Association of Vitamin D Repletion with Normalization of Elevated Serum 17-OH-Progesterone
Gabriel Fenteany, Taiga Inoue, Gul Bahtiyar and Alan S Sacerdote
DOI10.21767/2471-8041.100057
Gabriel Fenteany, Taiga Inoue, Gul Bahtiyar and Alan S Sacerdote*
Department of Medicine, New York City Health Hospitals/Woodhull, 760 Broadway, Brooklyn, New York 11206, USA
- *Corresponding Author:
- Alan S. Sacerdote
Department of Medicine, New York City Health Hospitals/Woodhull
760 Broadway, Brooklyn, New York 11206
USA
Tel: 718-963-8382
Fax: 718-963-8753
E-mail: Alan.Sacerdote@woodhullhc.nychhc.org
Received date: May 04, 2017; Accepted date: June 24, 2017; Published date: June 26, 2017
Citation: Fenteany G, Inoue T, Bahtiyar G, Sacerdote AS (2017) Association of Vitamin D Repletion with Normalization of Elevated Serum 17- OH-Progesterone. Med Cas Rep 3:3.
Abstract
Insulin resistance is associated with a number of conditions, such as non-classic 21-hydroxylase deficiency and allied disorders. Serum vitamin D is often deficient/ insufficient in insulin resistant individuals. Disorders associated with insulin resistance are often mitigated in association with vitamin D repletion. Here we report a patient with type 2 diabetes mellitus, lower extremity infection, vitamin D insufficiency, and elevated unstimulated serum 17-OH-progesterone (17-OHP), which normalized during vitamin D repletion. Serum 25-OHvitamin D (25-OHD) rose by 32% while serum 17-OHP fell by 87% over the course of four weeks receiving 50,000 IU ergocalciferol orally weekly. Vitamin D repletion in this setting restored normal serum 25-OHD levels and was associated with normalization of elevated serum 17-OHP. Serum 25-OHD levels should be determined before commencing glucocorticoids or mineralocorticoids for the treatment of elevated serum 17-OHP in disorders like non-classic adrenal hyperplasia (NCAH) and levels of 17- OHP, should be re-measured when vitamin D levels are replete to determine whether glucocorticoid/ mineralocorticoid replacement is actually necessary.
Keywords
Vitamin D deficiency; Glucocorticoid; Type 2 diabetes mellitus; Vitamin D Repletion; Hyperinsulinemia
Introduction
Vitamin D deficiency and abnormal glucose metabolism have been shown to be associated in humans and causally related in animal models [1,2], although the efficacy of vitamin D repletion/supplementation as a diabetes treatment is not yet universally accepted. We have previously reported that diverse interventions that reduce insulin resistance and hyperinsulinemia ameliorate non-classic adrenal hyperplasia (NCAH), biochemically and phenotypically, much as such interventions ameliorate polycystic ovarian syndrome (PCOS) [3,4].
We have also reported that NCAH is very frequently present in patients with Type 2 diabetes mellitus (T2DM), the quintessential disorder of insulin resistance, in our community who are not taking insulin sensitizers and have not developed T2DM in the setting of chronic Hepatitis C without a family history of T2DM [3,5]. Vitamin D repletion in patients who are vitamin D-deficient/insufficient mitigates insulin-resistanceassociated disorders such as T2DM, PCOS, and NCAH [1,2,4]; however, the present report is the first report of the amelioration of elevated serum 17-OHP during vitamin D repletion in a patient with likely NCAH.
Case Report
Our patient is a 59-year-old Afro-Caribbean male physician admitted to our Surgery Department for lower extremity infection/gangrene 2nd and 3rd toes of the left foot. The patient provided his informed consent to allow publication of his case. His temperature on admission was 38.1°C. His baseline haemoglobin A1c was 8.9%. His initial white blood count was 10.7 × 103/microliter with 74% neutrophils and mild thrombocytopenia. He appeared moderately ill. The Endocrine service was asked to see him to improve glycaemic control. Serum vitamin D level was performed per routine, as most of our in-patients are found to have hypovitaminosis D, and screening for non-classic adrenal hyperplasia (NCAH) was performed because he had T2DM, which we have previously reported to frequently be associated with NCAH [3-5].
On 5/5/2015 the patient’s unstimulated baseline serum 17- OHP concentration was markedly elevated to 2.3× the upper limit of normal at 460 ng/dl (27-199) as determined by highpressure liquid chromatography–tandem mass spectrometry. His baseline serum 25-OH-vitamin D concentration was moderately decreased at 24.7 ng/ml (30.0-100.0) as determined by immunochemiluminometric assay. Other measured serum adrenal steroid metabolites including 11- deoxycortisol, 17-OH-pregnenolone, and deoxycorticosterone were all within normal limits, thus excluding a generalized adrenal stress response to a severe infection, Cushing’s syndrome, or glucocorticoid resistance syndrome as possible explanations for the patient’s impressively elevated serum 17- OHP.
Our patient was treated with ergocalciferol, 50,000 IU orally weekly, with individualized diet, and titrated basal/bolus insulin therapy coupled with surgical removal of gangrenous tissue and parenteral, culture-guided antibiotic therapy.
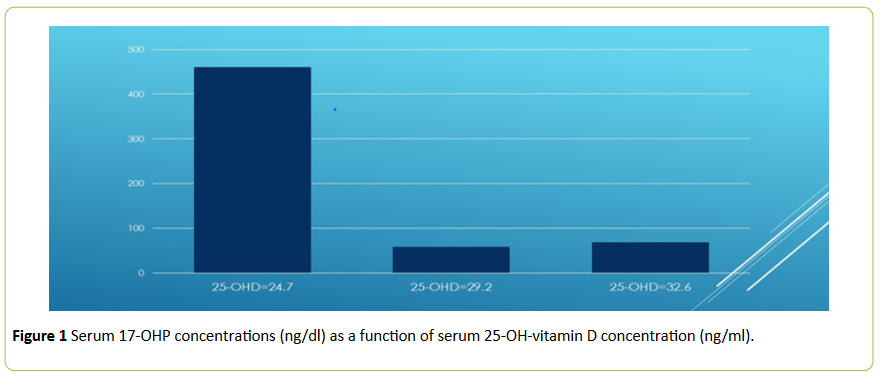
On 5/12/2015, his serum 17-OHP fell to 58 ng/dl and serum 25-OH-Vitamin D rose to 29.2 ng/ml (Figure 1). On 6/4/2015, serum 17-OHP remained normal at 69 ng/dl and serum 25-OHVitamin D normalized to 32.6 ng/ml (Figure 1). All of the blood samples were collected at 0600.
The outcome for the patient was normalization of serum 25- OHD, normalization of serum 17-OHP and improved glycemic control.
Discussion
In an effort to evaluate the treatment potential of vitamin D repletion in a patient presenting with T2DM, vitamin D insufficiency, and elevated serum 17-OHP, we assessed the possible effects of vitamin D repletion on biochemical improvement of the patient’s relevant abnormalities. Vitamin D repletion restored normal serum vitamin D levels and was associated with normalization of elevated serum 17-OHP. Vitamin D has been reported to be a regulator of 21- hydroxylase gene transcription [6]. As reported in this reference, under different circumstances, involving the balance between co-modulators and nuclear receptors, Vitamin D may either enhance or suppress the expression of the 21-hydroxylase gene, suggesting a possible role for Vitamin D as an adrenocortical adaptogen.
Although cosyntropin stimulation was not performed, it seems quite likely that our patient has non-classic 21- hydroxylase deficiency as baseline serum 17-OHP was already impressively elevated (>2.3× the upper limit of normal) and in a male patient, such as ours, there is no ovarian source of 17- OHP and thus, no possibility of diagnostic confusion between 21-hydroxylase deficiency and PCOS (where serum 17-OHP may be elevated due to LH and insulin stimulation of ovarian and adrenal 17-α-hydroxylase). Cosyntropin testing is of most value when there is a strong clinical suspicion for NCAH, yet baseline values are within the reference range or only mildly elevated. In such a setting cosyntropin testing serves to unmask heterozygotes as well as some homozygotes with functionally mild mutations. In female patients, such testing can help discriminate mild 17-OHP elevations due to NCAH from those due to polycystic ovarian syndrome. Although bacterial steroidogenesis has been reported, there are no published reports of 17-OHP synthesis by the organisms cultured in this patient (Pseudomonas sp., Corynebacterium sp., and Citrobacter sp.), and a non-specific, stress-mediated global hyperstimulation of the hypothalamic/pituitary/adrenal axis is unlikely since, as mentioned, no other measured adrenal steroid metabolite (17-OH-pregnenolone, 11- deoxycortisol, deoxycorticosterone) was elevated, as mentioned earlier. Applying Occam’s razor, there is actually no plausible alternative explanation for our patient’s isolated 17- OHP elevation other than NCAH and, as mentioned, we frequently encounter NCAH in patients with T2DM when we exhaustively test for all relevant steroid metabolites with and without co-syntropin stimulation.
Since this is a male patient we would not expect any abnormalities of growth or sexual development if he had NCAH (as opposed to the classic forms of congenital adrenal hyperplasia). As mentioned earlier, in our patient population, which may not be representative of the general world population, T2DM is reason enough to screen for NCAH [3-5].
Serum 25-OH-vitamin D levels have been reported to be lower than in the general population in many conditions associated with insulin resistance, including: obesity, T2DM, PCOS, and both classic and non-classic congenital adrenal hyperplasia [1-4]. Vitamin D receptors are abundant in the adrenal cortex [6], suggesting a possible direct regulatory role for vitamin D in the biosynthesis of adrenal steroids. In addition, vitamin D repletion/supplementation has been reported to improve insulin sensitivity and conditions associated with insulin resistance such as T2DM, PCOS, and both classic and non-classic 11-hydroxylase deficiencies [1,2,4]. The present report adds further support to the notion that vitamin D repletion/supplementation may be a valid treatment for insulin resistance and its associated comorbidities in the context of vitamin D deficiency/ insufficiency. It reinforces several emerging concepts: (1) Insulin resistance is associated with a number of conditions, such as non-classic 21-hydroxylase deficiency [7,8]; (2) interventions likely to improve insulin sensitivity often ameliorate co-morbidities associated with insulin resistance; (3) serum vitamin D is often deficient/insufficient in insulin resistant individuals; (4) disorders associated with insulin resistance may be mitigated in association with vitamin D repletion.
Vitamin D repletion in this setting restored normal vitamin D levels and was associated with normalization of serum 17-OHP. While some may regard the 32% increase in serum 25-OHD over the course of treatment as too trivial to explain the normalization of serum 17-OHP, it should be recalled that there is more active 1-α-hydroxylation of 25-OHD to the active form of the hormone in the setting of Vitamin D insufficiency/ deficiency, without hypocalcemia [9]. Thus, the increase in serum 1,25-(OH)2-Vitamin D3, might be of greater magnitude than the increase in serum 25-OHD. In addition, mean serum 25-OHD levels tend to be lower in Black patients than in other groups, in part due to lower mean levels of Vitamin D-binding protein [10]. Thus, the magnitude of the increase in bioavailable 25-OHD level may be greater than the magnitude of the increase in total 25-OHD. Our previously published experience with Vitamin D repletion in a patient with another form of congenital adrenal hyperplasia, classic 11-hydroxylase deficiency [11] in whom a modest increase in serum 25-OHD was associated with a dramatic drop in serum 11-deoxycortisol led us to somewhat expect that in the current patient, as well, modest increase in serum 25-OHD would be associated with a dramatic fall in 17-OHP.
We do not think it likely that our patient, while he probably has non-classic 21-hydroxylase deficiency, this was simply unmasked by the stress of acute infection pushing the hypothalamic/pituitary/adrenal (HPA) axis into overdrive and that the subsequent, rapid normalization of his serum 17-OHP was merely due to a reduction in stress as a result of resolution of his infection with subsequent dampening of HPA activity or that the increase in his serum 25-OHD was simply a bystander. Although his infection certainly improved he remained under a great deal of stress as a result of postsurgical pain and phantom pain associated with his amputation as well as the prospect of lengthy rehabilitation and considerable loss of income and mounting hospital bills during this period, thus his HPA axis likely remained very active. Beyond these considerations, as discussed in references [3,4,8]. We have reported these types of rapid responses to a number of insulin-sensitizing interventions. Future randomized double blind studies in patients with hypovitaminosis D and non-classic 21-hydroxylase deficiency should help to answer this question more definitively than can be done in the context of a case report.
Vitamin D levels should be determined before commencing glucocorticoid replacement for the treatment of elevated serum 17-OHP and levels of 17-OHP should be re-measured when vitamin D levels are replete to determine whether glucocorticoid and/or mineralocorticoid treatment is actually necessary.
Conclusion
Finally, the utility of treating an adult male patient with an asymptomatic elevation of serum 17-OHP might be argued; however, we were primarily treating his hypovitaminosis D in the interest of his bone health, his resistance to infection, and his insulin sensitivity. One can easily appreciate that the same intervention with the same percentage elevation of 17-OHP in a female patient with amenorrhea, acne, hirsutism, alopecia, or infertility might have been very clinically useful in addressing these issues. Furthermore, NCAH patients under extreme stress may experience adrenal crisis [12], possibly justifying its treatment even in asymptomatic patients.
References
- Mathieu C (2015)Vitamin D and diabetes: Where do we stand? Diabetes Res ClinPract 108:201-209.
- Al-Shoumer KA, Al-Essa TM (2015) Is there a relationship between vitamin D with insulin resistance and diabetes mellitus? World J Diabetes 6:1057-1064.
- Bahtiyar G, Sacerdote A (2011) Latest therapeutic advances in the treatment of congenital adrenal hyperplasia in adolescents and adults.publIntech65-90.
- Sacerdote A, Bahtiyar G (2015) Treatment of congenital adrenal hyperplasia by reducing insulin resistance and cysticercosis induced polycystic ovarian syndrome.publIntech.
- Sacerdote A (1995) Adrenal hyperandrogenemia in NIDDM. Diabetes Care 18:278-279.
- Lundqvist J, Wikvall K, Norlin M (2012) Vitamin D-mediated regulation of CYP21A2 transcription – A novel mechanism for vitamin D action. BiochimBiophysActa1820:1553-1559.
- Speiser PW, Serrat J, New MI, Gertner JM (1992) Insulin insensitivity in adrenal hyperplasia due to non-classical steroid 21-hydroxylase deficiency. J ClinEndocrinolMetab75:1421-1424.
- Saygili F, Oge A, Yilmaz C (2005) Hyperinsulinemia and insulin insensitivity in women with nonclassical congenital adrenal hyperplasia due to 21-hydroxylase deficiency: The relationship between serum leptin levels and chronic hyperinsulinemia. Horm Res 63:270-274.
- Booth BE, Tsai HC, Morris RC (1985) Vitamin D status regulates 25-hydroxyvitamin D3 1 alpha-hydroxylase and its responsiveness to parathyroid hormone in the chick. J Clin Invest75: 155-161.
- Powe CE, Evans MK, Wenger J, Zonderman AB, Berg AH, et al. (2013) Vitamin D-binding protein and vitamin D status of black Americans and white Americans. N Engl J Med369:1991-2000.
- Thomas N, Kalani A, Vincent R, Luis-Lam M, Bahtiyar G, et al. (2013) Effect of Vitamin D in a patient with classical adrenal hyperplasia due to 11- Hydroxylase deficiency. J Med Cases 4:569-575.
- Takasu N, Nakachi K,Higa H (2010) Development of Graves’ hyperthyroidism caused an adrenal crisis in a patient with previously unrecognized non-classical 21-hydroxylase deficiency. Inter Med 49:1395-1400.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences