A New Biological Technique of Elbow Reconstruction Following an Extensive Tumoral Resection of the Proximal Ulna
Sboui I, Jlalia Z, Riahi H, Bouaziz-Cheli M, Daghfous MS and Smida M
DOI10.21767/2471-8041.100055
Sboui I¹, Jlalia Z², Riahi H³, Bouaziz-Cheli M³, Daghfous MS¹ and Smida M¹
1Department of Orthopedics and Traumatology, Kassab Institute, Kasar Said-2010, Tunisia
2Faculty of Medicine of Tunis, Department of Pediatric Orthopedics, Kassab Institute, University of Tunis El-Manar, Kasar Said-2010, Tunisia
3Departement of Medical Radiology, Kassab Institute, Kasar Said-2010, Tunisia
- *Corresponding Author:
- Zied Jlalia
Faculty of Medicine of Tunis, Department of Pediatric Orthopedics
Kassab Institute, University of Tunis El- Manar, Kasar Said-2010, Tunisia
Tel: +00 216 21069395
E-mail: zied_j@yahoo.fr
Received Date: April 11, 2017; Accepted Date: May 14, 2017; Published Date: May 17, 2017
Citation: Sboui I, Jlalia Z, Riahi H. A New Biological Technique of Elbow Reconstruction Following an Extensive Tumoral Resection of the Proximal Ulna. Med Case Rep, 3:2. DOI: 10.21767/2471-8041.100055
Abstract
The resection of malignant tumors often poses the challenge of reconstruction. The objective of this reconstruction is the restoration of a function. We present the case of a chondroblastic osteosarcoma of the ulna in a 27-year-old patient. The resection sacrificed part of the ulna. The conservation of part of the olecrane allowed an innovative reconstruction to be carried out by bringing the radial head into contact with the humeral trochlea. The preservation of elbow function was satisfactory.
Keywords
Osteosarcoma; Elbow; Reconstruction
Introduction
Primary bone tumors around the elbow represent less than 1% of all the skeletal tumors [1]. Chondroblastic osteosarcoma is a relatively rare variant of osteosarcoma with an incidence of 4.2% [2,3]. But much lower than 21% and 23.8% in the series of Dahlin and Huvos [4,5]. The latter two series originate from specialized bone tumour referral centers, which may account for these differences. Differentiation between chondrosarcoma, osteosarcoma and chondroblastic osteosarcoma is relevant because of differences in treatment and prognosis. Current treatment of this type of tumor consists of chemotherapy and radical resection of the tumor. The defect produced after wide excision of the proximal ulna for malignant bone or soft tissue tumors presents a major reconstructive chalenge. Several reconstructive options have been described [6,7] these include the implantation of endoprosthesis, autogenous bone grafts, allografts, and other forms of reconstruction. Complications of these procedures include infection, fracture, nonunion, Charcot-type articular degeneration, prosthetic loosening, and prosthetic failure with fracture. We describe a new biological technique for the reconstruction of the elbow after resection of a proximal ulna tumor with the radio-ulnar union at the proximal articular surface of the ulna resulting in a single bone forearm and radius neck-to-humerus trochlea transposition.
Case Report
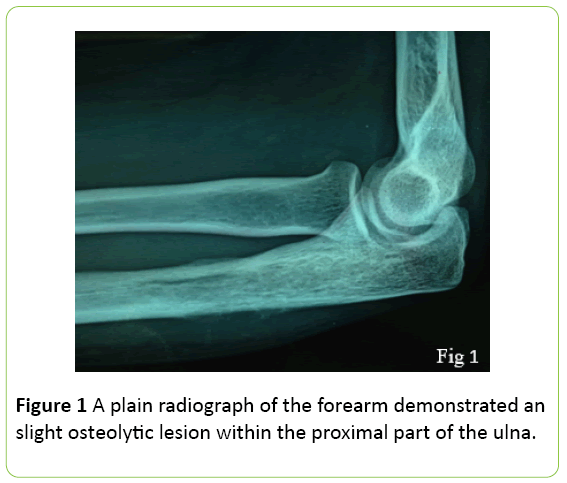
A 27-year-old woman presented with a 5-months history of repeated left elbow pain. Clinical examination revealed tenderness to palpation of the olecranon, without elbow distension. Elbow and wrist range of motion were normal, pronation and supination were restricted due to pain and no distal neurovascular deficiency was noted. A plain radiograph of the forearm demonstrated a slight osteolytic lesion within the proximal part of the ulna, with disorganized aggressive periosteal reaction without cortical rupture (Figure 1).
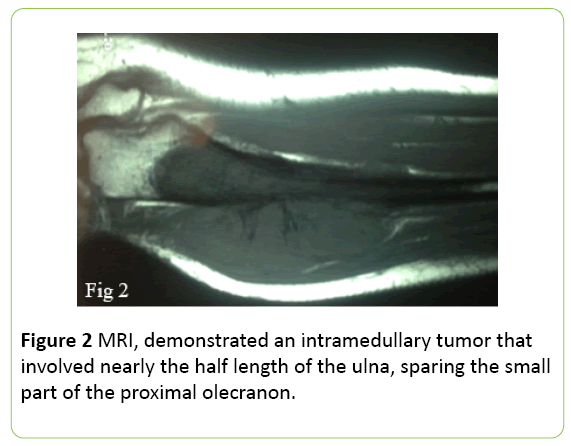
Magnetic resonance imaging (MRI) demonstrated an intramedullary tumor that involved nearly the half length of the ulna, sparing the small part of the proximal olecranon (Figure 2).
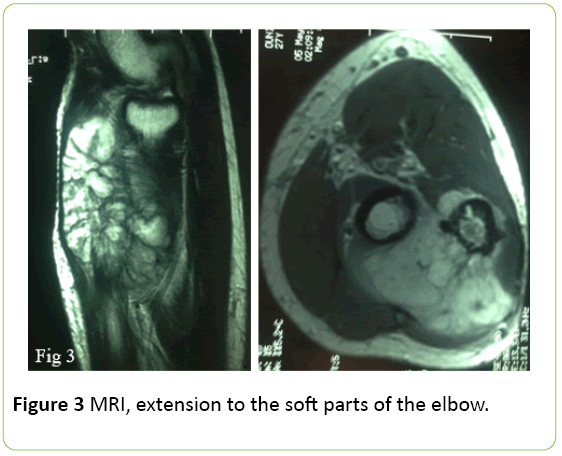
The surrounding cortex was partially involved; it was associated with an extension to the soft parts (Figure 3).
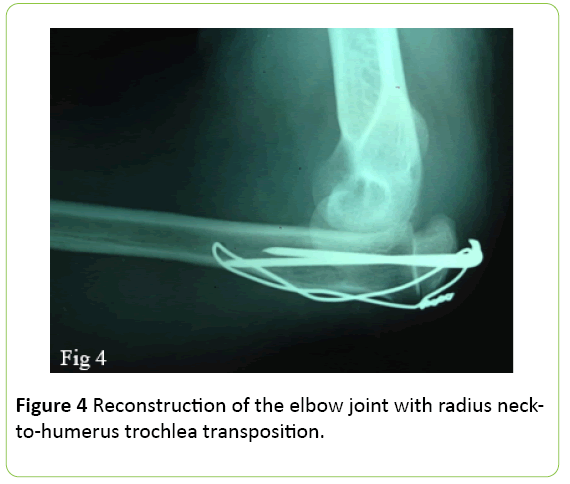
The elbow and wrist joints were tumor free. A biopsy of the olecranon showed neoplastic cells, which allowed for the diagnosis of chondroblastic osteosarcoma. Chest CT showed no evidence of metastatic disease and bone scintigraphy showed uptake only at the left ulna. Neo-adjuvant chemotherapy was started. Imaging studies performed after chemotherapy showed regression of the tumor. The patient was prepared for operative treatment, which consisted of resection of the proximal ulna and safe margin of normal appearing bone. Reconstruction of the elbow joint was done with radius neck-to-humerus trochlea transposition (Figure 4).
Surgical Technique
Under general anesthesia, the patient was operated in the supine position with a tourniquet. Tumor was exposed through posterior approach over the ulna from the distal humeral epiphysis along the edge of the ulna (Figure 5).
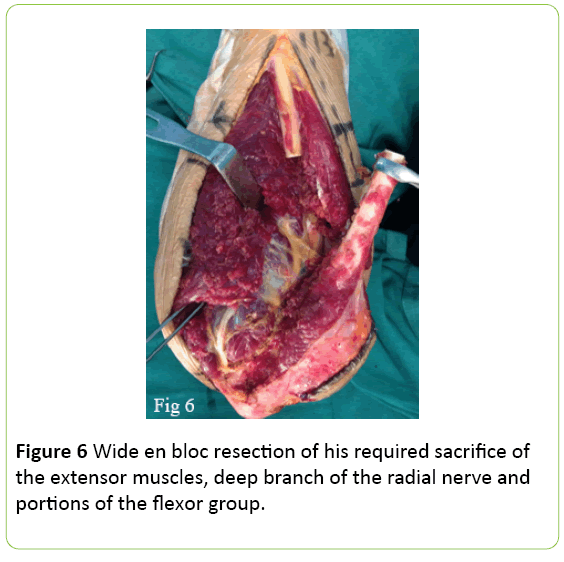
The incision involved the biopsy scar. Identification of ulnar nerve was conducted visually, and the structure was subsequent exposed within the olecranon. Furthermore, the adjacent portion of the median and vascular bundle were identified and conserved. Wide en bloc resection of his required sacrifice of the extensor muscles, deep branch of the radial nerve and portions of the flexor group (Figure 6).
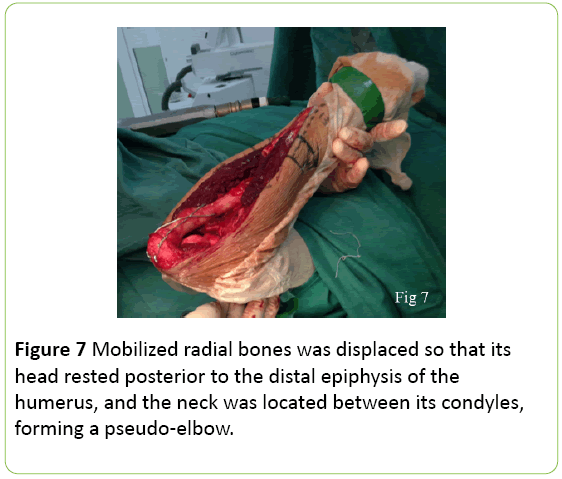
Muscles insertion and the interosseous membrane were gradually divided from the ulna. Having been completely isolated, the upper 16 cm of the ulna was resected except for half of the olecranon process with the attachment of the triceps tendon. Bone reconstruction was performed with the radius-to-trochlea transposition. In this technique, the mobilized radial bone was displaced so that its head rested posterior to the distal epiphysis of the humerus, and the neck was located between its condyles, forming a pseudo-elbow (Figure 7).
The stability of the construct is dependent on an intact biceps tendon at the bicipital tuberosity by providing a soft restriction to posterior translation of the relative to the humerus trochlea. The triceps tendon is attached to the amount of the proximal olecranon. This will allow subsequent extension and provide a restraint to anterior translation of the neck of the radius. The remaining stability is dependent on scar formation. The radial head was fixed to the remnant olecranon with pins and wires tension band. The forearm was fixed in a neutral position.
To protect the reconstructed elbow joint, 4 weeks of full immobilization with a cast at 90° flexion was applied after surgery, followed by an 6 weeks of passive and active assisted flexion and extension of the left elbow. The histopathological examination of the tumor from resected part of the ulna revealed chondroblastic osteosarcoma. Excision margins were clear of tumor. After surgery, the patient completed adjuvant chemotherapy. At the 3-year follow-up, there was no evidence of local recurrence or distant metastasis. At present, the patient has a good function with active movement of the elbow from 20° to 125° (flexion/extension), Prono-supination was absent. Furthermore, the patient is able to upon resuming normal daily activites.
Discussion
Malignant bone tumors are usually located in the lower extremities. Malignant bone tumors in the upper extremities, especially in the forearm, are rare [1]. Although there have been reports of osteochondroma primary giant cell tumors and Ewing’s sarcoma of the ulna. Salvaging the limb following an ulnar tumor resection poses a complex reconstructive challenge [8-11] options include resection arthroplasty, arthrodesis, resection-replantation [12], autografts [13,14], allografts [15], endoprostheses and radius neck-to-humerus trochlea transposition. Windrager and et al. Recommend resection-replantation, in wich the tumor-bearing area is resected as a cylindrical segment and the distal arm is replanted with shortening [12]. Autografts are an attractive biological option in the younger patient, but there are few reports of their use [13]. Free fibular grafts have been used frequently in orthopedics as a graft to bridge long bony gaps and very few cases to reconstruct joints. There have been reports of it being used to reconstruct elbow joints after resection of distal end of humerus [14,16]. But reconstruction of ulnar component of elbow has rarely been attempted. Usui et al. reported that the use of a free vascularized fibular graft including the heat carried a risk of fibular head collapse [17]. Vascularised fibula autografts have the potential to remodel and hypertrophy under mechanical head; however, they do not allow early weight bearing, they result in frequent complications and donor-site morbidity and are not considered suitable for large defects [18,19]. Allografts provide an alternative biological means of reconstructions, however, instability, fracture, nonunion and infection complicate their use, and the overall complication rate is high (70%) [15]. Certain prosthetic and patient criteria should be fulfilled for total elbow arthroplasty to be considered an acceptable reconstruction option. The prosthesis should allow stable motion of the hand and forearm, replace bone length, and have the mechanical strength to withstand daily use [20]. Total elbow arthroplasty should be performed only in patients with intact neurovascular structures providing function to the forearm and hand. Endoprostheses generally provide improved functional outcome and enable immediate commencement of adjuvant chemotherapy. Sperling et al. Reported 13 patients who underwent total elbow arthroplasty after excision of tumors at the distal humerus. On the other hand, there has been no report of total elbow arthroplasty after excision of tumors at the proximal ulna [21].
However, endoprosthetic reconstruction following distal humerus tumour resection has produced good functional and oncological results. Hanna et al. [22] reported 18 patients who had a distal humeral endoprosthetic replacement following malignant bone tumour resection. There are few reports on the use of endoprosthetic reconstruction following proximal ulna tumour [23,24], excision and their outcome is largely unknown. The main difference between a distal humeral and proximal ulna endoprosthetic reconstruction is the integrity of the triceps mechanism in the former, wich should provide superior function. However, these non-biological methods of reconstruction have higher rates of long-term complications such as implant loosening, postoperative infection and failure. There was no apparent compromise in patient survival following these various procedures. Delays in diagnosis, metastases, size, grade, location of primary tumour and reponse to chemotherapy are the most important factors affecting survival [25]. The procedure of radial neck articulation with the trochlea was first described by Enneking in 1983 [26], Dr. Cable young was the first to perform the procedure in severe trauma cases. The aim of the procedure was to provide a durable and stable reconstruction after complete tumor excision. Preservation of the proximal portion of the ulna with triceps attachement provides the necessary stability required for the elbow joint. This may be difficult to achieve if the total ulna is excised [27]. In this case, another similar type of surgical procedure was reported [28], which consisted of radius neck-to-humerus trochlea transposition and an inverted V-plasty of the triceps brachii muscle was attached in to an opening created in the center of the radial head.
Conclusion
Radius neck-to-humerus trochlea transposition with radioulnar synostosis can be considered as a new biologic salvage procedure after resection tumor at the proximal ulna provides a stable elbow with good function.
References
- Sewell MD, Hanna SA, Pollock RC, Aston WJ, Skinner JA, et al. (2012) Proximal ulna endoprosthetic replacement for bone tumours in young patients. IntOrthop 36: 1039-1044.
- Dorfman HD, Czerniak B (1995) Bone cancers. Cancer 75: 203-210.
- Schajowicz F (1993) Histological typing of bone tumours. Berlin Heidelberg, Springer, New York, USA.
- Unni KK (1996) Dahlin’s bone tumors: General aspects and data on 11 087 cases, (5edn) Charles C. Thomas Publishers, Springfield, IL, USA.
- Huvos AG (1991) Bone tumours. Diagnosis, treatment and prognosis. (2ndedn) WB Saunders Philadelphia, USA.
- Aberg M, Rydholm A, Holmberg J, Wieslander JB (1988) Reconstruction with a free vascularized fibular graft for malignant bone tumor. ActaOrthopScand 59: 430-437.
- Krepler P, Dominkus M, Toma CD, Kotz R (2003) Endoprosthesis management of the extremities of children after resection of primary malignant bone tumors. Ortho-pade 32: 1013-1019.
- Wang C, Lin N (2015) Ewing’s sarcoma of the ulna treated with sub-total resection and reconstruction using a non-vascularized, autogenous fibular graft and hernia mesh: A case report. Oncology Letters 10: 2067-2070.
- SuÃÆââ¬Â¦Ãâââ¬Å¡ko J (2013) Elbow reconstruction following an extensive resection of the proximal part of the ulna in a patient with Ewing Sarcoma. A case report. JBJS Case Connect 3: e111.
- Duncan SF, Athanasian EA, Healey JH (2008) Radius neck-to-humerus trochlea transposition for elbow reconstruction after resection of the proximal ulna: Report of 2 cases. J Hand Surg Am 33: 1384 1387.
- Goyal T, Rastogi S, Tripathy SK (2013) Desmoplastic fibroma of ulna: Excision and reconstruction of olecranon with a fibular graft. Indian J Orthop 47: 207 210.
- Windhager R, Millesi H, Kotz R (1995) Resection-replantation for primary malignant tumours of the arm. An alternative to for equarter amputation. J Bone Joint Surg Br 77: 176-184.
- Kimura K, Tatezaki S, Ishii T, Yonemoto T, Shigehara T, et al. (2002) Hemiarthroplasty of the elbow with a vascularised fibular graft after excision of Ewing’s Sarcoma of the proximal Ulna: A case report. Jpn J ClinOncol 32: 430-434.
- Gianoutsos MP, Marsden FW, McCarthy SW, Lee KK (1994) Ulnar adamantinoma: En bloc excision and fibular osteoseptocutaneous free flap reconstruction. J Hand Surg Am 19: 495-499.
- Dean GS, Holliger EH, Urbaniak JR (1997) Elbow allograft for reconstruction of the elbow with massive bone loss: Long term results. ClinOrthop 341: 12-22.
- Barnea Y, Amir A, Shlomo D, Cohen N, Zaretski A, et al. (2006) Free fibula flap elbow-joint hemiarthroplasty reconstruction for chronic osteomyelitis of the distal humerus. J ReconstrMicrosurg 22: 167-171.
- Usui M, Murakami T, Naito T, Wada T, Takahashi T, et al. (1996) Some Problems in wrist reconstruction after tumor resection with vascularized fibular-head graft. J ReconstrMicrosurg 12: 81-88.
- Chen CM, Disa JJ, Lee HY, Mehrara BJ, Hu QY, et al. (2007) Reconstruction of extremity long bone defects after sarcoma resection with vascularized fibula flaps: a 10-year review. PlastReconstrSurg 119: 915-924.
- Zaretski A, Amir A, Meller I, Leshem D, Kollender Y, et al. (2004) Free fibula long bone reconstruction in orthopedic oncology: a surgical algorithm for reconstructive options. PlastReconstrSurg 113: 1989-2000.
- Ross AC, Wilson JN, Scales JT (1987) Endoprosthetic replacement of the proximal humerus. J Bone Joint Surg 69B :652-655.
- Sperling JW, Pritchard DJ, Morrey BF (1999) Total elbow arthroplasty after resection of tumors at the elbow. ClinOrthop 367: 256-261.
- Hanna SA, David LA, Aston WJ, Gikas PD, Blunn GW, et al. (2007) Endoprosthetic replacement of the distal humerus following resection of bone tumours. JBJS Br 89: 1498-1503.
- Tang X, Guo W, Yang R, Tang S, Yang Y (2009) Custom-made prosthesis replacement for reconstruction of the elbow after tumor resection. JSES 18: 796-803.
- Weber KL, Lin PP, Yasko AW (2003) Complex segmental elbow reconstruction after tumor resection. ClinOrthop 415: 31-44.
- Skubitz KM, D’Adamo DR (2007) Review article. Sarcoma. Mayo ClinProc 82: 1409-1432.
- Enneking WF (1983) Musculoskeletal tumor surgery. Churchill Livingstone, New York, USA.
- Puri A, Gulia A, Byregowda S, Ramanujan V (2016) Reconstruction of the elbow and fore-arm for Ewing sarcoma of ulna: A new biological techniques. International Journal of Shoulder Surgery 10: 85-88.
- SuÃÆââ¬Â¦Ãâââ¬Å¡koJ(2013) Elbow reconstruction following an extensive resection of the proximal part of the ulna in a patient with Ewing sarcoma. JBJS Case Connect 3: e111.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences