Acute Liver Failure Induced by Joss Paper Ingestion
Barathi Sivasailam, Avnee Kumar, Ellen Marciniak and Janaki Deepak
Barathi Sivasailam, Avnee Kumar, Ellen Marciniak and Janaki Deepak*
Department of Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
- *Corresponding Author:
- Deepak J
Department of Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
Tel: + 410-328-2488
E-mail: jadeepak@som.umaryland.edu
Received date: March 23, 2019; Accepted date: April 23, 2019; Published date: April 30, 2019
Citation: Sivasailam B, Kumar A, Marciniak E, Deepak J (2019) Acute Liver Failure Induced by Joss Paper Ingestion. Med Case Rep Vol.5 No.2:96.
Abstract
We present a case of liver failure secondary to ingestion of Joss paper. A 44-year-old female initially presented with fever, nausea and vomiting and was subsequently diagnosed with acute liver failure. Prior to presentation she had consumed 1.3 gram of acetaminophen and 800 mg of ibuprofen. Her acetaminophen level was 18 mcg/mL initially and on repeat check was <10 mcg/ml and all viral hepatology antibodies and antigens were negative. History revealed that the patient ingested a ceremonial paper, Joss paper, daily, which is typically painted with heavy metals. Her mercury level was subsequently found to be elevated to 12 ug/L. Mercury can cause depletion of glutathione (GSH) through production of reactive oxygen species. Acetaminophen metabolism requires sufficient GSH to bind to a reactive metabolite to prevent cell death and hepatic injury. Daily exposure to mercury present in the Joss paper, likely accumulated in our patient’s body and allowed hepatic injury from even therapeutic doses of acetaminophen.
Keywords
Liver Failure; Viral hepatology; Antibodies and Antigens.
Introduction
Mercury has been recognized by the World Health Organization as a major public health concern. Exposure to mercury through ingestion, inhalation or physical contact can lead to neurologic and somatic symptoms [1]. While there have been some observational studies relating elevated liver enzyme levels and levels of mercury in the body, there are no known documented cases of fulminant liver failure in an adult attributed to mercury ingestion.
Acute liver failure has been attributed to a variety of causes, many of them drugs and toxins. In the United States, almost 50% of liver failure is a result of acetaminophen overdose. It is generally accepted that therapeutic doses of acetaminophen do not typically result in liver failure. Here, we report a case of fulminant liver failure in a patient with elevated mercury levels, which likely potentiated acetaminophen hepatotoxicity [2].
Case Presentation
A 44-year-old Vietnamese woman initially presented to her primary care physician with nausea, vomiting, myalgia and fever of 102 F. She had a medical history of hypertension and hypothyroidism and was prescribed hydrochlorothiazide and levothyroxine. The patient reported that she had taken 6 tablets of acetaminophen 325 mg (1.3 grams total) and 2 ibuprofen tablets (800 mg total). Two days prior to presentation, she had consumed tuna sushi and drank sake. She denied illicit drug use or tobacco use but did occasionally drink alcohol. She worked as an accountant and last travelled to Vietnam 1 year prior. At her primary care physician’s office, she was noted to be hypotensive and was sent to the hospital emergency room. On arrival to the hospital, the patient was awake and fully oriented, with mild diffuse abdominal tenderness.
Investigations
On admission, the patient’s AST was 7565, ALT 4891, total bilirubin 3.9, alkaline phosphatase 77, INR 1.8, and creatinine 1.7. Her acetaminophen level was 18 ug/mL and salicylate and ethanol <10. Urine toxicology was negative. She was then transferred to a tertiary care centre intensive care unit for further management of presumed acute liver failure.
Upon transfer, the patient’s AST was 6556, ALT 3335, total bilirubin 4.3, alkaline phosphatase 7, INR 2.9, creatinine 5.1, ammonia 176, and lactate 4.7. All viral serology including hepatitis A, hepatitis B, hepatitis C, human immunodeficiency virus, Epstein-Barr virus, adenovirus, and influenza returned negative. ANA, Anti-smAb and Anti-mAb were negative. Serum and urine copper and ceruloplasmin were within normal limits. Ultrasound guided liver biopsy revealed macro vesicular steatosis.
Family had suspected foul play on the part of the commonlaw husband and on further inquiry it was revealed that the patient burned and ingested sacred ceremonial paper called Joss paper as tea as part of a daily worship ritual. Joss paper, traditionally made of bamboo paper or rice paper, is painted with metal foil or with ink seals of various sizes. A sample of the Joss paper she used was analysed, which found high levels of mercury 0.02mcg/g and traces of copper, arsenic and iron.
Her mercury level was elevated at 12 ug/L (normal <5) and arsenic was 5.3 ug/L (normal 0).
Differential diagnosis:
• Heavy metal poisoning
• Acetaminophen toxicity
Treatment
The patient was admitted to the intensive care unit and treated with N-acetyl cysteine in spite of the Acetaminophen level and started on broad spectrum antibiotics as well as IV fluids. However, despite treatment she developed encephalopathy and altered mental status requiring intubation and mechanical ventilation for airway protection. She was given lactulose for hepatic encephalopathy but continued to decline.
Outcome and Follow-up
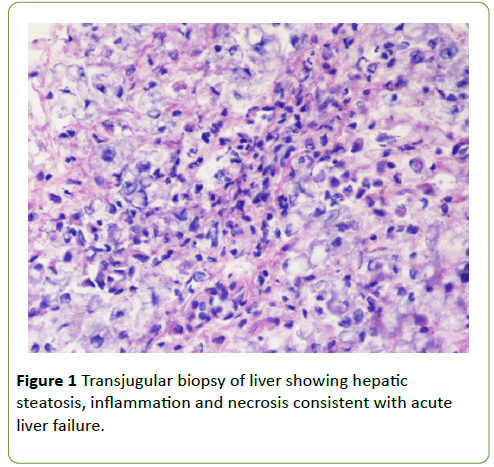
While in the ICU, the patient developed seizures, requiring several doses of Lorazepam and Propofol continuous infusion for treatment. She was evaluated by the liver transplant team and initially she was listed for transplant. However, she then became unresponsive despite discontinuation of sedatives. CT scan of the brain showed evidence of brain herniation and her exam was notable for loss of brainstem reflexes. Intracranial pressure monitoring was placed, with initial pressure was elevated to 90 mmHg. The patient was subsequently pronounced brain dead. Patient was a medical examiner case as per family wishes. The liver sections from autopsy were checked was stained for iron which was negative and showed steatosis, inflammation and necrosis (Figure 1). Post-mortem examination concluded that the cause of death was liver failure due to combination of acetaminophen use with concomitant mercury ingestion.
Discussion
Mercury toxicity can cause a variety of symptoms depending on the magnitude and duration of exposure, principally impacting the central nervous system and the kidneys. Typically, exposure to mercury is in the form of mercury containing fish consumption or dental amalgam use. Thus, exposure is from organic mercury such as methyl or dimethyl mercury [3]. This mercury is absorbed into the bloodstream through the intestine and adheres to sulflhydrl groups, such as on cysteine, and is distributed to peripheral tissues. Concentration of mercury occurs in the brain, liver, and kidneys and is slowly excreted, mostly through the stool. One mechanism of mercury toxicity is secondary to the production of reactive oxygen species and subsequent reduction of glutathione (GSH) [4].
The pathway of acetaminophen metabolism involves the creation of a reactive metabolite N-acetyl-p-benzoquinone imine (NAPQI). NAPQI is then bound to the sulfhydryl group of glutathione, which is then excreted in the urine. At supratherapeutic doses, excess NAPQI can deplete GSH stores, and instead bind to mitochondrial proteins and ion channels, which leads to cell death and hepatic injury [5,6]. In a patient with mercury accumulation, such as in our patient, levels of GSH are likely already partially depleted due to the production of reactive oxygen species. Thus, lower doses of acetaminophen may be sufficient to completely deplete GSH stores, even at therapeutic doses. In our case, the patient was known to use Joss Papers, which are sacred ceremonial papers that have been used in China to communicate with gods and goddesses in other worlds. It is traditionally made of coarse bamboo paper or rice paper. It often has metal foil or ink seals incorporated [7]. In the sample of paper provided by the patient’s family, there was evidence of several heavy metals including 0.02 ug/g of mercury. Compared to the mercury level of certain foods, such as swordfish, which has 100 ug/g of mercury, this is quite low. However daily exposure to small doses of mercury present in the Joss paper that our patient ingested daily likely accumulated in her body to a level that was clinically significant [8].
Conclusion
In our globalized society, physicians may not always have knowledge of the cultural rituals of their patients. Physicians should be aware of the diversity of these rituals and the potential for inadvertent heavy metal ingestion. In the case of acute liver failure, which is commonly caused by ingestion of drugs or other substances, obtaining a thorough history is important to eliciting the diagnosis. In addition, a medication history must include everything that the patient may be ingesting or inhaling, including over the counter medications and herbal supplements. As per current acute liver failure guidelines, N-acetylcysteine should be given to all patients where acetaminophen was known to be ingested or is suspected as the cause of liver injury. Mercury should be considered as a potential toxin that can be involved in the pathogenesis of liver injury.
Learning Points/Take Home Messages
When evaluating a patient with acute liver failure it is important to take a thorough history of all medications as well as anything the patient may be ingesting or inhaling.
N-acetylcysteine should be given to all patients where acetaminophen was known to be ingested or suspected even when checked levels are low or if full history is unknown.
Knowledge of our patient’s cultural background can be helpful in eliciting a diagnosis. Mercury should be considered as a potential toxin that can be involved in the pathogenesis of liver injury.
References
- Risher JF, Amler SN (2005) Mercury exposure: Evaluation and intervention the inappropriate use of chelating agents in the diagnosis and treatment of putative mercury poisoning. Neurotoxicology 26: 691-699.
- Lee WM, Squires Jr RH, Nyberg SL, Doo E, Hoofnagle JH (2008) Acute liver failure: A summary of a workshop. Hepatology 47: 1401-1415.
- Carocci A, Rovito N, Sinicropi MS, Genchi G (2014) Mercury toxicity and neurodegenerative effects. Rev Environ Contam Toxicol 229: 1-18.
- Bernhoft RA (2012) Mercury toxicity and treatment: A review of the literature. J Environ Public Health 2012: 1-10.
- Ramachandran A, Jaeschke H (2017) Mechanisms of acetaminophen hepatotoxicity and their translation to the human pathophysiology. J Clin Transl Res 3: 157-169.
- Mazaleuskaya LL, Sangkuhl K, Thorn CF, FitzGerald GA, Altman RB, et al. (2015) PharmGKB summary: Pathways of acetaminophen metabolism at the therapeutic versus toxic doses. Pharmacogenet Genomics 25: 416-426.
- Chew NK, Lee MK, Ali M, Tan CT (2003) Parkinsons disease in occupational exposure to joss paper: A report of two cases. Neurol Asia J 8: 117-20.
- Polson J, Lee WM (2005) American Association for the Study of Liver Disease. AASLD position paper: The management of acute liver failure. Hepatology 41: 1179-97.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences