Abstract
Pancreatitis, panniculitis, polyarthritis (PPP-) syndrome caused post-pancreatitis mesenteric vein necrosis. A case report
Pancreatic disease can rarely express itself by extraabdominal pathological processes. The symptomatic triad of pancreatic disease, panniculitis and polyarthritis, also known as PPP syndrome, is characterized by severe chronic episodes and high mortality rate. The pathognomic hallmark of PPP syndrome is fat necrosis in affected tissues. It is essential to identify its indicators due to complicated diagnosis procedure as a result of absent or mild abdominal symptoms. We report a case of 58-year-old male with a history of acute pancreatitis one year ago, admitted to University Hospital because of progressing feet joint arthritis, panniculitis, and febrile fever with chills lasting for approximately 2 weeks. Significantly increased levels of plasma lipase and α-amylase with inflammatory changes of blood and ascitic fluid were identified by laboratory testing, although patient did not complain of pancreatitis clinical symptoms. Inflammatory features of joints and surrounding soft tissues were detected during palmar ultrasound. Skin biopsy was not informative. Ascites, excessive oedematous changes in multiple organs were identified, whereas no pancreatic parenchymal changes were observed. Patient did not respond to applied treatment, and he died. Predominate peripancreatic steatonecrosis, superior mesenterial vein necrosis with perforation complicated by extensive steatonecrosis at omentum, liver, colon, local lymph nodes, and subcutaneous tissues were identified during an autopsy. Finally, this condition was named as PPP syndrome. Knowledge of association between panniculitis and polyarthritis with acute pancreatic disease may lead to a prompt diagnosis and management. Histopathological features of skin lesions can be a valuable clue for focusing attention to a pancreatic disease.
Author(s):
Neringa Musteikaite and Jurgita Makstiene
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 241
Medical Case Reports received 241 citations as per google scholar report
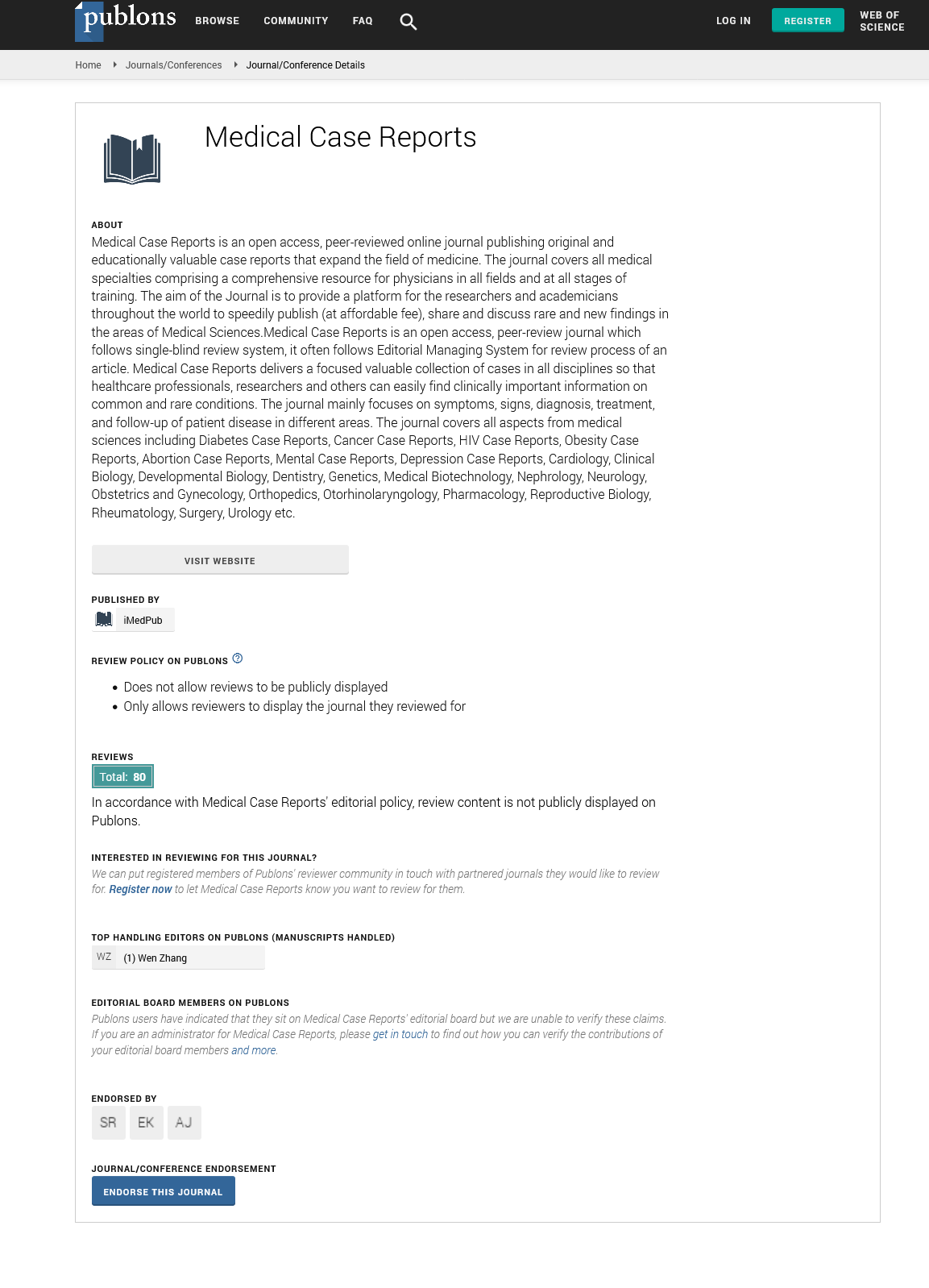
Medical Case Reports peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Cosmos IF
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Secret Search Engine Labs
- Euro Pub
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences