Barnes Syndrome: A Case of De Novo with Progression to Severe Respiratory Failure
Raúl Montero Yéboles1*, Jesús López Herce1, Clara Molina1, María Herrera1, Amaya Bustinza1, Amelia Sánchez1, Adoración Blanco2 and María Antonia Casillas3
DOI10.21767/2471-8041.100110
Raúl Montero Yéboles1*, Jesús López Herce1, Clara Molina1, María Herrera1, Amaya Bustinza1, Amelia Sánchez1, Adoración Blanco2 and María Antonia Casillas3
1Paediatric Intensive Care Section, Hospital General Universitario Gregorio Marañón, Madrid, Spai
2Neonatology Service, Hospital General Universitario Gregorio Marañón, Madrid, Spain
3Paediatric Surgery Service, Hospital General Universitario Gregorio Marañón, Madrid, Spain
- *Corresponding Author:
- Raúl Montero Yéboles
Avenida de Moratalaz 187 1C 28030 Madrid, Spain
Tel: +34 677 69 34 01
E-mail : rmyeboles@hotmail.com
Received date: May 21, 2018; Accepted date: June 22, 2018; Published date: June 24, 2018
Citation: Yeboles RM, Herce JL, Molina C, Herrera M, Bustinza A, et al. (2018) Barnes Syndrome: A Case of De Novo with Progression to Severe Respiratory Failure. Vol.4 No.3:74. doi:10.21767/2471-8041.100110
Abstract
Barnes syndrome is a rare entity observed among thoracic dysplasia/hypoplasia with or without polydactyly. It is a very low frequency disease of autosomal dominant transmission with variable penetrance. It is characterized by a laryngeal stenosis, costal narrowing and reduced pelvic dimensions. We present the case of a 5-month-old patient who is admitted to our Intensive Care Unit for progressive respiratory failure. She was diagnosed in utero with probable asphyxiating thoracic using Magnetic Resonance Imaging. When the patient was two months old, a whole-body bone scan was made and ruled out the disease, diagnosing the patient with spondyloepiphyseal dysplasia congenita. On admission to our unit, she presented progressive worsening, despite non-invasive mechanical ventilation, requiring intubation. This intubation was not possible due to significant subglottic stenosis.
A tracheostomy was performed, and the patient was connected to mechanical ventilation. Fibrobronchoscopy was performed and showed significant laryngeal stenosis and a Chest CT showed severe obliteration of the proximal tracheal lumen. The bone scan showed chest narrowing and hypoplasia of the pelvis which, together with laryngeal stenosis, allowed the diagnosis of Barnes Syndrome. We proposed thoracic surgery in order to increase the size of the rib cage, thereby improving the lung function. The family refused consent and the patient died a month later after removal of ventilation (at the request of parents).
Keywords
Barnes syndrome; Jeune syndrome; Respiratory failure; Laryngeal stenosis; Costal narrowing; Pelvic dysplasia; Thoracic surgery
Introduction
Barnes syndrome is a rare entity observed among thoracic dysplasia/hypoplasia with or without polydactyly. It was described by Barnes in 1969, who included it within the Jeune syndrome [1] but identified as a distinct syndrome called thoracolaryngopelvic dysplasia (TLPD) or Barnes Syndrome in 1986 [1]. It is a very low frequency disease of autosomal dominant transmission with variable penetrance. It is characterized by a laryngeal stenosis, costal narrowing and reduced pelvic dimensions. The clinical expression of the syndrome is variable from minimal impact to fatal outcome [1-4]. Mortality is determined by the degree of degree of impairment of lung function. We present a patient diagnosed with Barnes syndrome with no family history, that showed a progressive evolution that led to severe respiratory failure.
Clinical Case Presentation
A 5-month-old patient diagnosed with asphyxiating thoracic dysplasia and severe bronchopulmonary dysplasia requiring home oxygen therapy, who is admitted to our Intensive Care Unit for progressive respiratory failure. She was diagnosed in utero with polyhydramnios and probable asphyxiating thoracic dysplasia subsequently confirmed by Nuclear Magnetic Resonance. The patient was born at 29 weeks with birth weight of 1330 g. In the neonatal period she presented hyaline membrane disease and needed mechanical ventilation for 4 days, two doses of surfactant and then 3 days of non-invasive ventilation. Transfontanelar and abdominal ultrasounds were performed, pH monitoring, laryngo fiberscope, metabolic tests and karyotype that were normal. Chest radiography and CT were consistent with Bronchopulmonary Dysplasia and heart ultrasound showed a small-sized muscular ventricular septal defect without pulmonary hypertension. When the patient was 2 months old, the chest diameter was 29 cm and the whole-body bone scan ruled out asphyxiating thoracic dysplasia diagnosing the patient with spondyloepiphyseal dysplasia congenital.
When the patient was two and a half months old she was discharged with oxygen therapy to her referral hospital and subsequently to her home.
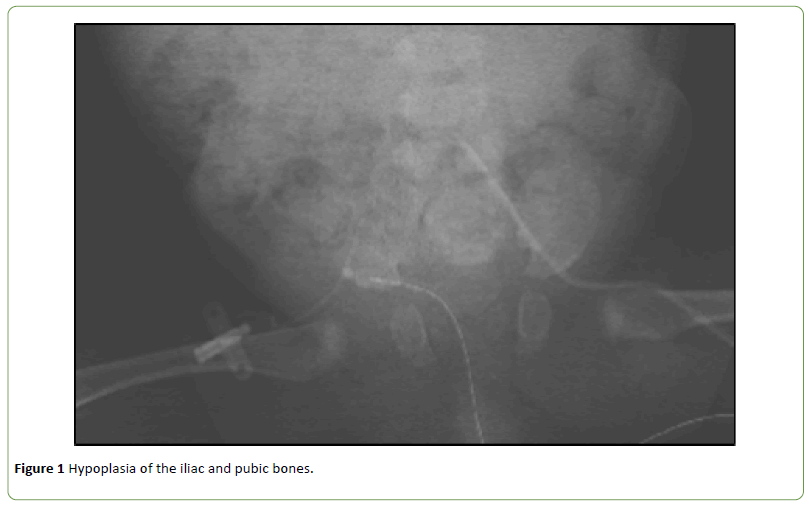
On admission to our ICU the patient weighed 5 kg (10 percentile corrected for gestational age) and was in a regular general state: heart rate 135 beats per minute; breathing frequency: 45 rpm; blood pressure 99/54 mmHg and an oxygen saturation of 93% with oxygen in nasal cannula at 4 L/ min. She had abdominal breathing with severe subcostal and intercostal retractions and bilateral pulmonary hypoventilation with elongated expiration. Cardiac auscultation evidenced a grade II/IV murmur. The abdomen was globose compared with a small chest. We began noninvasive ventilation and it was progressively increasing to a peak inspiratory pressure of 21 cm H2O and maximum expiratory pressure of 12 cm H2O. On the 5th day of admission, she presented significant worsening with bilateral pulmonary atelectasis, cyanosis and severe hypercapnia with PCO2: 124 mmHg, therefore we decided to perform a fiberoptic intubation, where we observed a significant subglottic stenosis, and it did not allow tracheal intubation not even with a 2 mm diameter tube. During the intubation attempt, the patient suffered a cardiac arrest (CA) from which it recovered with cardiac massage and adrenaline, performing an emergency tracheotomy, implanting a paediatric cannula size 3.5. Within a few hours of the cardiac arrest, neurological examination and EEG were normal. Fibrobronchoscopy was performed and it showed a significant laryngeal stenosis and a chest CT showed severe obliteration of the proximal tracheal lumen of about 8 mm, bilateral bronchiectasis in the lower lobes and bell-shaped rib cage with short and wide ribs. Whole-body bone scan showed chest narrowing and changes of the pelvis (hypoplasia of the iliac and pubic bones) (Figure 1) which, together with laryngeal stenosis, allowed the diagnosis of Barnes Syndrome.
A study was conducted not finding clinical signs in any of the members of the family. Since the disease has an autosomal dominant transmission, we concluded that the patient was a carrier of a de novo mutation. The patient required continuous mechanical ventilation support with a restrictive lung disorder without a decrease of ventilatory support. Although thoracic diameters increased from 29 cm (when she was two months old) to 41 cm (when she was 7-months-old) we proposed thoracic surgery using expander bars as initial surgery, to subsequently perform costal distraction surgery in both hemithorax in order to increase the size of the rib cage, thereby improving the lung function. The family refused consent and the patient was transferred to another unit closer to her home, where she died a month later after removal of ventilation (at the request of parents).
Discussion
Generally, Barnes syndrome is very rare; we found fewer than 10 cases reported in the literature and with a highly variable evolution [1-4]. Typically, children with this syndrome have a small, stiff, bell-shaped chest with costal horizontalization but they do not have hypoplastic lungs, unlike in the Jeune syndrome in which pulmonary hypoplasia is the root cause of death [5-7]. They have an abnormal configuration of laryngeal cartilages with an increase of the chondrocostal junction, small pelvic cavity, hands and feet of normal proportions and normal height. They neither have kidney malformations, which is the second leading cause of death in the Jeune syndrome [4-8] nor neurological deficit (Table 1). The differential diagnosis must be established with all these skeletal dysplasias presenting small thorax and short ribs (Table 2).
| Jeune Syndrome | Barnes syndrome |
| Short fingers, polydactyly and nail hypoplasia | Normal hands and feet |
| Dwarfism or short height | Normal height |
| Renal disorders (nephronophthisis, interstitial nephritis) | Healthy kidneys |
| Pulmonary hypoplasia | Normal pulmonary parenchyma (Respiratory insufficiency due to a thoracic narrowing) |
| Hepatic and pancreatic involvement (prolonged neonatal jaundice, cysts, cirrhosis, pancreatic insufficiency) | Normal liver and pancreas |
| Normal upper respiratory tract | Laryngeal stenosis |
| Sometimes, neurological disorders (agenesis of the corpus callosum Dandy-Walker syndrome) Retinopathy Normal intelligence in most cases |
No neurological disorders |
| Occasionally, poor intestinal absorption | Normal digestive system |
Table 1: Differences between Barnes syndrome and Jeune syndrome.
| Variables | Jeune Syndrome | Barnes Syndrome | Ellis-Van Creveld Syndrome | Saldino- Noonan Syndrome | Majewski Syndrome | Beemer-Langer Syndrome |
|---|---|---|---|---|---|---|
| Prevalence | Frequent | Very rare | Rare | Frequent | Very rare | Rare |
| Thoracic Restriction | ++ | ++ | + | +++ | +++ | +++ |
| Polydactyly | + | - | ++ | ++ | ++ | ++ |
| Cardiopathy | + | + | + | +++ | + | ++ |
| Characteristics | Renal disease | Laryngeal stenosis | Ectodermic dysplasia | Genitourinary and gastrointestinal disorders | Cleft lip and palate | Cleft lip and palate, genitourinary and gastrointestinal disorders |
Table 2: Differential diagnosis of the skeletal dysplasias with thoracic hypoplasia.
Conclusion
The prognosis of this disease is difficult to determine because there are few cases described the varied clinical expression that may occur. When respiratory failure is severe, as in our patient's case, and no chest expansion surgery is performed long-term survival is nil. There is only one published case who reached adulthood [1]. Therefore, the early diagnosis and prenatal genetic counseling are paramount. Treatment will vary depending on the degree of respiratory failure [2]. Costal expansion surgery is seen as a possibility to allow the growth and maturation of nonhypoplastic lungs [3,4].
However, severe laryngeal stenosis will likely lead to the need for permanent tracheostomy and these patients will require, if they survive, multiple surgeries at risk of long-term development of pulmonary hypertension. In our case, the family after being informed of the diagnosis and little chance of long term survival without continuous mechanical ventilation, decided not to subject her to any surgical treatment and to remove ventilator support.
Acknowledgments
We thank our dear singular patient and especially their parents, whose commitment and dedication were constant, and all workers who perform outstanding work in our Intensive Care Unit.
References
- Burn J, Hall C, Marsden D (1986) Autosomal dominant thoracolaryngopelvic dysplasia: Barnes syndrome. J Med Genet 23: 345-349.
- Miller TL, Cox T, Blackson T (2006) Pulmonary function assessment in an infant with Barnes syndrome: proactive evaluation for surgical intervention. Pediatrics 118: 1264-1267.
- Gilchrist BF, Kearns D (1995) Laryngotracheal stenosis in thoracolaryngopelvic dysplasia: Barnes syndrome. Otolaryngol Head Neck Surg 113: 807-809.
- Gilchrist BF, Shroff V, DeLuca FG (1996) Management of thoracolaryngeal dysplasia. Eur J Pediatr Surg 6: 231.
- Guerrero FJ, Domínguez GMV (2001) Displasia torácica asfixiante. Pediatrika 2: 1-3.
- Sleurs E, Clavelli W (2001) Asphyxiating thoracic dystrophy. Fetus Net.
- Ozcay F, Derbent M, Demirhan B (2001) A family with Jeune syndrome. Pediatr Nephrol 16: 623-626.
- Ring E, Zobel G, Ratschek M (1990) Retrospective diagnosis of Jeune's syndrome in two patients with chronic renal failure. Child Nephrol Urol 10: 88-91.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences