cases that must be handled immediately, especially posterior epistaxis with comorbidities or epistaxis that does not stop with pressure on the nostrils. Even though more invasive procedure such as cauterization, embolization or ligation of the affected blood vessels are effective but Foley catheter technique is beneficial in emergency room setting because it is simple, safe, efficient, and quick. Blind approach of Foley catheter technique might be also useful in patient with mallampati class III-IV. This technique can also be done in health facilities that have limited resources for the best service for the community.
References
- Snow JB, Wackym PA, Ballenger JJ (2009) Ballengerâ??s Otorhinolaryngology: Head and neck surgery. 17th Ed. Shelton, Conn: Peopleâ??s Medical Pub 551-555.
- Reichman EF (2013) Emergency Medicine Procedures. 9th Ed McGraw Hill Medical 1103-1112.
- Claire M (2018) Advanced Trauma Life Support. 10th Ed. American College of Surgeon 29- 49.
- Suresh SD (2016) Clinical Pathways in Emergency Medicine Volume II. Springer 355.
- World Health Organization (2020) Clinical Management of Covid19: interim guidance; 27 World Health Organization 16-37.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences