Biliary Stent with 125I Seeds vs. Simple Biliary Stent for Malignant Obstructive Jaundice: A Systematic Review and Meta-Analysis
Hao Zhang, Shadike Apaer, Li Yu-peng and Tuerhongjiang Tuxun
DOI10.21767/2471-8041.S1-009
Hao Zhang, Shadike Apaer, Li Yu-peng and Tuerhongjiang Tuxun*
Department of Liver and Laparoscopic Surgery, Center of Digestive and Vascular Surgery, The first affiliated Hospital of Xinjiang Medical University, Urumqi, Xinjiang Uyghur Autonomous Region, 830054, P.R.China
- *Corresponding Author:
- Dr. Tuerhongjiang Tuxun
Department of Liver and Laparoscopic Surgery
Center of Digestive and Vascular Surgery
The first affiliated Hospital of Xinjiang Medical University
Urumqi, Xinjiang Uyghur Autonomous Region, 830054, P.R.China
Tel: +86 991 436 2634
E-mail: turgunbay@163.com
Received Date: January 01, 2018; Accepted Date: January 29, 2018; Published Date: February 08, 2018
Citation: Zhang H, Apaer S, Yu-peng L, Tuxun T (2018) Biliary Stent with 125I Seeds vs. Simple Biliary Stent for Malignant Obstructive Jaundice: A Systematic Review and Meta-Analysis. Med Case Rep Vol.4 No. S1:009. DOI: 10.21767/2471-8041.S1-009
Abstract
Aim: To assess the safety, feasibility and efficacy of 125I seeds irradiation stents compared with conventional selfexpandable metal stents (SEMS) to treat malignant obstructive jaundice (MOJ).
Methods: A systematic search of English and Chinese databases, from January 1980 to December 2017, was conducted. All prospective random trials comparing SEMS and the various form of irradiation stent with 125I seeds to treat MOJ were included.
Results: Overall, six studies with 276 patients were eligible in current analysis. Of reported 276 patients, 138 patients were subjected to irradiation stents while 138 patients to SEMS. The irradiation stents are associated with a longer survival (hazard ratio (HR) 0.46, IV, random, 95% confidence interval (CI) 0.34-0.63; p<0.001, I2=0%) and stent patency (HR 0.45, IV, random, 95% CI 0.25-0.80; p=0.007, I2=59%) than conventional SEMS.
There are no differences in total complications rate (relative risk (RR) 0.75, M-H, random, 95% CI 0.41-1.38; p=0.35, I2=0%), hemobilia (RR 0.34, M-H, random, 95% CI 0.07-1.64; p=0.18, I2=0%), pain (RR 0.87, M-H, random, 95% CI 0.29-2.61; p=0.80, I2=0%), and cholangitis (RR 1.33, M-H, random, 95% CI 0.32-5.48; p=0.69, I2=0%).
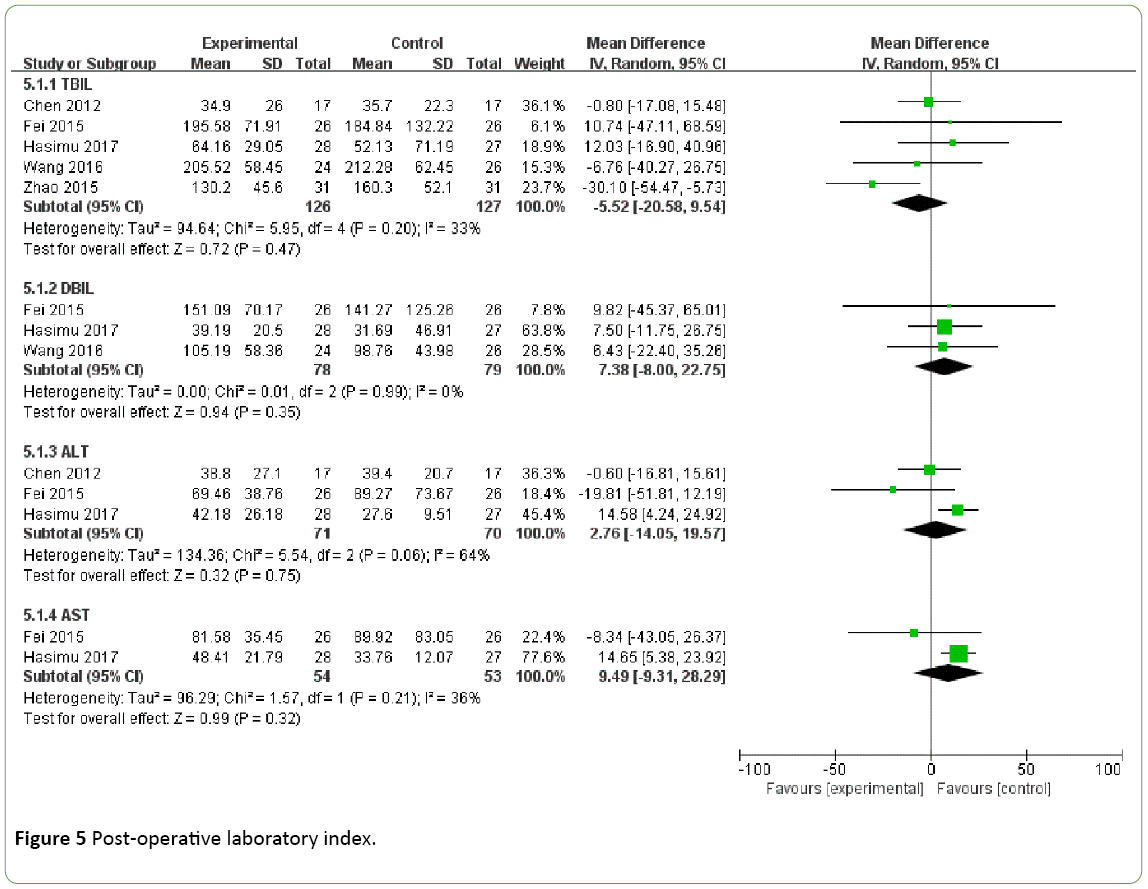
Also, no differences were observed in all indexes, which included total bilirubin (TBIL) (weighted mean difference (WMD) -5.52, IV, random, 95% CI -20.58-9.54; p=0.47, I2=33%), direct bilirubin (DBIL) (WMD 7.38, IV, random, 95% CI -8.00-22.75; p=0.35, I2=0%), alanine aminotransferase (ALT) (WMD 2.76, IV, random, 95% CI -14.05-19.57; p=0.75, I2=64%), aspartate aminotransferase (AST) (WMD 9.49, IV, random, 95% CI -9.31-28.29; p=0.35, I2=0%).
Conclusions: According to limited source data, the current meta-analysis suggests that the irradiation stent is a feasible, safe treatment of MOJ, with longer survival and stent patency. Application of irradiation stent with antitumor effect does not add extra adverse events compared to SEMS stent.
Keywords
125I seeds; Malignant obstructive jaundice; Choledochojejunostomy; Stent patency
Introduction
Malignant obstructive jaundice (MOJ) is a common clinical disease entity primarily caused by pancreato-biliary malignancies including cholangiocarcinoma, pancreatic cancer and ampullary cancer [1,2]. At the time of diagnosis, majority of patients have been barred from radical resection due to extensive tumor growth [3,4].
The median survival of patients with MOJ is reported as 4.8 months [5]. Alleviation of patients' clinical symptoms and correction of complications are priority regarding its unimproved and limited survival and quality of life [2,5].
During recent three decades, surgeons and interventional therapists endeavored to perform palliative drainage by means of choledochojejunostomy, laparoscopic or open, endoscopic or percutaneous techniques [6]. Biliary stents showed better clinical efficacy and quality of life compared to surgical bypass [7].
Various types of biliary stents with special structure and materials were designed for endoscopy or percutaneous drainage. Previous studies compared different types of stents and claimed that self-expandable metallic stents (SEMS) is superior to plastic stents in terms of patency, morbidity, and re-interventions [8].
In addition, no obvious advantages were identified in coverd self-expandable metal stent (CSEMS) or uncovered selfexpandable metal stents (UCSEMS) [9]. However, the tumor growth is not control and resulting in a high risk of occlusion, epithelial hyperplasia, sludge formation, and clot accumulation [10,11].
Efforts have been made to introduce novel biliary stent with anti-tumor effect. Currently, paclitaxel-eluting stents [12] and irradiation stent loaded with 125I seeds [13-18] are among the mostly used stents in South Korea and China respectively.
Permanent radioactive seed implantation in malignancy was firstly suggested by several authors in the early 1900s [19]. Thereafter, this technique has been practiced in different types of cancers. Recent years, large number of animal experiments, single arms, and control studies regarding the application of 125I stent in patients with MOJ have been published one after another [20,21].
However, systematic review and meta-analysis comparing 125I stents with conventional stents are still lacking. Therefore, we performed a systematic review and meta-analysis by synthesizing present evidence to assess efficacy and safety of the irradiation stents compared with conventional stents.
Materials and Methods
Eligibility criteria
We include all randomized controlled trials (RCTs) and control clinical trials (CCTs) in human. There were no language restrictions. Conference abstract and thesis were ruled out. We included single and multi-centre studies, which compared the 125I irradiation stent (various form of combined implantation of 125I seeds and CSEMS or UCSEMS) with CSEMS or UCSEMS.
Both endoscopic and percutaneous approaches for stent implantation were included. The study population is without age and gender restrictions. MOJ was caused by any unresectable tumor (distal or proximal).
Search strategy
English databases (MEDLINE, EMBASE, Cochrane library), Chinese databases (CBM, CNKI, VIP), and Clinicaltrials.gov (from January 1980 to December 2017) were searched. References of systematic review and included studies were also searched. The search strategy was based on MeSH terms combined with text words. The detail can be view in Table S1.
Choice of outcome
The primary outcomes included patient survival and cumulative stent patency. Cumulative stent patency is time from stent placement to recurrent biliary obstruction or patient died.
Secondary outcomes included (i) complications: total complications, pancreatitis, cholecystitis, cholangitis, hemobila, stent and seed migration, tumor ingrowth and outgrowth; (ii) post-operative laboratory values: alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TBIL), direct bilirubin (DBIL).
Data collection
Two independent reviewers (S.A and L.Y.P) selected the studies by reviewed the title and abstract of every single study. Disagreements were resolved by a third reviewer (T.T). For selected studies, data of trial information (author, year, intervention, center and type of stent), population characteristics (sex, age, classification of the tumor and location of obstruction), and reported outcomes were extracted independently by two investigators (H.Z and S.A).
Quality of studies was assessed by the Cochrane Collaboration’s tool for assessing risk of bias. The assessment was carried out by three independent investigators (H.Z, T.T and S.A).
Statistical analysis
Hazard ratios (HRs) with 95% confidence intervals (CIs) were chosen to measure the effects of stent patency and patient survival, relative ratios (RRs) with 95% CIs to measure the complications, and weighted mean differences (WMDs) to measure laboratory values. HRs can be extracted from the paper directly or obtained by method of Tierney et al. [22] from Kaplan-Meier curves or other data.
All comparisons were performed by random-effects models in RevMan software version 5.3. Inconsistency index (I2) statistics were calculated to measure the heterogeneity. Although size of heterogeneity have no uniform definition, I2 values more than 50% indicated significant heterogeneity in current article. Sensitivity analyses were performed, if high heterogeneity was found or the significance of effect size was affect by a single study. For primary outcome, publication bias was assessed using Egger test and Begg test by Stata 14.0.
Results
Search results
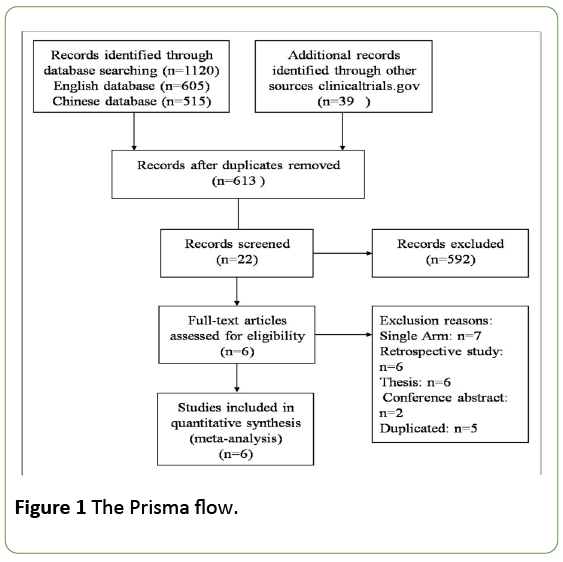
A total number of 1120 publications were examined in initial systematic search. 1098 duplicates and irrelevant comparisons publications were excluded. Of remaining 22 trials, seven were single arm studies, six were retrospective studies, eight were theses and conference abstracts, four were duplicate publications.
Finally, six studies (Tables 1 and 2) were included in the meta-analysis with three English articles [13,15,18] and three Chinese articles [14,16,17]. English abstract of Chinese article can be searched in PubMed or EMBASE, one was registered in clinicaltrial.com. The prisma flow is shown in Figure 1.
| Study | Stent | NO. of patients | Male/female | Age (y) | patient survival (days) | stent patency (days) | No. of complications |
|---|---|---|---|---|---|---|---|
| Hasimu[15] | Irradiation stents | 28 | Nov-17 | mean ± SD 70.93 ± 8.58 | mean ± SD 222.6 ± 21.0 | mean ± SD 191 ± 19.8 | 4 |
| UCSEMSs | 27 | 14/13 | mean ± SD 70.26 ± 9.71 | mean ± SD 139.1 ± 14.5 | mean ± SD 88.3 ± 16.3 | 5 | |
| Zhu [18] | Irradiation stent | 12 | 07-May | Median62.50 (21.00) | median 222 | median 222 | 1 |
| UCSEMSs | 11 | 09-Feb | Median71.00 (22.00) | median 75 | median 75 | 5 | |
| Chen [13] | Irradiation stents | 17 | 12-May | mean ± SD 61.2 ± 14.5 | - | median 300 | 4 |
| UCSEMSs | 17 | 10-Jul | mean ± SD 63.9 ± 9.3 | median 240 | 4 | ||
| Wang [16] | Irradiation stents | 24 | 29/21 | Median (range) | median 306 | median 295 | - |
| UCSEMSs | 26 | 57.3 (41-80) | median 162 | median 167 | |||
| Fei[14] | Irradiation stents | 26 | Oct-16 | mean ± SD 70 ± 12 | mean ± SD 386 ± 47 | - | 6 |
| UCSEMSs | 26 | Nov-15 | mean ± SD 73 ± 11 | mean ± SD 267 ± 32.4 | 7 | ||
| Zhao [17] | Irradiation stents | 31 | 28/34 | mean ± SD (range) | median 330 | - | 0 |
| UCSEMSs | 31 | 68 ± 3.5 (56-85) | median 300 | 0 | |||
| UCSEMSs: Uncovered self-expandable metal stents;Irradiation stents. Combination of 125I seeds and uncovered self-expandable metal stents. |
|||||||
Table 1: Characteristics of the studies included in meta-analysis.
| Study | Stent | Diagnosis of obstructive jaundice | |||||
|---|---|---|---|---|---|---|---|
| Cholangiocarcinoma | Hepatocellular carcinoma | Pancreatic cancer | Metastases | Gallbladder cancer | Ampullary carcinoma | ||
| Hasimu[15] | Irradiation stents | 24 | - | - | - | 4 | - |
| UCSEMSs | 24 | 3 | |||||
| Zhu [18] | Irradiation stent | - | - | - | 4 | - | - |
| UCSEMSs | 6 | ||||||
| Chen [13] | Irradiation stents | 7 | 2 | 3 | 5 | - | - |
| UCSEMSs | 7 | 4 | 3 | 4 | |||
| Wang [16] | Irradiation stents | 18 | - | 14 | 12 | - | 6 |
| UCSEMSs | |||||||
| Fei[14] | Irradiation stents | 26 | - | - | - | - | - |
| UCSEMSs | 26 | ||||||
| Zhao [17] | Irradiation stents | 39 | - | 17 | 3 | 3 | |
| UCSEMSs | |||||||
| Total | - | 171 | 6 | 37 | 31 | 10 | 9 |
| UCSEMSs: Uncovered Self-Expandable Metal Stents;Irradiation stents. Combination of 125I seeds and uncovered self-expandable metal stents. |
|||||||
Table 2: Tumor type of studies included in meta-analysis.
A total of 276 patients were enrolled, 138 to irradiation stents and 138 to UCSEMS. Cholangiocarcinoma and pancreatic cancer were the main reasons for MOJ. In all studies, stent and 125I seeds implantations was performed by percutaneous insertion and UCSEMS was identified as control group. All studies were carried out by single center in China.
Risk of bias
Six trials included three RCTs and three CCTs. Every study was conducted a qualitative risk assessment by Cochrane Collaboration’s tool for assessing risk of bias (Figures S1 and S2). Performance bias was severe, due to it is difficult to mask radiologists on whether to implant radiation sources. High heterogeneity was observed in comparisons of stent patency and ALT.
Sensitivity analyses were carried out, no differences were observed in any comparisons. Heterogeneity of stent patency originates from CCTs.
After excluding the trial, heterogeneity decreased distinctly, but the outcome was the same indicated that irradiation stents exhibited a better stent patency.
The Egger and Begg tests were carried out to assess potential publication bias for primary outcomes, and no potential publication biases were observed (Figure S3).
Primary outcomes
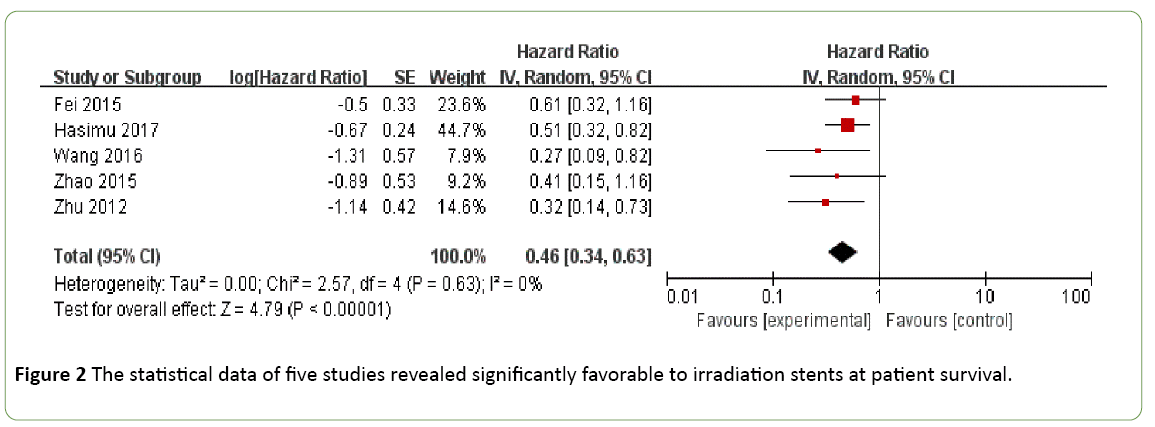
Patient survival: Patient survival data were not provided in one study. The statistical data of five studies revealed significantly favorable to irradiation stents at patient survival (HR 0.46, IV, random, 95% CI 0.34-0.63; p<0.001, I2=0%) (Figure 2).
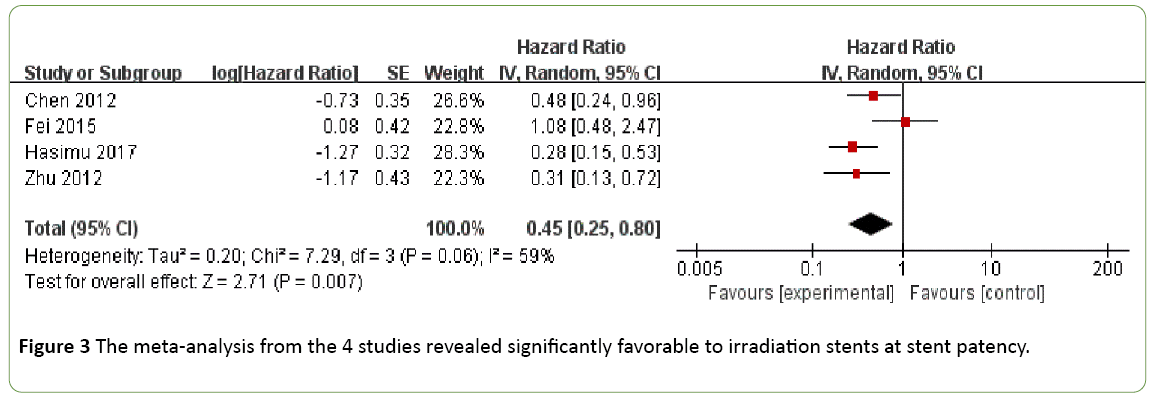
Stent patency: The meta-analysis from the 4 studies revealed significantly favorable to irradiation stents at stent patency (HR 0.45, IV, random, 95% CI 0.25-0.80; p=0.007, I2=59%) (Figure 3).
Secondary outcomes
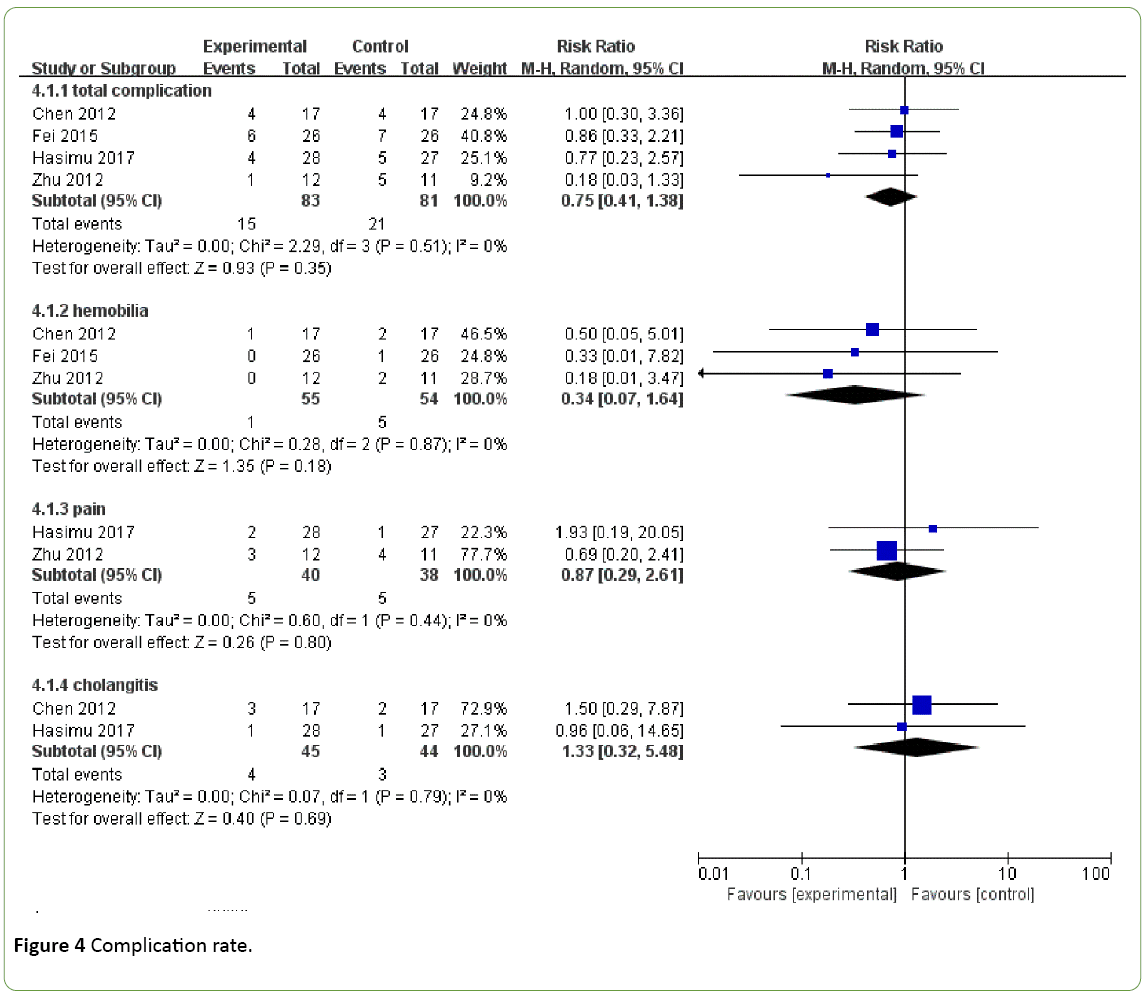
Complication rate: There are no differences in total complications rate (RR-0.75, M-H, random, 95% CI 0.41-1.38; p=0.35, I2=0%), hemobilia (RR 0.34, M-H, random, 95% CI 0.07-1.64; p=0.18, I2=0%), pain (RR 0.87, M-H, random, 95% CI 0.29-2.61; p=0.80, I2=0%), and cholangitis (RR 1.33, M-H, random, 95% CI 0.32-5.48; p=0.69, I2=0%) (Figure 4).
Post-operative laboratory index: No differences were observed in all indexes, which included to TBIL (MD -5.52, IV, random, 95% CI -20.58-9.54; p=0.47, I2=33%), DBIL (MD 7.38, IV, random, 95% CI -8.00-22.75; p=0.35, I2=0%), ALT (MD 2.76, IV, random, 95% CI -14.05-19.57; p=0.75, I2=64%), AST (MD 9.49, IV, random, 95% CI -9.31-28.29; p=0.35, I2=0%) (Figure 5).
Discussion
Biliary stents have been applied in treatment of patients with MOJ more than 30 years, since it is considered as the most effective and mini-invasive approach to alleviate patients' clinical symptoms. Currently, local chemoradiotherapy combined with stent drainage has been becoming the classic therapeutic strategy to prolong patient survival and stent patency [6]. However, the hypovascular feature of pancreatic cancer, cholangiocarcinoma, and most of metastases limit curative effect of chemotherapy [23,24].
Additionally, the existence of radiosensitive organs around the site of obstruction and poor general conditions of patients may lead to adverse events in application of external beam radiation therapy. Intraluminal brachytherapy (ILBT) avoid these problems. Before Iodine-125, Iridium-192 wire as a high dose of irradiation showed promising effects in MOJ treatment [24,25]. However, with the development of radioisotope seeds, Iodine-125 seed as a low dose seed has been replacing Iridium-192 in many indications [26], due to the advantage of safety and prolonged exposure which avoid the second operation to take out the seeds and/or repeated interventions in some conditions.
To the best of our knowledge, this is the first meta-analysis to assess the safety and efficacy of 125I irradiation stent compared with conventional metal stents. The meta-analyses of primary outcome showed that irradiation stent provided significantly longer patient survival and stent patency. Same results can observe from median or mean of patient survival and stent patency which were not involved the meta-analysis, due to the limited expression of overall survival status.
Although there were various inserting ways and type of irradiation stents in different studies, all implanting seeds increased complexity of the operation and narrowed caliber of stent indirectly. However, our analyses showed no significant difference between two group in complication rates and laboratory values after operation which were analyzed to measure the short-term drainage efficiency and recovery of liver function. Three studies reported Hemobilia, which occurred mainly during hospital stay and were healed before discharge, due to injury of the biliary intima resulted from the interventional operation rather than effect of irradiation. Fecal occult blood test in Chen et al. [13] indicated negative results in both groups during the first month of follow-up. The quantitative records of pain were defined as short-term and severe conditions, which were mainly caused by biliary irritation, operative injury, and infection. Two investigators have reported the incidence of cholangitis, although a pervious study [27] suggested that ILBT correlates with increased risk for cholangitis, especially after percutaneous transhepatic biliary drainage (PTBD) or stent insertion, our analyses showed no significant difference between two group, even carrying drainage catheter with the seeds strand for two months in the experimental group of Chen et al.
Three studies reported antitumor effect of irradiation stents. CA19-9 were followed up by two investigators [16,17] at different time point, the results showed after procedure the marker declined and remained at a lower level in experimental group, while the marker in control group was gradually increased. Fei et al. [14] showed the changed in maximum and minimum tumor size before and six months after operation by CT scan. The results indicated that the seed strand shrank the tumor obviously.
In terms of radiological safety, a minimal average does (0.018 ± 0.009 mSV) were detected in Liu et al. [21] by a personal dosimeter, which was worn on the waist of operator during all procedures. Additionally, the effective radiation radius of 125I seeds is less than 20mm that results in easy radioprotection for peri-tumor tissue and medical workers [28]. The number and distribution of implanted seeds were determined by the length of the obstructive segment. In seeds strand, Fei et al. [14] identified a 6-10mm source-to-source distance to adjust radiation dose. However, other studies arranged no spacing in their seed strand. Tight arrangement provided higher dose (80-90Gy), which has been proven to be safe in the previous experiment [29]. And all studied mentioned no migration or dislodging of 125I seed was observed during the follow-up period, also no radiationinduced enteritis or liver injury were reported.
In the current meta-analysis, as in previous clinical and animal studies, irradiation stent displayed better efficiency and has equal safety and stability compared with conventional stent. Although various forms of the irradiation stent with 125I seeds have been used in treatment of MOJ and a number of clinic retrospective studies can be indexed, there are no guidelines for specific applications, uniformly designed stents, and experience of using radioactive source for the most of clinical department. Considering radioactivity, operators might prefer to other non-radioactive methods. Clearly, the wide application of irradiation stent in MOJ still has a long way to go, and need further promotion and more special stent and auxiliary equipment. Moreover, a recent high quality RCT [12] demonstrated another anti-tumor paclitaxel-eluting stent had no obvious advantage over the conventional covered stent. Nevertheless, maybe we can compose the two stent together to obtain better effectiveness, based on the radiosensitization of paclitaxel in many malignant tumors [30].
Limitations
The most important limitation of the current meta-analysis is only six studies were included into the analyses according to our inclusion criteria, and all studies are from Chinese single center. Owing to the limited number of studies, the power of publication bias tests was also reduced significantly. All studies were performed by percutaneous insertion and only used UCSEMS both in two groups. Sources of heterogeneity include patient populations (different department, other treatments during follow-up or not, proximal or distal), use of antibiotics, definitions of complications, choice of reporting secondary outcomes, and measures of data spread. The Cochrane bias risk scare showed incomplete blind method, which caused by the nature of invasive procedures. Moreover, since most of the patients died during the follow-up period, there is not a appropriate index to measure the stent patency only, which also caused the differently reported form and make it difficult to integrate. Finally, no studies involved cost-effective analysis or mentioned the cost of seed strand and seeds-loaded-stent, which may limit the application of the results and choice of finished products or self-made seed strand.
Conclusion
Our meta-analysis suggested that various kinds of 125I seeds irradiation stent are a potent tool for MOJ. The patients treated with the irradiation stent do not experience extra adverse events (pain, hemobilia, and cholangitis) and have a longer survival, stent patency, compared with UCSEMS. And the unique anti-tumor effect of irradiation stent was noted by CA19-9 and CT scan during the follow up period.
References
- Khan SA, Thomas HC, Davidson BR (2005) Taylor-Robinson SD. Cholangiocarcinoma. Lancet 366: 1303-1314.
- Kozarek R (2013) Role of preoperative palliation of jaundice in pancreatic cancer. J HepatobiliaryPancreatSci 20: 567-572.
- Baron TH (2006) Palliation of malignant obstructive jaundice. GastroenterolClin North Am 35: 101-112.
- Fazal S, Saif MW (2007) Supportive and palliative care of pancreatic cancer. JOP 8: 240-253.
- Pinter M, Hucke F, Zielonke N, Waldhor T, Trauner M, et al. (2014) Incidence and mortality trends for biliary tract cancers in Austria. Liver Int 34: 1102-1108.
- Lorenz JM (2016) Management of malignant biliary obstruction. SemIntervenradiol 33: 259-267.
- Moss AC, Morris E, Leyden J, MacMathuna P (2007) Malignant distal biliary obstruction: a systematic review and meta-analysis of endoscopic and surgical bypass results. Cancer Treat rev 33: 213-221.
- Almadi MA, Barkun A, Martel M (2017) Plastic vs. self-expandable metal stents for palliation in malignant biliary obstruction: A series of meta-analyses. Am J Gastroenterol 112: 260-273.
- Li J, Li T, Sun P, Yu Q, Wang K, et al. (2016) Covered versus uncovered self-expandable metal stents for managing malignant distal biliary obstruction: A meta-analysis. PLoSOne. 11: e0149066.
- Rogart JN, Boghos A, Rossi F, Al-Hashem H, Siddiqui UD, et al. (2008) Analysis of endoscopic management of occluded metal biliary stents at a single tertiary care center. GastrointestEndosc 68: 676-682.
- Shah T, Desai S, Haque M, Dakik H, Fisher D (2012) Management of occluded metal stents in malignant biliary obstruction: similar outcomes with second metal stents compared to plastic stents. Dig Dis Sci 57: 2765-2773.
- Jang SI, Lee SJ, Jeong S, Lee DH, Kim MH, et al. (2017) Efficacy of a multiplex paclitaxel emission stent using a pluronic (r) mixture membrane versus a covered metal stent in malignant biliary obstruction: A prospective randomized comparative study. Gut&Liver 11: 567-573.
- Chen Y, Wang XL, Yan ZP, Wang JH, Cheng JM, et al. (2012) The use of 125I seed strands for intraluminal brachytherapy of malignant obstructive jaundice. Cancer bio radiopharma 27: 317-323.
- Fei SX, Liu HC, Sun Z, Li ZK, Zhou L, et al. (2015) Evaluation of the curative effect of biliary stents combined with 125I particles for intracavitary treatment of malignant jaundice in cholangiocarcinoma. Chin J ClinOncol 42: 564-569.
- Hasimu A, Gu JP, Ji WZ, Zhang HX, Zhu DW, et al. (2017) Comparative study of percutaneous transhepatic biliary stent placement with or without Iodine-125 seeds for treating patients with malignant biliary obstruction. J VascIntervRadiol 28: 583-593.
- Wang T, Liu S, Zheng YB, Song XP, Jiang WJ, et al. (2016) Application of (125) I seeds combined with biliary stent implantation in the treatment of malignant obstructive jaundice. Zhonghuazhongliuzazhi 38: 228-231.
- Zhao SM, Zhao H, Gu WW, Yang XH, Jia PF (2015) Treatment of malignant obstructive jaundice by biliary stent and biliary stent combined with 125I seed implantation. Journal of Shanghai Jiaotong University (Medical Science) 35: 1661-1665.
- Zhu HD, Guo JH, Zhu GY, He SC, Fang W, et al. (2012) A novel biliary stent loaded with (125)I seeds in patients with malignant biliary obstruction: preliminary results versus a conventional biliary stent. J Hepatol 56:1104-1111.
- Packer S, Rotman M (1980) Radiotherapy of choroidal melanoma with iodine 125. Ophthalmology 20: 135-142.
- Liu Y, Liu JL, Cai ZZ, Lu Z, Gong YF, et al. (2009) A novel approach for treatment of unresectableextrahepatic bile duct carcinoma: design of radioactive stents and an experimental trial in healthy pigs. GastrointestEndosc 69: 517-524.
- Liu Y, Lu Z, Zou DW, Jin ZD, Liu F, et al. (2009) Intraluminal implantation of radioactive stents for treatment of primary carcinomas of the peripancreatic-head region: a pilot study. GastrointestEndosc 69: 1067-1073.
- Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8: 16.
- Kawahara N, Ono M, Taguchi K, Okamoto M, Shimada M, et al. (1998) Enhanced expression of thrombospondin-1 and hypovascularity in human cholangiocarcinoma. Hepatol 28: 1512-1517.
- Chen Y, Wang XL, Yan ZP, Cheng JM, Wang JH, et al. (2004) HDR-192Ir intraluminal brachytherapy in treatment of malignant obstructive jaundice. World journal Gastroenterol 10: 3506-3510.
- Levitt MD, Laurence BH, Cameron F, Klemp PF (1988) Transpapillary iridium-192 wire in the treatment of malignant bile duct obstruction. Gut 29: 149-1452.
- Clarke DH, Edmundson GK, Martinez A, Matter RC, Vicini F, et al. (1989) The clinical advantages of I-125 seeds as a substitute for Ir-192 seeds in temporary plastic tube implants. Int J RadiatOncolBiolPhys 17: 859-863.
- Li Sol Y, Kim CW, Jeon UB, Lee NK, Kim S, et al. (2010) Early infectious complications of percutaneous metallic stent insertion for malignant biliary obstruction. AJR 194: 261-265.
- Blasko JC, Ragde H, Luse RW, Sylvester JE, Cavanagh W, et al. (1996) Should brachytherapy be considered a therapeutic option in localized prostate cancer? UrolClin North Am 23: 633-650.
- Liu Y, Liu JL, Cai ZZ, Lu Z, Dong YH, et al. (2007) A novel approach for treatment of unresectable pancreatic cancer: Design of radioactive stents and trial studies on normal pigs. Clin Cancer Res 13: 3326-3332.
- Kurdoglu B, Cheong N, Guan J, Corn BW, Curran WJ Jr., et al. (1999) Apoptosis as a predictor of paclitaxel-induced radiosensitization in human tumor cell lines. Clin Cancer Res 5: 2580-2587.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences