A Rare Case of Uterine Didelphys in a Rural Based Tertiary Hospital in Southern Nigeria: The Role of Imaging in a Resource Poor Setting
Irabor Pamela Isioma1,2, Izevbekhai Stephen Ohikhuemei1*, Akhigbe Oriazo Theophilus1,2, Obi Egbedi-Ejakpovi E.B1,2 and Oriaifo Bosede1
1 Department of Radiology, Irrua Specialist Teaching Hospital, Irrua, Nigeria
2 Department of Radiology, Ambrose Alli University College of Medicine, Ekpoma, Nigeria
- *Corresponding Author:
- Izevbekhai Stephen Ohikhueme
Department of Radiology, Irrua Specialist Teaching Hospital, Irrua, Nigeria,
E-mail: steveizevbekhai@gmail.com
Received date: May 16, 2023, Manuscript No. IPMCRS-23-16663; Editor assigned date: May 18, 2023, Pre QC No. IPMCRS-23-16663 (PQ); Reviewed date: May 29, 2023, QC No. IPMCRS-23-16663; Revised date: June 06, 2023, Manuscript No. IPMCRS-23-16663 (R); Published date: June 12, 2023, DOI: 10.36648/2471-8041.9.5.296.
Citation: Irabor PI, Izevbekhai OS, Akhigbe OT, Obi-Egbedi-Ejakpovi EB, Oriaifo B (2023) A Rare Case of Uterine Didelphys in a Rural Based Tertiary Hospital in Southern Nigeria: The Role of Imaging in a Resource Poor Setting. Med Case Rep Vol.9 No. 5:296.
Abstract
Introduction: Uterine didelphys is a rare Müllerian duct anomaly of the female genital tract characterized by duplication of the uterine horn, body, cervix and occasionally the vagina.
Although, most cases of uterine didelphys are asymptomatic, some may present with gynaecological symptoms like dyspareunia, dysmenorrhoea, palpable lower abdominal swelling, recurrent miscarriages, preterm deliveries and fetal mal-presentations etc.
The diagnoses of uterine didelphys can be established with imaging modalities such as ultrasonography (pelvic), hysterosalpingography and magnetic resonance imaging; each modality having its own merits and demerits. However, the choice of a particular modality depends on the availability, cost and relevance in evaluating associated complications.
Ultrasonography and hysterosalpingography are invaluable tools for evaluating patients with uterine didelphys, with the latter being the gold standard. Both are cheap and readily available in an environment like ours. However, while ultrasonography is non-ionizing, hysterosalpingography utilizes conventional x-rays and contrast agents for outlining the uterine cavity and fallopian tubes.
Objectives: To report a rare case of uterine didelphys in a 29 year old patient who presented with eight years history of infertility.
To highlight the findings in imaging and also to review relevant existing literature pertaining to this condition.
Case report: A 29 years old nulliparous female patient who presented to the department of Radiology at Irrua Specialist Teaching Hospital, Nigeria for radio-diagnostic evaluation on account of eight years history of infertility. She came with a request for ultrasound scan and Hysterosalpingography (HSG) which were part of a barrage of investigations for infertility work-up by the gynecology unit of the hospital.
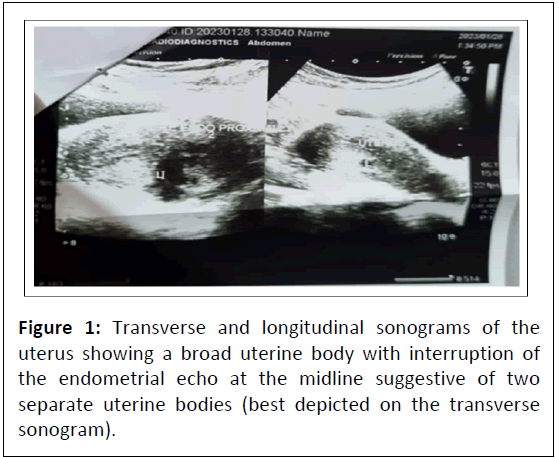
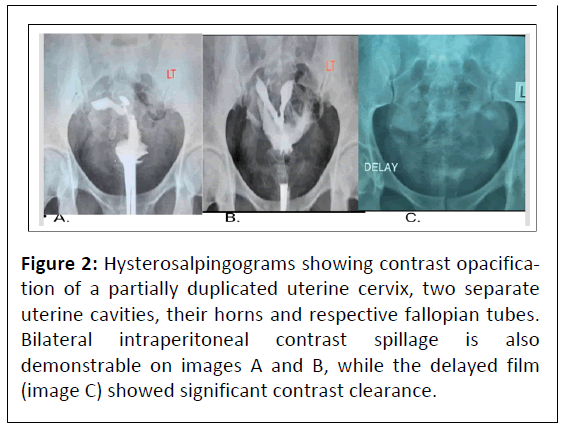
Initial pelvic ultrasonography using a Mindray ultrasonic scanner; DC-6 model (Shenzhen Mindray Biomedical Electronics Company Ltd, China 2016) with a low frequency (3-5 MHz) curved array transducer, revealed presence of two separate uterus; each with its own midline endometrial echo. These endometrial echoes were seen adjacent to one another on a transverse sonogram. Complementary hysterosalpingography done as requested, using 76% urografin, showed two moderate capacities but elongated contrast opacified uterine cavities, each with a single uterine horn and fallopian tube. The uterine outlines were irregular, with partial duplication of the cervix. This was affirmed by the difficulty in cannulation and uterine sounding. These findings confirmed the uterine didelphys initially suspected during sonography.
Conclusion: Ultrasonography and hysterosalpingography are indispensible tools for evaluating patients with Mullerian duct anomalies.
Keywords
Mullerian duct anomalies; Uterine didelphys; Hysterosalpingography; Ultrasonography; Irrua
Introduction
Mullerian Duct Abnormalities (MDA) are congenital defects of the female genital tracts that arises from abnormal embryological development of the Mullerian duct [1,2].
Uterine didelphys results from complete failure of fusion of the Mullerian duct and it is characterized by complete duplication of the uterine cavity, cervix and in some cases the vagina.
Malformation of the reproductive organs occur in approximately 4.3% and 3.5% of fertile and infertile women respectively, with septate and bicornuate uterus being the most commonly encountered defects accounting for about 35% and 25% respectively [3]. Uterine didelphys has been reported to account for approximately 8% of Mullerian duct anomalies [4].
Although, majority of cases are asymptomatic, some patients may present with dyspareunia and dysmenorrhea [1].
Uterine didelphys is commonly associated with adverse pregnancy outcomes such as recurrent miscarriages, intrauterine growth restriction, fetal mal-positioning and malpresentation, preterm deliveries and low birth weight [5].
Mullerian duct anomalies have previously been grouped into 4 major classes [6-8] viz:
• Incomplete or partial failure1 of the Mullerian duct development (agenesis; unicornate uterus without a rudimentary horn).
• Failure of the Mullerian ducts to canalize (unicornuate uterus with a rudimentary horn without proper cavities).
• Incomplete fusion of Mullerian ducts (bicornuate or dididelphys uterus).
• Incomplete resorption of uterine septum (septate or arcuate uterus).
Embryologically, the Mullerian ducts and Wolfian ducts, have a common origin, hence abnormalities of the urinary/renal system (a derivative of the latter) may occur in association with uterine abnormalities [9].
The diagnosis of uterine didelphys can be made using imaging modalities like; ultrasonography, Hysterosalpingography (HSG) and Magnetic Resonance Imaging (MRI). Ultrasography and hysterosalpingography are cheap and readily available modalities in Sub-Saharan Africa. Ultrasonography can assess the uterine wall and endometrium, the ovaries and adnexa. However, it is operator dependent. Hysterosalpingography is the gold standard of imaging. It is an invasive procedure that requires contrast injection into the uterine cavity via a canula/catheter anchored at the cervix, so as to opacify and outline the uterine cavity and evaluate the morphology and patency of the fallopian tubes. It requires the use of conventional x-rays and thus involves ionizing radiation. Magnetic resonance imaging is reserved for evaluating complex Mullerian duct anomalies due to its multiplanar capability, superior tissue characterization and large field of view. It can demonstrate the uterine contour, shape of uterine cavity, associated cervical and vagina anomalies. It may also help in classifying the anomaly, characterization of contents of obstructed cavities and also help in the detection of associated renal or ureteric abnormalities [10]. However, it is very expensive and not readily available.
Case Report
A 29 years old nulliparous female patient who presented to the radiology Department of Irrua Specialist Teaching Hospital in Nigeria, for radio-diagnostic evaluation on account of eight years history of sub-fertility. She came with a request for ultrasound scan and Hysterosalpingography (HSG).
The patient denied any history of use of contraceptive pills and devices, presence of dyspareunia or dysmenorrhea. She admitted that her menses were regular and normal in flow and duration.
Initial pelvic ultrasonography done using a Mindray ultrasonic scanner DC-6 model (Shenzhen Mindray Biomedical Electronics Company Ltd, China 2016) with a low frequency (3-5 MHz) curvilinear array transducer revealed presence of two separate uterus with an apparent single cervix; each with its own distinct endometrial echo. The endometrial stripes were demonstrable both in the longitudinal and transverse plane. The uterine myometrial echotexture was uniform with no demonstrable intrauterine mass lesion. The adnexa were also free.
Speculum examination of the vagina confirmed a single vagina with no longitudinal or transverse septum. There was some resistance to uterine sounding and cervical catheterization/ cannulation.
Complementary hysterosalpingography was done using about 40 mls of dilute 76% urograffin. Following contrast injection, we noted the presence of two moderate capacity contrast opacified uterine cavities with partial duplication of the cervix; each leading to a single uterine horn and fallopian tube. The uterine cavities were separated with irregular outlines. The opacified fallopian tubes demonstrated normal configuration and calibre with free intraperitoneal spillage of contrast which cleared significantly on the delayed film. The sonograms and hysterosalpingograms are shown in Figures 1 and 2.
Figure 2: Hysterosalpingograms showing contrast opacification of a partially duplicated uterine cervix, two separate uterine cavities, their horns and respective fallopian tubes. Bilateral intraperitoneal contrast spillage is also demonstrable on images A and B, while the delayed film (image C) showed significant contrast clearance.
Figure 2 is a series of spot films taken during hysterosalpingography. The hysterosalpingograms shows two separate contrast opacified moderate capacity uterine cavity with irregular outline and partial duplication of the cervix. Bilateral free intraperitoneal contrast spillage was also noted with adequate contrast clearance on the delayed film.
This patient had earlier undergone recent laboratory investigations like serum hormonal assay (follicle stimulating hormone, luteinizing hormone, prolactin, progesterone and estrogen), while her spouse had also previously done seminal fluid analysis. Their results had values which were within normal limits.
Result and Discussions
Uterine didelphys are asymptomatic in majority of cases thus making early diagnosis difficult. It is usually detected in women of reproductive age when they present for routine radiological investigations on account of infertility/subfertility, recurrent miscarriage and other complications. Although, it is thought that uterine didelphys is usually not a direct cause of infertility, conditions like recurrent pelvic inflammatory diseases and pelvic adhesions may coexist or complicate it, resulting in subfertility and poor pregnancy outcome [11].
Similarly, our patient fell within the reproductive age group and presented for routine investigative work-up for infertility management by a gynecologist. Although, this patient has had occasional pregnancies in the past terminating as early first trimester miscarriages, some studies (both local and international) have reported cases of uterine didelphys that successfully conceived and carried their pregnancies to term [5,12].
Varied clinical and imaging manifestations of uterine didelphys have previously been noted by some authors. One of these was the publication by Han, et al., [10] who reported a case of uterine didelphys associated with Obstructed Hemivagina and Ipsilateral Renal Anomaly (OHVIRA) syndrome in a teenager who presented with progressive cyclic lower abdominal pain and a large pelvic mass from hydrometrocolpos and left hydrosalpinx. Conversely, this present case has no evidence of an abdominal mass or renal anomaly. Menstrual symptoms are also absent in this current case. Uterine didelphys may be associated with a vagina septum in 75% of cases, thus resulting in obstruction of normal menses and its consequent accumulation resulting in hydrometrocolpos and unilateral hydrosalpinx [4].
Radiographic features of uterine didelphys have previously been described by Frank, et al., [4] to include divergent and separate uterine horns, as well as a presence of a large fundal cleft. The appearances seen on sonography and hysterosalpingography for this reported case closely mirrors the findings described by Frank, et al., [4].
Uterine didelphys can be differentiated from a bicornuate uterus in that in the latter, the uterine horns are separated by an acute fundal defect. Another differential diagnosis for uterine didelphys is septate uterus. However, in septate uteris, a thin midline uterine septum is usually demonstrable on imaging [4].
Conclusion
This case report shows that imaging plays an indispensable role in the diagnostic work-up of patients with infertility. In particular, it is valuable in diagnosing uterine didelphys and other Mullerian duct anomalies. Hysterosalpingography still remains the gold standard of imaging, as it can clear any IOTA of diagnostic doubt especially if the initial ultrasound finding is suggestive of a uterine anomaly.
References
- Ä?wiertnia A, Borzyszkowska D, Golara A, TuczyÅ?ska N, KozÅ?owski M, et al. (2022) The impact of uterus didelphys on fertility and pregnancy. Int J Environ Res Public Health 19: 10571.
[Crossref], [Google Scholar], [Indexed]
- Rezai S, Bisram P, Alcantara IL, Upadhyay R, Lara C, et al. (2015) Didelphys uterus: A case report and review of the literature. Case Rep Obstet 2015: 865821.
[Crossref], [Google Scholar], [Indexed]
- Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P (2001) Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod 7: 161–174.
[Crossref], [Google Scholar], [Indexed]
- Gaillard F, Yap J, El-Feky M (2023) Uterine didelphys. Radiopaedia.org 5: 1-24.
[Crossref], [Google Scholar]
- Awolude O, Olutoye A, Obajimi G (2022) Case report: Incidental finding of didelphys uterus in a multigravida woman at Caesarean delivery. F1000Research 11: 789.
[Crossref], [Google Scholar]
- Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P (2001) Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update 7: 161–174.
[Crossref], [Google Scholar], [Indexed]
- http://www.digitalpathology.uct.ac.za/topics/congenital_anomalies/uterus.html.
- Chandler TM, Machan LS, Cooperberg PL, Harris AC, Chang SD (2009) Müllerian duct anomalies: From diagnosis to intervention. Br J Radiol 82: 1034–1042.
[Crossref], [Google Scholar], [Indexed]
- Heinonen PK (2000) Clinical implications of the didelphic uterus: Long-term follow-up of 49 cases. Eur J Obstet Gynecol Reprod Biol 91: 183-190.
[Crossref], [Google Scholar], [Indexed]
- Boram H, Christopher NH, Mitchell PR, Wang JZ, Heike D (2010) Uterine didelphys associated with Obstructed Hemivagina and Ipsilateral Renal Anomaly(OHVIRA) syndrome. Radiol Case Rep 5: 327.
[Crossref], [Google Scholar], [Indexed]
- Chan YY, Jayaprakasan K, Tan A, Thornton JG, Coomarasamy A, et al. (2021) Reproductive outcomes in women with congenital uterine anomalies: A systematic review. Ultrasound Obstet Gynecol 38: 371-382.
[Crossref], [Google Scholar], [Indexed]
- Rezai S, Bisram P, Alcantara IL, Upadhyay R, Lara C, et al. (2015) Didelphys uterus: A case report and review of the literature. Case Rep Obstet Gynecol 2015: 865821.
[Crossref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences