An Interesting Case of Complete Androgen Insensitivity Syndrome (CAIS): Imaging Features in Ultrasound and MRI
Revanth RB*, Deepti Naik, Yashas Ullas L and Shanthala Sawkar
Department of Radio Diagnosis, SDUMC Tamaka, Kolar, India
- *Corresponding Author:
- Revanth RB
Department of Radio Diagnosis,
SDUMC Tamaka, Kolar,
India,
E-mail: revanthrbhat@gmail.com
Received date: August 16, 2022, Manuscript No. IPMCRS-22-14372; Editor Assigned date: August 19, 2022, PreQC No. IPMCRS-22-14372 (PQ); Reviewed date: August 29, 2022, QC No. IPMCRS-22-14372; Revised date: September 08, 2022, Manuscript No. IPMCRS-22-14372 (R); Published date: September 23, 2022, DOI: 10.36648/2471-8041.8.8.241.
Citation: Revanth RB, Naik D, Ullas LY, Sawkar S (2022) An Interesting Case of Complete Androgen Insensitivity Syndrome (CAIS): Imaging Features in Ultrasound and MRI. Med Case Rep Vol.8 No.8: 241.
Abstract
An X-linked recessive androgen receptor disorder is called complete androgen insensitivity syndrome. It is distinguished by a female XY karyotype phenotype. The external genitalia of the female are normal, but the Mullerian duct derivatives that is, the uterus, cervix and the proximal section of the vagina are absent. However, the intraabdominal, labial, or inguinal testes are present. Up to 5 males out of every 100,000 develop it. Prior to surgical intervention, imaging is crucial for gonad diagnosis and localization.
In this article, we present a case of primary amenorrhea in a teenager who had complete androgen insensitivity syndrome.
Keywords
Complete androgen insensitivity disorder; Xlinked recessive disorder; Karyotype
Introduction
Complete Androgen Insensitivity Syndrome (CAIS) as an Xlinked recessive condition in which there is a lack of or deficiency in the androgen receptor, preventing the end organs from responding to androgens [1]. Genetically speaking, they are males XY, but phenotypically and psychologically speaking, they are females [2]. They commonly appear with primary amenorrhea or infertility, feminine breasts, scant pubic and axillary hair, normal external genitalia and a short, blind vagina. Vagina, the top two-thirds of the uterus, and the tubes are missing. Testes are placed in the labia, inguinal canal, or intraabdominal areas. In this case of CAIS, the testes were found in the bilateral inguinal canal.
Case Report
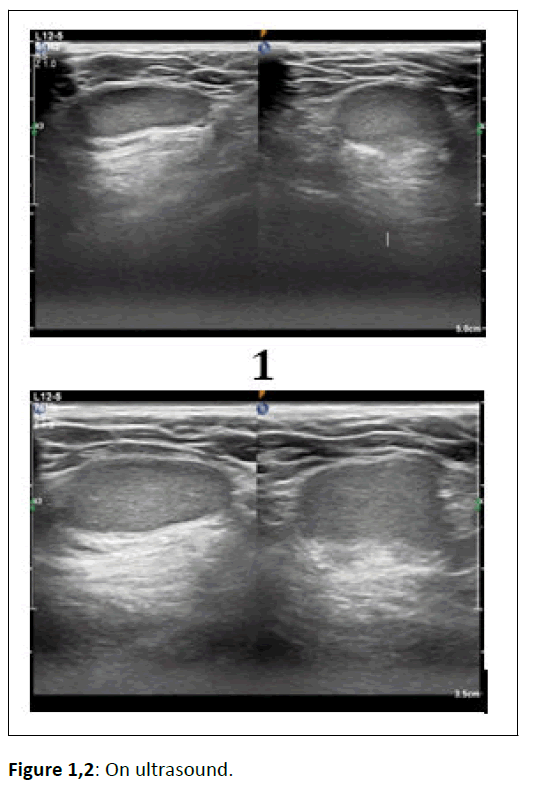
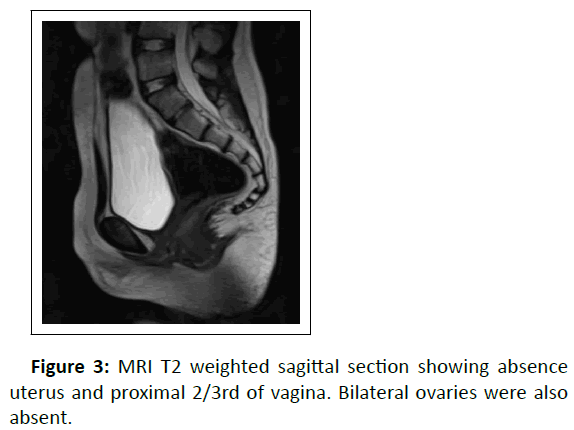
A 16 year old female patient presented with primary amenorrhea. Her vital signs were within normal limits, and her height was 165 cm, and her weight was 55 kg. The following are secondary sexual characteristics: Pubic and axillary hair was scanty and her breasts were undeveloped. Despite having a feminine external genitalia and a vagina with a blind pouch, she had a male karyotype [3,4]. She was sent to our division for additional assessment. Serum FSH was found to be 52 IU/L, LH was found to be 30 IU/L, estradiol was found to be 18 pg/ml and testosterone was found to be 2.6 ng/dl. She underwent ultrasound and MRI in our department. The imaging characteristics were as follows shown in figures 1-7.
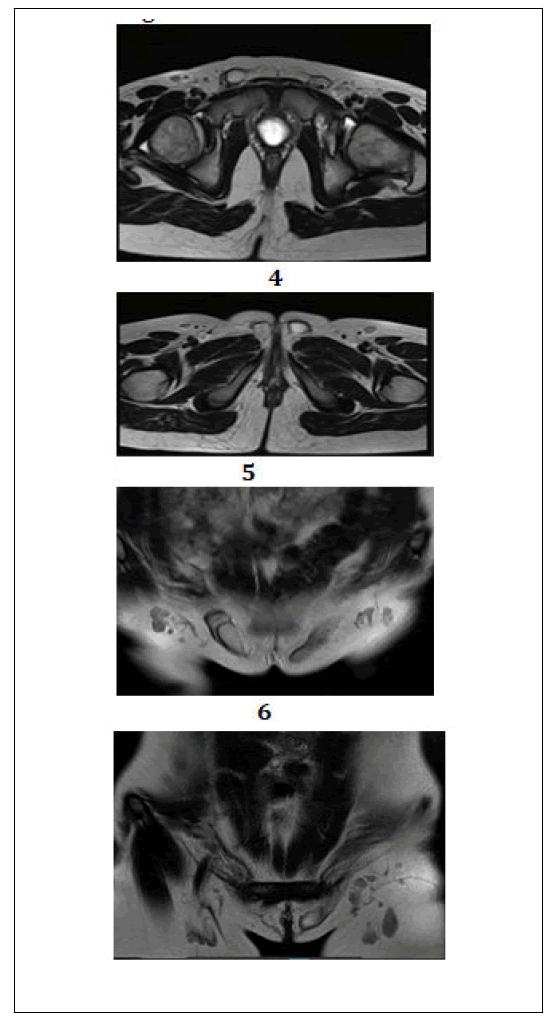
Figure 4,7: MRI T2 weighted axial and coronal sections showing two well-defined ovoid T2 hyperintense structures measuring 2.0 × 1.1 × 2.5 cm (TR × AP × CC); Vol~3 cc. on the right side in the right inguinal canal and 2.5 × 1.3 × 2.4 cm; Vol~4 cc. on the left in the left inguinal canal extending into the ipsilateral labia majora–likely testes.
Discussion
One of the most prevalent Disorders of Sex Development (DSD), CAIS was first identified as "testicular feminization syndrome" by American gynaecologist John Morris in 1953. CAIS is a rare, recessive X-linked condition in which genetic males (46,XY) exhibit phenotypic feminine external genitalia due to abnormalities of the Androgen Receptor (AR). Between 1/20,000 and 1/65,000, or 1–5/100,000 genetic males, are thought to be affected. There have been reports of over 1,000 distinct AR mutations, particularly on the proximal long arm of the X chromosome (Xq11–12).
A discrepancy between prenatal sex prediction and birth phenotype makes CAIS susceptible to accidental discovery in the first few days of life or in the event of monolateral or bilateral inguinal hernia in a young girl who has testicles, or in the case of a pelvic tumour in an adult. Until they exhibit primary amenorrhea during puberty, CAIS patients typically go undiagnosed. Because of the androgen-receptor-impaired function, patients with CAIS typically have a male karyotype and do not develop male genitalia or secondary sexual features despite normal testicularsynthesis of testosterone and dihydrotestosterone.
Before undergoing surgical procedures, imaging tests are required for diagnosing, evaluating, and detecting the gonads. Transabdominal Ultrasonography (US), which has a high sensitivity at the level of the inguinal canal, is the first line of evaluation for determining the presence or absence of mullerian structures and the position of testicles.
Due to its precise anatomical information, superior tissue characterisation and multiplanar capacity, Magnetic Resonance Imaging (MRI) is the gold standard for gonad diagnosis and localization as well as for the evaluation of mullerian abnormalities (accuracy, 100%). In instance, MRI is more sensitive than US for locating the gonads intra-abdominally and in the pelvis.
Results
As the patient has already been reared as a girl till the time of diagnosis, it is significant that a female gender identity may have already been present in some way subconsciously. Psychological effect also plays a significant role in the child's ongoing management.
The kid must be thoroughly informed, participated in all conversations with the attending doctors and included in deciding on the final choice.
Treatment of symptoms
CAIS may be treated by prepubertal gonadectomy in conjunction with oestrogen replacement treatment or removal of the testes after puberty when feminization is complete in order to prevent testicular cancer. The minimal risk of malignancy, however, is making the decision to remove the gonads increasingly controversial. Another CAIS therapy option is vaginal dilation to prevent dyspareunia. Similar to CAIS, prepubertal gonadectomy is more usually undertaken to help avoid the development of clitoromegaly during puberty in patients with PAIS who have predominantly female genitalia.
Conclusion
In situations of PAIS patients with ambiguous or mostly male genitalia, parents and healthcare professionals typically determine sex of rearing after an expert assessment has been completed. PAIS patients who were raised as males may have urologic treatments such orchiopexy and the repair of hypospadias. Combining oestrogen and androgen replacement therapy may be required if the gonadectomy is done after puberty and the PAIS patient is raised as a female. Men with MAIS could require mammoplasty for gynecomastia. Infant virilization may be aided by androgen pharmacotherapy. The afflicted person and family should be told of the AIS diagnosis in a caring environment with support from family and friends.
References
- Morris JM (1953) The syndrome of testicular feminization in male pseudohermaphrodites. Am J Obstet Gynecol. 65: 1192-1211.
[Crossref], [Google Scholar], [Indexed]
- Kore S, Chippa S, Khot R, Sarodey G, Kelkar S, et al. (2010)Testicular feminization syndrome. Bombay Hosp J 52:126-128.
[Crossref], [Google Scholar]
- Fauci A, Braunwald E, Kasper DL, Hauser S, Longo D, et al. (2008) Harrison's principles of internal medicine. (17th edition), McGraw Hill, New York.
- Pritsini F, Kanakis GA, Kyrgios I, Kotanidou EP, Litou E, et al. (2017) Psychological aspects of androgen insensitivity syndrome: Two cases illustrating therapeutically challenges. Case Rep Endocrinol 2017: 8313162.
[Crossref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences