Spontaneous Pneumothorax in a Non-Mechanically Ventilated COVID-19 Patient
Priya Jha, Kathryn JO Connell and Sama Alreddawi
Published Date: 2022-05-20DOI10.36648/2471-8041/8.5.226
Priya Jha*, Kathryn JO Connell and Sama Alreddawi
Department of Computer Science, SNDT Women's University, United States
- *Corresponding Author:
- Priya Jha
Department of Computer Science, SNDT Women's University, United States
Tel: 8482489864
E-mail: pjha5290@gmail.com
Received date: March 16, 2022, Manuscript No. IPMCRS-22-12381; Editor assigned date: March 19, 2022, PreQC No. IPMCRS-22-12381 (PQ); Reviewed date: April 04, 2022, QC No. IPMCRS-22-12381; Revised date: May 13, 2022, Manuscript No. IPMCRS-22-12381 (R); Published date: May 20, 2022, DOI: 10.36648/2471-8041/8.4.226
Citation: Jha P, O’Connell JK, Alreddawi S (2022) Spontaneous Pneumothorax in a Non-Mechanically Ventilated COVID 19 Patient. Med Case
Rep Vol:8 No:5
Abstract
Background
The outbreak of Corona Virus Disease-19 (COVID-19) was initially reported in Wuhan, China in December 2019. The disease was officially named COVID-19 by World Health Organization (WHO) on February 11, 2020. Most patients presented with symptoms of the upper respiratory tract, such as fever, dry cough, shortness of breath, and fatigue. However, other symptoms such as gastrointestinal disturbances, loss of smell and taste were also noted. Coronaviruses are enveloped positive-stranded Ribo Nucleic Acid (RNA) viruses.
Patients are diagnosed via real time Polymerase Chain Reaction (PCR) and imaging findings are characterized with ground glass opacities. Complications from the virus include but not limited to Acute Respiratory Distress Syndrome (ARDS), arrhythmias, acute cardiac injury, shock, cardiomyopathy, pulmonary embolism, acute stroke, encephalopathy, Guillain Barre, secondary infections, pneumomediastinum, and pneumothorax. We present a case of spontaneous pneumothorax in a non-smoker patient who did not require any mechanical ventilation or have any prior pulmonary illnesses as a risk factor.
Case Presentation
Our patient is a 75 years old man with a past medical history of hyperlipidemia and hypertension who presented to the emergency department with shortness of breath, cough, and a fever. He was diagnosed with COVID-19 three days prior to his admission with symptoms starting nine days prior to his diagnosis of COVID-19. His symptoms progressively worsened with muscle aches, generalized weakness, exertional dyspnea leading to his presentation to the hospital.
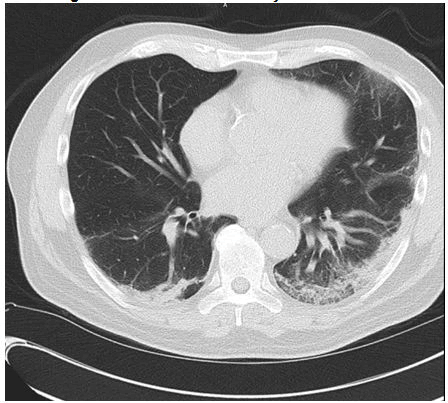
Initially, he was started on 4-liter supplemental oxygen to achieve saturation of peripheral oxygen (SpO2) >92%. A Computer Tomography (CT) of his chest was obtained on the day of his admission which showed the extent of COVID-19 affecting his lungs. Six days into his admission, he required transitioning to High Flow Nasal Cannula (HFNC) for increased oxygenation demand and worsening infiltrates on chest x-ray. He was treated with five days of Remdesivir and ten days of Dexamethasone (Table 1).
| DAY 1 | DAY 2 | DAY 3 | DAY 4 | DAY 5 | DAY 6 | DAY 7 | DAY 8 | DAY 9 |
DAY 10 | DAY 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Remdesivir | X | X | X | X | X | ||||||
| Decadron | X | X | X | X | X | X | X | X | X | X | |
| Oxygen | NC | NC | NC | NC | NC | HFNC | HFNC | HFNC | HFNC | NC | NC |
| Chest Tube | |||||||||||
| Pneumothorax | |||||||||||
| DAY 12 | DAY 13 | DAY 14 | DAY 15 | DAY 16 | DAY 17 | DAY 18 | DAY 19 | DAY 20 | DAY 21 | DAY 22 | |
| Remdesivir | |||||||||||
| Decadron | |||||||||||
| Oxygen | HFNC | HFNC | NC | NC | NC | NC | NC | NC | Room Air | Room Air | Room Air |
| Chest Tube | X | X | X | X | X | X | X | X | X | X | |
| Pneumothorax | X | X |
Table 1: Hospital Course
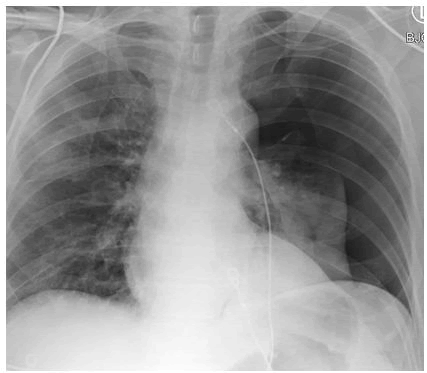
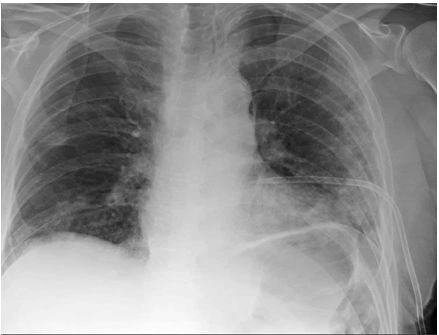
After five days of oxygenation via HFNC, he started to require less oxygen and was transitioned to nasal cannula. The following day, the patient had sudden hypoxia (SpO2 ~70%) with a near syncopal episode. A stat chest x-ray showed a large left pneumothorax. He required oxygen via HFNC and placement of a chest tube which showed immediate improvement of oxygenation and re-expansion of his lungs. The next few days, he was finally off of any supplemental oxygen. His chest tube was managed by a few days of going back and forth between water seal and suction due to recurrence of the pneumothorax. Eventually, his chest tube was clamped and removed with no recurrence of the pneumothorax and the patient was discharged home (Figures 1-3).
Discussion
Pneumothorax occurs when the lung collapses secondary to air entering the pleural space. This can be further classified into spontaneous vs. traumatic. Spontaneous pneumothorax can be due to primary or secondary causes. The primary causes do not have any associations with an underlying lung disease. Whereas secondary causes are due to underlying lung diseases such as Chronic Obstructive Pulmonary Disease (COPD), emphysema, cystic fibrosis, or lung malignancy. Traumatic pneumothorax, on the other hand, is due to a force causing penetration into the pleural cavity. This can be due to iatrogenic or non-iatrogenic causes. Iatrogenic causes include mechanical ventilation, thoracocentesis. Pacemaker insertion, tracheostomy. Non-iatrogenic causes are due to external force which results in a chest wall defect allowing external air to enter the pleural space.
Our patient had a spontaneous pneumothorax in the setting of a recent diagnosis of COVID-19 infection. He was a non-smoker, with no known past medical history of lung disease and no evidence of blebs of bullae on chest imaging. Additionally, his oxygenation demands were adequately supported with HFNC and did not require up titration to mechanical ventilation. Patient did not suffer any trauma with his near syncopal episode prior to his pneumothorax. The cause of his pneumothorax can only be associated with a recent COVID-19 diagnosis [1].
The largest series of pneumothoraces in nonventilated patients with COVID-19 were described in a multicentre retrospective case series by Martinell [2]. which reported pneumothorax to be more prevalent in males, especially those who were affected with severe form of COVID-19. Additionally, pneumothorax has been associated with a poor prognostic marker previously. However, in the case series, the patients with pneumothorax had an overall survival of 63.1% which aligns with our patient’s response to his pneumothorax & his survival from this complication.
According to a retrospective review of COVID-19 patients by Zantah which reviewed 902 COVID-19 positive patients, only six cases developed a spontaneous pneumothorax. Out of those, four required mechanical ventilation & all six cases required a chest tube placement. The incidence of mechanical ventilation causing pneumothorax is high secondary to the barotrauma and volutrauma causing overdistention of the alveoli. Our patient not requiring any mechanical ventilation rules out barotrauma and volutrauma as a predisposing factor for his pneumothorax [3-6].
Conclusion
Spontaneous pneumothorax is a rare but serious complication of COVID-19. This case brings to surface a complication of COVID-19 which has been reported scarcely in literature. There have been very few cases of spontaneous pneumothorax in association with COVID-19 without any predisposing factors. It is essential that the medical community consider pneumothorax when presented with a sudden respiratory decompensation is observed in COVID-19 patients, even in the absence of mechanical ventilation.
References
- Chen X, Zhang G, Tang Y, Peng Z, Pan H (2020) The coronavirus diseases 2019 (COVID-19) pneumonia with spontaneous pneumothorax: a case report. BMC Infect Dis 20:662
[Crossref] [Google scholar] [Indexed]
- Martinelli AW, Ingle T, Newman J, Nadeem I, Jackson K, et al. (2020) COVID-19 and pneumothorax: a multicentre retrospective case series. Eur Respir J 56:2002697
[Crossref] [Google scholar] [Indexed]
- Zantah M, Dominguez Castillo E, Townsend R, Dikengil F, et al. (2020) Pneumothorax in COVID-19 disease- incidence and clinical characteristics. Respir Res 21:236
[Crossref] [Google scholar] [Indexed]
- Kircher LT, Swartzel RL. (1954) Spontaneous pneumothorax and its treatment. J Am Med Assoc 155(1):24-29.
[Crossref] [Google scholar] [Indexed]
- Le TT, Andreadakis Z, Kumar A, Román RG, Tollefsen S, Saville M, et al. (2020) The COVID-19 vaccine development landscape. Nat Rev Drug Discov 19(5):305-6.
[Crossref] [Google scholar] [Indexed]
- Tschopp JM, Rami-Porta R, Noppen M, Astoul P. (2006) Management of spontaneous pneumothorax: state of the art. Eur Respir J 28(3):637-650
[Crossref] [Google scholar] [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences