Wide Spread Skeletal Bones Involvements of Brown Tumors in A Patient with an Ectopic Mediastinal Parathyroid Adenoma: A Case Report and Review of Literature
Khalid SJ Aljabri, Areej A Bokhari, Samia A Bokhari, Muneera A Alshareef, Ahmad Alhumidi and Bandari K Aljabri
DOI10.21767/2471-8041.1000032
1Department of Endocrinology, King Fahad Armed Forces Hospital, Jeddah, Kingdom of Saudi Arabia
2Department of Surgery, King Saud University, Riyadh, Kingdom of Saudi Arabia
3Department of Pathology, King Khalid University Hospital, King Saud University, Riyadh, Saudi Arabia
4Faculty of Medicine, Um Al Qura University, Makkah, Saudi Arabia
- *Corresponding Author:
- Khalid SJ Aljabri
Department of Endocrinology, King Fahad Armed Forces Hospital, Jeddah, Kingdom of Saudi Arabia
Tel: 966555544919
Fax: 966(02)5760665
E-mail: khalidsaljabri@yahoo.com
Received date: June 23, 2016; Accepted date: September 27, 2016; Published date: September 30, 2016
Citation: Khalid Aljabri SJ, Areej Bokhari A, Samia Bokhari A et al., Wide Spread Skeletal Bones Involvements of Brown Tumors in A Patient with an Ectopic Mediastinal Parathyroid Adenoma: A Case Report and Review of Literature. Med Case Rep. 2016, 2:3. doi: 10.21767/2471-8041.1000007
Abstract
Primary Hyperparathyroidism presents uncommonly with unusual clinical manifestations in ectopically located Parathyroid gland adenomas. Brown tumor is an osseous lesion that can develop in bones affected by primary or secondary hyperparathyroidism. We report a case of a 29- year-old woman with diffuse brown tumor and ectopic mediastinal parathyroid gland adenoma.
Introduction
Primary Hyperparathyroidism presents uncommonly with unusual clinical manifestations in ectopically located Parathyroid gland adenomas. Inability to locate the adenoma may delay the diagnosis [1]. Intrathyroidal or other ectopic locations of parathyroid glands are uncommonly encountered [2]. Brown tumor is an osseous lesion that develops in bones affected by primary or secondary hyperparathyroidism, as a component of a metabolic bone disease known as osteitis fibrosa, cystica generalisata or Recklinghausen’s disease [3]. Brown tumors affect commonly the long bones, pelvic girdle, clavicle, ribs and the mandible. Tumors involving the maxillae are rare [4,5]. The reported prevalence of brown tumors is 0.1%, with a male to female ratio of 1: 3 with the disease is more common in persons older than 50 years [4,5]. Nuclear imaging scintigraphy accurately localizes the tumor in 90% of cases and simplifies the surgical management [2]. We encountered a case of 29-year- old woman with diffuse brown tumor and parathyroid gland adenoma in ectopic mediastinal location which that presented with diagnostic problems. Preoperative nuclear imaging helped in localizing the culprit lesion and in directing the surgeon to the affected gland.
Case Report
A 29-year female reported to King Khalid University hospital on wheelchair with non-healing fracture of both left arm and left leg after trivial fall for one-year duration. Casts were applied. She reported severe pain with no improvement after 9-month follow up.
She complained severely painful swelling at multiple sites including face, hands, arm and lower limbs that disabled her from standing up without support. She is known to have type 2 diabetes mellitus on oral hypoglemic medications and primary hypothyroidism on L- thyroxine 75 mcg daily for three years. The family history was non-contributory. When examined, she has multiple facial bony swelling mainly on right and left mandible and right maxilla (Figure 1).
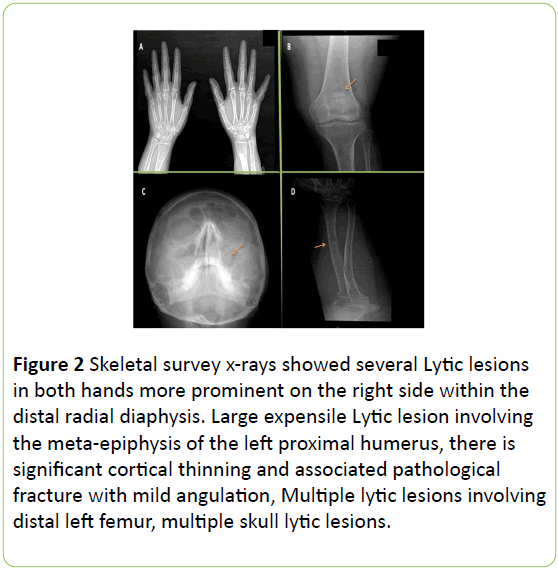
Left arm was on in a sling with tender swelling in at the head of the humerus with limited shoulder range of motion. Fingers were tender bilaterally with proximal bony joints swellings and there was limited range of movement in both hips associated with limping gait. Her corrected calcium was 3.1 mmol/L (2.1-2.55), Inorganic phosphorus: 0.86 mmol/L (0.87-1.45), Alkaline phosphates: 566 U/L (50-136), Parathyroid hormone (PTH): 41.1 PM/L (1.65-6.9) 25-Hydoxyvitamin D: 34.3 nmol/L (75-250), TSH: 16.47 MIU/L (0.25-5), Free T4: 7.5 PM/L (10.3-25.8) and HBA1, C: 7.40%. Skeletal survey x-rays showed several lytic lesions in both hands more prominent on the right side within the distal radial diaphysis. No spine lytic lesions, lytic lesion involved the right acetabular roof extending into iliac bone. Large expensile lytic lesion involved the metaepiphysis of the left proximal humerus and there is significant cortical thinning and associated pathological fracture with mild angulation, multiple lytic lesions involving distal left femur, proximal tibia bilaterally, distal right tibia with previous fracture of the distal tibiofibular diaphysis (Figure 2).
Figure 2: Skeletal survey x-rays showed several Lytic lesions in both hands more prominent on the right side within the distal radial diaphysis. Large expensile Lytic lesion involving the meta-epiphysis of the left proximal humerus, there is significant cortical thinning and associated pathological fracture with mild angulation, Multiple lytic lesions involving distal left femur, multiple skull lytic lesions.
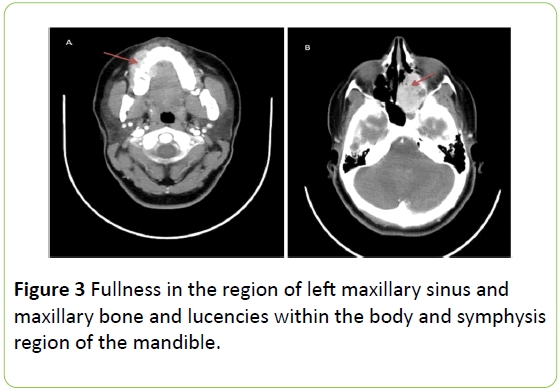
Fullness in the region of left maxillary sinus and maxillary bone and lucencies within the body and symphysis region of the mandible (Figure 3).
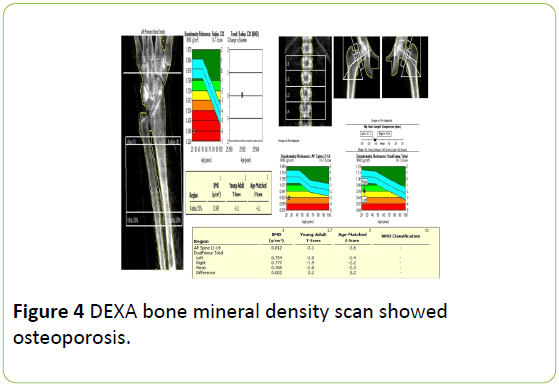
DEXA bone mineral density scan showed osteoporosis (Figure 4).
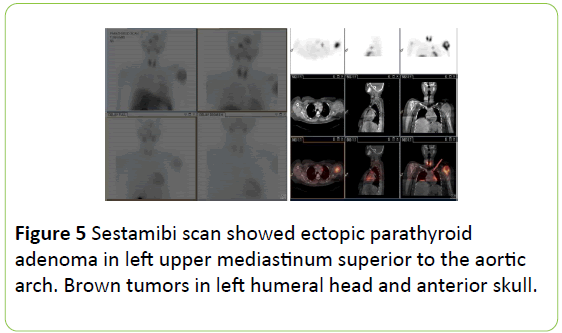
Sestamibi scan showed ectopic parathyroid adenoma in left upper mediastinum superior to the aortic arch. Brown tumors in left humeral head and anterior skull (Figure 5).
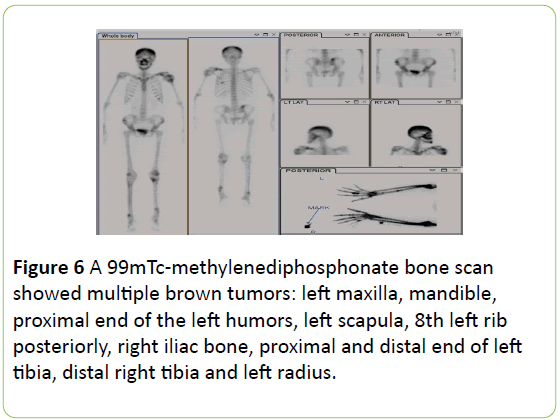
A 99mTc-methylenediphosphonate bone scan showed multiple brown tumors: left maxilla, mandible, proximal end of the left humors, left scapula, 8th left rib posteriorly, right iliac bone, proximal and distal end of left tibia, distal right tibia and left radius (Figure 6).
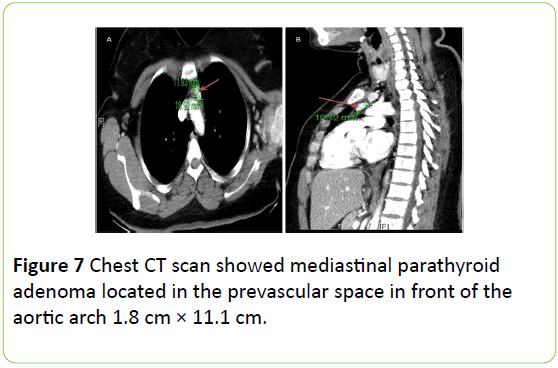
Neck ultrasound showed small thyroid nodules and there were no identified parathyroid glands. Neck and chest CT scan showed mediastinal parathyroid adenoma located in the prevascular space in front of the aortic arch 11.9 mm × 18.9 mm (Figure 7) correlating with the sestamibi scan.
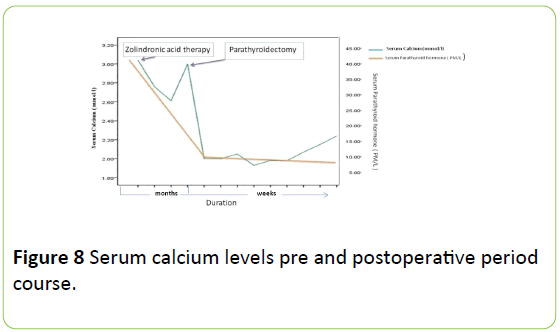
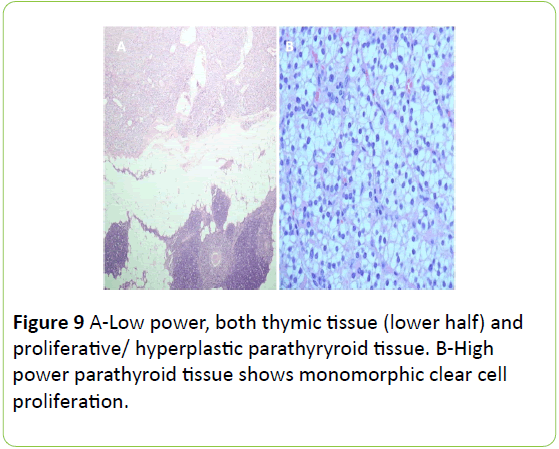
She was given zoledronic acid and vitamin D3 45000 IU weekly with bone profile monitoring as follow: corrected Ca: 2.9 mmol/L, inorganic phosphorous: 0.71 mmol/L, alkaline phosphates: 502 U/L, PTH: 37.7 PM/L, Vit D: 31.01 mmol/L Vitamin D3 400000 IU IM injection was given as her 25 hydroxyvitamin D was not optimal. As her localizing studies showed that it's ectopic in the mediestanium in front of the aortic arch that was approached thorcascopically. Pre excision PTH: 24.15 PM/L. with post excision by 10 min: 5.740 PM/L and corrected calcium 2.3 mmol/L (Figures 8 and 9 ).
Histopathology of the surgically removed ectopic parathyroid gland confirmed parathyroid adenoma. She was seen walking after three months in clinic with almost total resolution of her facial brown tumors (Figure 9).
Discussion
Sylvanus was the first to diagnose hyperparathyroidism in 1973. Primary hyperparathyroidism is the uncontrolled production of PTH with majority of cases are sporadic, and only a small number of patients have a hereditary component [6]. The underlying abnormality in sporadic hyperparathyroidism is typically a single hyper- functioning adenoma that produces an inappropriately high level of PTH relative to the serum calcium, hyperplasia and parathyroid carcinoma follow in order of decreasing incidence [7,8]. Diagnosis of primary hyperparathyroidism in a clinically suspected case is suggested by hypercalcemia, hypophosphatemia, raised levels of bone specific alkaline phosphatase and raised intact PTH levels. The bone changes result from the direct effect of PTH on bone, causing the conversion of potentially osteogenic cells from osteoblasts to osteoclasts, with bone resorption exceeding the formation of new osseous tissue [7]. Brown tumor is an osseous lesion that develops in bones affected by primary or secondary hyperparathyroidism, as a component of a metabolic bone disease known as osteitis fibrosa, cystica generalisata or Recklinghausen’s disease of bone. Recklinghausen is credited with the first description of the associated bone changes known as osteitis fibrosa cystic [9]. The name “tumor” is a misnomer because the lesion does not have a neoplastic potential, although invasive in some instances and should be differentiated from true giant cell tumors of bone. The common sites of brown tumors are the long bones, pelvic girdle, clavicle, ribs and the mandible. Radiographically, brown tumors appear as well-defined marginated expansile lytic lesions and may cause cortical expansion. Concurrent bone changes associated with hyperparathyroidism, such as generalized demineralization of the medullary bones of the jaw and loss of lamina dura around the roots of teeth, can help differentiate brown tumors from other processes [10,11]. The superior and the inferior parathyroid glands originate from the 4th and the 3rd branchial pouches respectively and migrate caudally to occupy their normal positions in relation to the thyroid gland. Any aberrancy during this descent may lead to ectopic locations of these glands. They may be located in 20% in the mediastinum either the posterior mediastinum behind the cervical esophagus, retrosternally in the anterior mediastinum, within the thymus (intrathymic) in 70% of cases, in the tracheo-esophageal groove or unusually within the thyroid parenchyma (intrathyroidal). Pre-operative 99mTc sestamibi scan helps in localizing the tumor accurately in almost 90% of patients [2]. It has a greater role in localizing ectopic glands which helps the surgeon in planning the surgical approach, as in our case [2]. Treatment of hyperparathyroidism is the first step in the management of brown tumor. After appropriate medical or surgical treatment of the underlying endocrine abnormality, brown tumor may regress, and almost all radiographic changes tend to return to normal [9]. Intraoperative parathyroid hormone levels are measured as a baseline immediately after induction of anesthesia, before excision, and 10 minutes after excision of parathyroid tissue. If the initial excision is not sufficient to adequately lower serum PTH levels (a 50% or more decline from baseline), the surgeon can take more tissue until the hormone levels fall to an appropriate level. Intraoperative PTH assays have replaced tissue analysis by frozen section and provided a more effective screen for surgical success [12,13]. Grossly, a brown tumor appears as a mass with partly cystic and partly solid areas. Microscopically, brown tumors are characterized by intensely vascular fibroblastic stroma serving as a background for numerous osteoclast-like multinucleated giant cells [3]. Cysts develop as a result of intraosseous bleeding and tissue degeneration.
The cystic spaces are filled up by clusters of giant cells, hemosiderin-laden macrophages and plump fibroblasts. The presence of hemorrhage, hemosiderin and hypervascularity leads to the brownish color, and thus the name. Histological features alone cannot establish a certain diagnosis of a brown tumor. However, a clinical history of more wide spread skeletal involvement, pathological fractures and renal stones may suggest the presence of primary hyperparathyroidism. The diagnosis is readily confirmed by establishing elevated serum calcium and PTH levels. In some cases, the postoperative hypocalcemia is severe and prolonged, despite normal or even elevated levels of PTH. This phenomenon, called the hungry bone syndrome, most often occurs in patients who have developed bone disease preoperatively due to a chronic increase in bone resorption induced by high levels of PTH (osteitis fibrosa) [14]. Given the frequency of vitamin D deficiency in the hemodialysis population, most physicians recommend preoperative administration of calcitriol to all such patients, if they are not already being treated with a vitamin D metabolite. A few case reports and several retrospective studies have suggested a possible role for the preoperative administration of bisphosphonates as another preventive measure [15]. In these reports, bisphosphonates were used to treat hypercalcemia in patients with severe primary and secondary hyperparathyroidism prior to parathyroidectomy [16,17]. As in our patient, she did not have hungry bone syndrome as she was treated with vitamin D and biphosphonate preoperatively.
Conclusion
In conclusion this is the first reported case to our knowledge of wide spread skeletal involvement of a brown tumor presented as the first sign of primary hyperparathyroidism due to an ectopic parathyroid.
References
- Mitlak B, Daly M, Potts JJ (1991) Asymptomatic primary hyperparathyroidism. J Bone Miner Res. 6: S103-S110.
- Gogas J, Kouskos E, Mantas D, Markopoulos C, Kyriaki D, et al. (2003) Pre-operative Tc-99m-sestamibi scanning and intra-operative nuclear mapping: Are they accurate in localizing parathyroid adenoma? Acta Chir Belg.103: 626-630.
- Gnepp DR (1997) Diagnostic surgical pathology of the head and neck. (2ndedn). Philadelphia: WB Saunders Co. 781.
- Jebasingh F, Jacob JJ, Shah A, Paul TV, Seshadri MS (2008) Bilateral maxillary brown tumors as the first presentation of primary hyperparathyroidism. Oral Maxillofac Surg. 12: 97-100.
- Proimos E, Chimona TS, Tamiolakis D, Tzanakakis MG, Papadakis CE (2009) Brown tumor of the maxillary sinus in a patient with primary hyperparathyroidism: a case report. J Med Case Rep. 6: 7495.
- Lew JI, Solorzano CC (2009) Surgical management of primary hyperparathyroidism: state of the art. Surg Clin North Am. 89: 1205-1225.
- Levin KE, Clark OH (1989) The reasons for failure in parathyroid operations. Arch Surg 124: 911-914.
- Neville BW, Damm DD, Allen CM, Bouquot JE (2002) Oral and maxillofacial pathology. (2ndedn), Pennsylvania: Saunders. p: 724-726.
- Auclair PL, Avendt DM, Hellstein JW (1997) Giant cell lesions of the jaws. Oral Maxillofac Surg Clin North Am 9: 655-680.
- Cruz Vigo FDl, Ortega G, Gonzalez S, Martinez JI, Cruz Leiva J, et al. (1997) Pathologic intrathyroidal parathyroid glands. Int Surg. 82: 87-90.
- Scholl RJ, Kellett HN, Neumann DP, Lurie AG (1999) Cysts and cystic lesions of the mandible: Clinical, radiologic and histopathologic review. Radiographics. 19: 1107-1124.
- Mandell DL, Genden EM, Mechanick JI, Bergman DA, Diamond EJ (2001) The influence of intraoperative parathyroid hormone monitoring on the surgical management of hyperparathyroidism. Arch Otolaryngol Head Neck Surg. 127: 821-827.
- Irvin GL, Solorzano CC, Carneiro DM (2004) Quick intraoperative parathyroid hormone assay: surgical adjunct to allow limited para-thyroidectomy, improve success rate, and predict outcome. World J Surg. 28: 1287-1292
- Brasier AR, Nussbaum SR (1988) Hungry bone syndrome: clinical and biochemical predictors of its occurrence after parathyroid surgery. Am J Med 84: 654.
- Lee IT, Sheu WH, Tu ST (2006) Bisphosphonate pretreatment attenuates hungry bone syndrome postoperatively in subjects with primary hyperparathyroidism. J Bone Miner Metab 24: 255.
- Kumar A, Ralston SH (1996) Bisphosphonates prevent the hungry bone syndrome. Nephron 74: 729.
- Davenport A, Stearns MP (2007) Administration of pamidronate helps prevent immediate post-parathyroidectomy hungry bone syndrome. Nephrology (Carlton) 12: 386.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences