An Unusual Etiology for Neurodevelopmental Delay and Epilepsy
Sai Sampath Kumar, Ravi Kiran, Sunanda Tirupathi, Anil Kumar and Sangamithra Gandra
Sai Sampath Kumar*, Ravi Kiran, Sunanda Tirupathi, Anil Kumar and Sangamithra Gandra
Department of Neurology, Narayana medical college, Nellore, Andhra pradesh, India
- *Corresponding Author:
- Sai Sampath Kumar
Department of Neurology
Narayana medical college
Nellore, Andhra pradesh, India
Tel: 0861 231 7968
E-mail: drnssampath123@gmail.com
Received date: January 22, 2016; Accepted date: April 29, 2016; Published date: May 03, 2016
Citation: Kumar SS, Kiran R, Tirupathi S, et al. An Unusual Etiology for Neurodevelopmental Delay and Epilepsy. Med Case Rep. 2016, 2:2.
Abstract
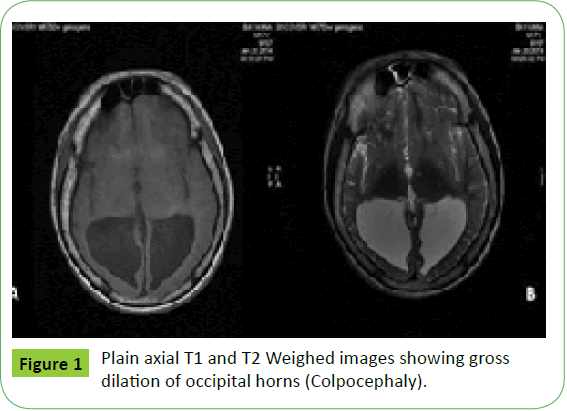
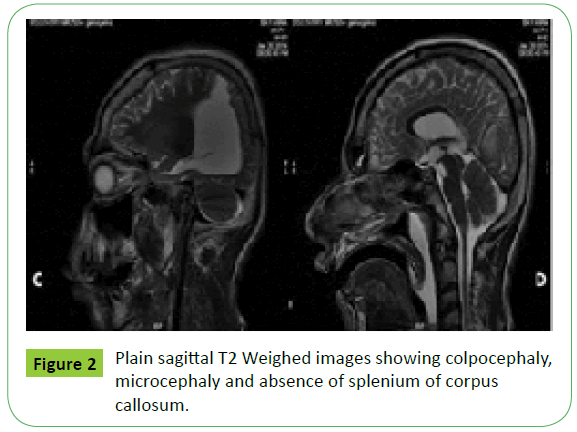
Colpocephaly is an abnormal enlargement of the occipital horn of the lateral ventricle, also described as persistence of the fetal configuration of the lateral ventricles. Since it was first described, colpocephaly has been found in association with several abnormalities of the brain. Various etiologies have been postulated, including intrauterine/perinatal injuries, genetic disorders, and an error of morphogenesis. We report a case of colpocephaly associated with absence of splenium of the corpus callosum presented with neurodevelopmental delay and epilepsy.
Keywords
Colpocephaly; Microcephaly; Corpus callosum dysgenesis; Epilepsy
Introduction
The corpus callosum is a band of approximately 200 million neural fibers that connects the left and right cerebral hemispheres. It begins to develop around the 12th week of gestation and matures through a complex process of neuronal migration and development [1]. By week 20, the corpus callosum can be seen using ultrasound examination or fetal MRI [2]. Although the corpus callosum may be considered fully developed by 4 years of age, as most neural structures, it is likely to change in the following years of life [3]. The corpus callosum has traditionally been viewed as having five distinct parts: the rostrum, genu, anterior midbody, isthmus, and splenium. The primary role of the corpus callosum is to facilitate communication between the hemispheres, using both inhibitory and excitory interhemispheric transfer [4].
Colpocephaly represents a disproportionate enlargement of the occipital horns of the lateral ventricles [5]. This does not represent hydrocephalus but may represent the reduction of ipsilateral cortical association tracts. It is a nonspecific finding and it can be associated with agenesis of the corpus callosum, Chiari malformation, lissencephaly and microcephaly.
The cause maybe a disorder in neuronal migration during early brain development, perinatal injuries or other central nervous system disorders [6]. Clinically the patients may present visual disturbances, spasticity and moderate mental retardation. Corpus callosum agenesis (CCA) is among the most common brain malformations observed in humans [7], its estimated prevalence is 3–7 per 1000 birth, while in children with developmental disabilities it is 2-3 per 100 [8]. It can occur either as an isolated malformation (isolated CCA) (49% of cases), or in association with another malformation syndrome, including malformation of the forebrain, secondary to intrauterine viral infections, toxic or metabolic disease, chromosomal abnormalities [9].
Case Report
A 17 year old male, 2nd born to non-consanguinous marriage brought to Emergency Department for Status epilepticus for which the patient was treated with Anti-Epileptic drugs according to the treatment protocol. Patient is a known epileptic since 5th month of age. Patient was on oral medications of Phenytoin and Leviteracetam orally with poor drug compliance with seizure recurrences at irregular intervals. Patient is dependent on family members for his activities of daily living with poor scholastic performance. The antenatal, natal and immediate post natal period were uneventful. Family history was insignificant. History of Global developmental delay. On examination in the emergency department patient is drowsy and arousable to repetitive verbal commands and, there is flexion of limbs with incomprehensible vocal response to the deep pain stimuli; Pupils reacting equally to light on both sides. Patient’s Vitals: Pulse: 98/min, Blood Pressure: 110/70 mmHg, Respiratory Rate: 20/min, regular. Patient has microcephaly [Head circumference 49 cm (<5th centile)] and Dysmorphic facies, with irregular shape of the skull with occipital protruberance, and low set ears, Spastic four limbs with exaggerated Deep Tendon Reflexes and Bilateral Plantar Extensors. Detailed sensory and cerebellar system examination could not be done because of the poor conscious level of the patient. Investigations like Hemogram, Renal function, Liver function, Lipid profile were within normal limits. Serum ammonia lactate was normal. MRI brain shows microcephaly, absence of splenium of corpus callosum, dysgenesis of corpus callosum and widely separated lateral ventricles with dilated occipital horns (colpocephaly [Figures 1 and 2].
Discussion
Callosal dysgenesis implies a malformation of the corpus collosum originating in the embryogenesis of the telencephalon. The term dysgenesis (malformation) includes three distinct categories: agenesis (total absence), hypogenesis (partial formation), and hypoplaisa (underdevelopment). The basis of this distinction relies on consideration about neural tube closure, formation and maintenance of the Massa commisuaralis inductive plate, and migration of the neuronal elements of the cerebral cortex responsible for the projection of the corpus callosum commissural fibers. These processes are somewhat interdependent in their expression resulting in a mosaic of callosal and cortical gray matter arrangement and hemispheric clinic-radiologic manifestations [10]. Colpocephaly has a typical association with mental retardation, seizures, motor and visual abnormalities.
Conclusion
The diagnosis of corpus callosum dysgenesis as well as colpocephaly is given by neuroimaging. Magnetic resonance imaging (MRI) is currently the imaging procedure of choice, as the CT scan could not show the small part of the corpus callosum. Prognosis depends on the extent and severity of malformations. It is not possible for the corpus callosum to regenerate or degenerate. Patient was treated symptomatically.
References
- Paul B, Adolphs W, Tyszka R, Richards J, Mukherjee L, et al(2007) Agenesis of the corpuscallosum: genetic, developmental and functional aspects of connectivity. Nature 8: 287-299.
- Cignini P, D’emidio L, Padula F, Girgenti A, Battistoni S et al(2010). The role of ultrasonography in the diagnosis offetal isolated complete agenesis of the corpus callosum: along-term prospective study. The Journal of Maternal-Fetal and Neonatal Medicine 23: 1504-1509.
- Keshavan M, Diwadkar V, Harenski K, Rosenberg D, Sweeney J, et al(2002) Abnormalities of the corpus callosum in first episode, treatment naive schizophrenia. Journal of Neurology, Neurosurgery & Psychiatry 72: 757-760.
- Witelson S(1989) Hand and sex differences in the isthmus and genu of the human corpus callosum: a postmortem morphological study. Brain 112: 799–835.
- Baker L, Barkovich J (1992)The large temporal horn: MR analysis in developmental brain anomalies versus hydrocephalus. Am J Neuroradiol13: 115-122.
- Mori K (1992)Giant inter-hemispheric cysts associated with agenesis of the corpus callosum. J Neurosurg 76: 224–230.
- DobynsW (1996)Absence makes the search grow longer. American Journal of Human Genetics 58: 7-16.
- Chiappedi M, BejorM (2010) Corpus callosum agenesis and rehabilitative treatment. Italian Journal of Pediatrics 36.
- Jeret J, Serur D, Wiesniewski K, Lubin R (1987)Clinico-pathological findings associated with agenesis of the corpus callosum. Brain Dev 9: 255-264.
- Jinkins R, Whitemore R, Brandley G(1989)MR Imaging of callosal and corticocallosal dysgenesis AJNR AM J Neuradiol 10:329-334.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences